Abstract
Understanding the role of therapeutic process factors in treatment change may prove useful for discerning why some autistic youth benefit from psychosocial interventions that target emotional and psychological aspects of mental health, while others do not. The aim of the current study was to synthesize what is currently known about therapeutic process factors in mental health treatment of emotional and psychological challenges for autistic youth, regarding how process factors have been measured in past research, and the relation between process factors and treatment outcome. A systematic review of the literature was conducted to narratively synthesize all articles published up until June 2021. Methodological quality of included studies was appraised. Twenty-five studies met inclusion criteria. Process factors assessed across studies included relational factors; treatment expectations, readiness, and satisfaction; and treatment engagement from youth and their parents. Process-outcome associations were reported for a limited number of constructs. There is a limited, albeit growing, body of high-quality research evaluating the role of process factors in the treatment of mental health issues for autistic youth. Future research should continue to examine process factors in relation to treatment outcome, and validate measures to accurately capture process-related constructs in mental health treatment for this population. Greater understanding of therapy processes can lead to developing evidence-informed strategies that clinicians can implement to promote positive expectations, relationships, and engagement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Autistic children and adolescents often experience emotional and psychological challenges related to mental health, such as anxiety, mood, and associated behavioural problems (Lai et al., 2019; Salazar et al., 2015). These mental health issues may be attributed in part to a limited capacity to regulate emotions (Mazefsky & White, 2014; Weiss, 2014) and can manifest as tantrums or meltdowns, self-injurious behaviour, or aggression towards others. In addition to the occurrence of sub-clinical mental health challenges, approximately 70% of autistic youthFootnote 1 are estimated to meet criteria for at least one psychiatric disorder (Mattila et al., 2010; Simonoff et al., 2008), with even higher rates reported for youth receiving mental health services (Brookman-Frazee et al., 2018).
There is emerging evidence supporting the use of psychosocial interventions to address mental health challenges for verbally able autistic youth. Cognitive behaviour therapy (CBT) is the most well-researched intervention to date and has largely focused on reducing anxiety-related symptoms (Ameis et al., 2018; Weston et al., 2016). Recent research suggests CBT may also be useful in promoting emotion regulation skills (Weiss et al., 2018). Early-stage research on other psychosocial treatments, such as mindfulness-based interventions, also show promise for promoting psychological well-being in young autistic people (Hartley et al., 2019). Nonetheless, a notable portion of autistic children who take part in psychosocial interventions do not exhibit clinically meaningful improvements upon therapy completion (e.g., Wood et al., 2009, 2020). For example, a systematic review of anxiety treatment for autistic youth indicated that up to 71% of youth responded to CBT; in other words, at minimum, almost one-third of those who participated in therapy did not demonstrate clinically significant improvement (Vasa et al., 2014). Additionally, meta-analytic results indicate that only 23% of autistic youth who participate in CBT show complete recovery from anxiety symptoms (Warwick et al., 2017). Beyond anxiety, it has been shown that approximately half of autistic youth receiving modified CBT for obsessive–compulsive symptoms do not show meaningful improvement at the end of treatment (Jassi et al., 2021), and one-third have been deemed non-responders in regard to changes in emotion regulation (Swain et al., 2019). Understanding the specific factors that contribute to treatment success may prove useful for discerning who benefits from treatment and why, and could potentially lead to enhanced treatment effectiveness for youth who are particularly susceptible to mental health challenges.
Common therapeutic factors may play a role in some of the variation observed in mental health outcomes for autistic youth who take part in psychosocial interventions. The common factor approach recognizes the importance of therapy-specific techniques for effecting change (e.g., thought records or behavioural activation in CBT), but also emphasizes the influence of factors that are common across therapeutic modalities (Thomas, 2006). For example, client pre-treatment characteristics, such as symptom severity, expectations about therapy, or developmental level, are believed to impact the therapeutic process, regardless of the type of therapy (e.g., CBT, psychodynamic; Karver et al., 2005). Process factors are a subgroup of common factors that broadly refer to universal aspects of treatment, which unfold from moment to moment over the course of therapy (Orlinsky, 2001). At the individual level, these factors may include client behaviour within treatment sessions, such as the quality of participation in-session tasks, and outside the therapy environment, such as adherence to at-home skill practice. The therapeutic process may be influenced by pre-treatment factors that evolve and become part of the therapy process, such as treatment expectation or willingness to participate. Interpersonal factors, such as the working relationship between the client and therapist, known as the therapeutic alliance, or parental scaffolding during home practice (in the case of child-focused therapies) may also affect the therapy process. Process factors are believed to contribute to symptom change, beyond unique technical elements of any specific therapeutic modality (Brown, 2015; Sprenkle & Blow, 2004).
There is a growing interest in process-related factors within the field of youth-focused therapy. Over the past two decades, several reviews and meta-analyses have been conducted to summarize process-related constructs in association with youth treatment outcome (Becker et al., 2018; Fjermestad et al., 2009; Karver et al., 2006, 2018; Kazantzis et al., 2016). Process factors that have been assessed in the youth treatment literature include therapeutic alliance with both youth and parent, youth and parent willingness to participate in treatment, youth and parent involvement, as well as therapist-specific factors, such as use of self-disclosure, therapist experience, and perceived competency. Relationship factors are the most well-understood process factor in the youth literature outside of autism-related research. The latest meta-analytic review (Karver et al., 2018) identified 28 studies examining the association between therapeutic alliance and treatment outcome, which yielded an overall moderate-sized effect—in line with previous alliance-outcome associations observed in youth-focused therapies (Karver et al., 2006; Shirk & Karver, 2011). Several studies have also examined youth treatment expectations and motivation to participate in therapy, which have been shown to predict whether youth complete treatment or terminate early, and which are positively related to symptom reduction in mental health-related outcomes (Adelman et al., 1984; Dew-Reeves & Athay, 2012; Lewin et al., 2011; Wergeland et al., 2015). Treatment engagement (interchangeably referred to as “involvement” or “participation”) encompasses participation both within and outside of therapy sessions. Based on findings from 13 studies, meta-analysis of in-session participation and treatment adherence (i.e., homework completion) in the youth treatment literature indicated an overall moderate-sized association between child participation and treatment outcome (Karver et al., 2006).
In addition to youth-focused process factors, numerous studies have examined parent-focused factors that may contribute to therapeutic change. Parents’ willingness to participate in their children’s treatment has been found to be a moderate-sized predictor of youth improvement (Karver et al., 2006). Therapeutic alliance between parents and therapist, and parent participation in and out of sessions, predicts a small portion of variance in youth mental health outcomes (Karver et al., 2006; McLeod, 2011). Across youth and parent-related process factors, small to moderate-sized effects have been reported for process-outcome associations within the youth treatment literature (Karver et al., 2006, 2018).
Findings from existing studies largely apply to youth treatment in general and have often failed to specify whether any of the included research involved autistic youth. It is unclear whether similar effect sizes are observed, or whether process factors can be validly and reliably measured in the context of therapy for this population. It is plausible that the therapeutic process unfolds differently for autistic youth, relative to peers without autism, because of common difficulties with social-communication and restrictive patterns of thinking, as well frequent co-occurring challenges, like inattention, executive dysfunction, and oppositionality (Demetriou et al., 2018; Salazar et al., 2015). For example, therapeutic alliance may have a disparate relation to treatment outcome for youth who struggle with social relationships. Given how commonly occurring mental health problems are (Lai et al., 2019) and the marked portion of autistic youth who do not improve from psychotherapy (e.g., Vasa et al., 2014), it is important to establish a strong knowledge base on addressable factors that can contribute to therapeutic success for this population. The aim of the current study was to synthesize what is currently known about therapeutic process factors in mental health treatment for autistic youth, in regard to how process factors have been measured in past research, and the relation between process factors and treatment outcome.
Method
Search Strategy
A systematic review of empirical research examining process factors in mental health treatment for autistic youth was conducted in accordance with the standards described by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA; Moher et al., 2009) guidelines. The review protocol was prospectively registered with the PROSPERO international review database (ID: CRD42021240272; https://www.crd.york.ac.uk/prospero/). A concurrent search of Ovid MEDLINE, PubMed, and PsycINFO was conducted on June 7, 2021 to identify all articles published to date. The final search strategy is provided in Supplemental Table 1. Based on the previous review of therapeutic process factors completed by Karver et al. (2006), 29 process-related search terms were selected. The search strategy also included autism-related terms (i.e., autis*, Asperger syndrome) and terms describing youth age range (i.e., child*, pediatric, youth, adolescen*, and kid), which were combined with the process-related terms. When possible, terms were modified to align with database-specific index terms (e.g., MeSH terms for PubMed).
Selection Criteria
Studies identified through the searches were included based on the following criteria: (a) evaluated or described a psychosocial intervention addressing an emotional or psychological mental health-related outcome (as either a primary or secondary outcome; e.g., anxiety, depression); (b) at least a portion of the sample included youth under the age of 18 years, with a previous diagnosis of autism or related disorder (e.g., Asperger syndrome); (c) assessed and/or described at least one process-related factor; and (d) was available in English. Exclusion criteria were: (a) interventions addressing disruptive behaviour only (e.g., opposition, defiance, conduct problems) without consideration of the emotional and psychological aspects of mental health; (b) non-empirical publications (e.g., editorials, commentaries, books, book chapters, theoretical papers); (c) reviews or meta-analyses; and (d) unpublished dissertations or theses. Notably, there is a large body of literature (e.g., studies evaluating applied behavioural interventions) that has focused on reducing “disruptive” behaviours (e.g., self-injurious behaviour; aggression towards others) without evaluating the role of internalized emotional and psychological experiences (e.g., anxiety, depression, emotion regulation) that may explain the observable behaviour. Although it is not uncommon for autistic youth to demonstrate disruptive behaviour that stems from emotional and psychological issues, it is uncertain whether these problems are a targeted treatment outcome of an intervention when there is a lack of direct measurement. For clarity and consistency, the decision was made to focus on studies that explicitly assessed emotional and psychological outcomes related to mental health.
To identify eligible studies, all titles and abstracts of articles retrieved through database searches were independently screened by two authors (CA and NV). For the screening phase, disagreements were resolved through discussion until consensus was reached between the two authors. All articles that underwent full-text review were also independently reviewed by each author. Disagreements for full-text review were resolved through discussion and consultation with the senior author (JW).
Quality Appraisal of Included Studies
The Mixed Methods Analysis Tool (MMAT; Hong et al., 2018) was used to assess the methodological quality of studies that met inclusion criteria, which was developed for empirical studies based on the study design. To determine whether a study is considered empirical, reviewers respond “Yes” or “No” to two screening questions regarding clarity of research questions and adequacy of data collection for addressing research questions. For studies that fail to meet screening criteria, quality appraisal is not conducted. For articles that meet screening criteria, reviewers respond “Yes” or “No” to five methodological-related questions that vary depending on study design (e.g., qualitative vs. randomized controlled trial). If there is insufficient information provided in the article to answer the question, reviewers may respond with “Can’t Tell”. As per the MMAT guidelines (Hong et al., 2018), methodological quality of each study is considered based on responses to individual criterion, versus a global rating or overall score. Included studies were assessed by one of two reviewers (CA or NV), and approximately 30% of studies (n = 8) were coded by the other reviewer as a reliability check. Reviewers were recused from rating articles that they authored. There was substantial agreement across raters (Fleiss κ = 0.77). Disagreements in ratings were resolved through discussion. The MMAT has been used as a quality appraisal tool in other review studies focused on developmental disabilities literature, including autism (Albaum et al., 2021; Doherty et al., 2020).
Results
Search Results
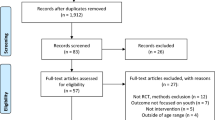
Search results are illustrated in Fig. 1. An initial search of the databases using the search strategy described above yielded 6,409 articles. After duplicate articles were removed, 4,994 articles remained for review. The two authors screening titles and abstracts agreed on whether studies should be excluded or undergo full-text review for 97% of articles (n = 4849 articles). Title and abstract screening resulted in 4,898 articles being excluded. The full-text for the remaining 96 articles were again reviewed by both authors. Authors agreed regarding eligibility for 82% of articles (n = 79). Full-text review resulted in an additional 74 articles being excluded (see Fig. 1 for exclusion reasons), leaving 22 articles for data extraction and synthesis. Reference lists from included articles were reviewed for potentially relevant studies that were not identified in the original search, which resulted in inclusion of three additional studies (Brown et al., 2015; Jassi et al., 2021; White et al., 2013).
Study Characteristics
Study characteristics are detailed in Table 1, including study location, study design, sample characteristics, description of intervention, mental health outcomes, and process factors identified. Twenty-five studies derived from 21 unique samples were identified; four of the included articles utilized the same sample (Albaum et al., 2020; Burnham Riosa et al., 2019; Thomson et al., 2015; Weiss et al., 2018). Although there was no lower date bound set for inclusion criteria, all studies identified through the search were published from 2012 onwards, with 68% of studies (n = 17) being published within the past six years (i.e., after 2015). Of the 25 included studies, 64% (n = 16) were conducted in North America and 28% (n = 7) in Europe; one study occurred in Asia, and one study occurred in Australia. In terms of study design, most studies were quantitative-descriptive in nature (36%, n = 9). Five studies (20%) conducted quantitative, non-randomized intervention trials, and five studies were randomized controlled trials. Three studies (12%) employed qualitative designs, and the remaining three studies used a mixed methods approach, involving quantitative and qualitative methods.
Across studies, participants ranged in age from 4 to 29 years. Nine studies (36%) involved adolescents (i.e., 13 years of age or older) and nine included both children and adolescents; five studies (20%) included children only (i.e., 12 years of age or younger), and two did not report on the age range of the sample. The mean age reported across studies was 12.6 years (SD = 3.41; range: 6.2 to 20.6). On average, samples comprised 82.3% males (SD = 13.2%, range: 43% to 100%). Sixteen studies (64%) reported that the majority of participants in the sample identified as White/Caucasian, 11 of which included samples with more than 75% White/Caucasian participants; one study sample comprised 100% Asian participants (i.e., Chinese, Indian, or Malays; Drmic et al., 2017), and one study comprised 100% Latinx participants (Chlebowski et al., 2018). Seven studies (28%) did not report on the ethnicity or racial identity of participants. Most studies (80%, n = 20) reported using autism diagnostic (e.g., ADOS; ADI-R) and/or screening tools (e.g., SCQ; SRS-2), or having participants share a report from a licensed healthcare provider to confirm autism diagnostic criteria were met. The majority of studies excluded participants with a diagnosed intellectual disability or who had limited intellectual abilities (e.g., IQ < 70; 76%, n = 19); five studies (20%) did not specify level of intellectual functioning. One study included a single participant with an intellectual disability, as reported by parents (London et al., 2020).
Regarding the interventions, the majority of studies (64%, n = 16) involved treatment programs that were based on CBT. Other forms of psychosocial treatment included psychoeducation (Backman et al., 2018; Gordon et al., 2015), social skills interventions (Kang et al., 2021; Lordo et al., 2017; White et al., 2013), mindfulness-based interventions (Brewe et al., 2021; Pahnke et al., 2014), counselling or psychotherapy (Brown et al., 2015; Chlebowski et al., 2018), music programs (Hillier et al., 2012), and animal-assisted occupational therapy (London et al., 2020). Fifteen studies (60%) involved individualized treatment and 36% (n = 9) used group formats; one study involved a combination of individual and group sessions (White et al., 2013). Parents were fully involved in treatment (i.e., were present for the entire duration of all sessions) in 40% of studies (n = 10), and partially involved for another 40% of studies (e.g., present for only a portion of each session; attended some, but not all sessions; participated in parallel parent-only sessions). For 20% of studies (n = 5), the extent of parent involvement was not reported. Mental health outcomes that were commonly targeted included anxiety (60% of studies, n = 15), emotion regulation (28%, n = 7), internalizing and externalizing symptoms broadly (16%, n = 4), depression (8%, n = 2), and obsessive–compulsive symptoms (8%, n = 2). Studies also examined other mental health-related outcomes such as general psychopathology and psychiatric comorbidity, psychological distress and stress-related behaviour, emotional and behaviour problems, positive and negative affect, and self-esteem.
Quality of Included Studies
Study quality was appraised using the MMAT (Hong et al., 2018). All studies were deemed to have clear research questions and collected appropriate data to address the research questions, and thus met MMAT screening criteria to proceed for further appraisal. Eight studies (32%) met 100% of the MMAT criteria for the respective study design; 10 studies (40%) met 80% of criteria; four studies (16%) met 60% of criteria; one study (4%) met 40% of criteria; and two studies (8%) met 20% of criteria. Summary of responses to questions regarding methodological quality are provided in Table 2.
Process Factors Assessed in Quantitative Studies
Among studies that employed quantitative methods (n = 22; including randomized and non-randomized, descriptive, and mixed methods designs), the following process factors were identified: family accommodation, parent-therapist alliance, treatment adherence, treatment expectations, treatment readiness, treatment satisfaction, youth involvement, and youth-therapist alliance. Details regarding the measures used to assess each process factor are provided in Table 3. As shown in Table 1, approximately 62% of studies described process factors as indicators of treatment feasibility, without examining process-outcome associations. For example, several studies described homework completion as an indication of treatment adherence (e.g., McNally Keehn et al., 2013; Thomson et al., 2015), but did not report correlations between homework completion and treatment outcome. Eight studies explicitly evaluated the relation between process factors and treatment outcome, and six studies assessed relations among process factors. An overview of study results for each process factor follows below.
Family Accommodation
Family accommodation is described as the tendency for family members to engage in behaviours that aim to prevent the child from experiencing anxiety or aid the child in avoiding anxiety-provoking stimuli (Lebowitz et al., 2012), such as providing unnecessary reassurance or adapting routines to intentionally avoid situations that cause anxiety (Lebowitz et al., 2014). Three studies measured family accommodation of youth anxiety or obsessive–compulsive symptoms (Jassi et al., 2021; Jones & Jassi, 2020; Storch et al., 2015) using two different parent-report measures (details provided in Table 3). All three studies assessed family accommodation pre- and post-treatment, and two studies also assessed family accommodation at multiple timepoints during, and three-months following the end of treatment (Jassi et al., 2021; Jones & Jassi, 2020). All three studies cite evidence for the valid use of the selected measures based on previous research involving youth without autism; however, psychometric properties (e.g., metric of internal consistency) based on the study sample were not reported in any of the studies.
Only one of these studies considered family accommodation in relation to treatment outcome. Storch et al. (2015) assessed parent accommodation of youth anxiety symptoms prior to and following participation in CBT. In comparison to those considered non-responders, families of youth who responded to treatment had a lower frequency of symptom accommodation at the end of treatment, and accommodation had less of an impact on parents’ activities and work schedules, family routine, and family distress. There was no significant difference between responders and non-responders in terms of the impact of accommodation on youth treatment outcomes. Family accommodation was the only process factor measured in this study, and thus could not be examined in relation to other process factors. Jassi et al. (2021) reported clinically elevated levels of family accommodation at baseline, which significantly improved by the end of treatment, with changes maintained at 3-month follow-up. However, the authors did not examine the relation between reduction in family accommodation and reduction in OCD symptoms found at post-treatment. Similarly, in their case study of an autistic adolescent receiving modified CBT for treatment-resistant OCD, Jones and Jassi (2020) noted improvements in family accommodation and OCD symptoms, but did not assess the association between the two variables.
Parent-Therapist Alliance
Four studies examined therapeutic alliance between parents and therapists; three of these studies assessed parent-therapist alliance at multiple points during treatment (Burnham Riosa et al., 2019; Klebanoff et al., 2019; Thomson et al., 2015), and one measured alliance post-treatment (Kerns et al., 2018). Two studies used the parent-report Therapeutic Alliance Scale for Children, Revised (TASC-R; Shirk & Saiz, 1992) as a measure of alliance, with one reporting adequate internal consistency among scale items (Kerns et al., 2018). Two other studies (derived from the same larger clinical trial; Weiss et al., 2018) relied on therapist-report using a single-item (Burnham Riosa et al., 2019; Thomson et al., 2015). Burnham Riosa et al. (2019) also used the Therapy Process Observational Coding Scheme, Alliance scale (TPOCS-A; McLeod & Weisz, 2005) for independent-observer ratings of parent-therapist alliance, which strongly converged with the single-item therapist ratings. The authors reported good to excellent inter-rater reliability across items, and acceptable to good internal consistencies for TPOCS-A subscales.
Two studies examined therapeutic alliance between parents and therapists, in association with child treatment outcomes. Klebanoff et al. (2019) found parent-therapist alliance, as reported by parents, predicted greater reduction in child anxiety severity post-treatment, with a stronger alliance-outcome correlation for older children (i.e., 10 years or older) compared to younger children (i.e., under 10 years). In contrast, Kerns et al. (2018) did not find a significant relation between parent-therapist alliance and improvements in child anxiety following treatment, nor did they find a difference in parent-therapist alliance between treatment responders and non-responders. In terms of the relation among process factors, Klebanoff et al. (2019) found a moderate correlation between parent-therapist alliance and therapist-reported alliance with youth, whereas Kerns et al. (2018) did not find a significant association. Other studies aimed to examine the psychometric properties of therapeutic alliance measures (Burnham Riosa et al., 2019) or included parent-therapist alliance as an indicator of treatment feasibility (Thomson et al., 2015), and did not report on process-outcome or process-process correlations.
Treatment Satisfaction
Treatment satisfaction has not been consistently operationalized, but generally refers to the perceived helpfulness, enjoyment, and/or acceptability of treatment. Treatment satisfaction was the most commonly reported process factor in included studies. Four studies had participants provide ratings of treatment satisfaction following each session, and five studies included a single satisfaction rating provided at the end of treatment. Treatment satisfaction was rated by youth, parents, and/or therapists, with four studies involving a single informant (Backman et al., 2018; Gordon et al., 2015; Pahnke et al., 2014; Swain et al., 2019), and six studies involving multiple informants (Hillier et al., 2012; Jassi et al., 2021; Thomson et al., 2015; Walsh et al., 2018; Weiss et al., 2018; White et al., 2013). Measures were typically developed to assess satisfaction for the specific
intervention program being delivered, and thus tended to vary across studies. None of the studies reported on psychometric properties of treatment satisfaction measures.
The majority of studies that reported on treatment satisfaction did not describe process-outcome or process-process associations, but reported on satisfaction as an indication of treatment feasibility. In general, participants reported being satisfied with the treatment they received. Only two studies measured the relation between treatment satisfaction and mental health outcomes. Walsh et al. (2018) examined the association between youth and parent ratings of treatment acceptability, and improvements in anxiety following participation in CBT. The authors found that for sessions focused on exposure to anxiety-provoking stimuli, acceptability ratings from both parent and youth respondents negatively predicted anxiety severity following treatment. For sessions that focused on psychoeducation, neither parent nor youth ratings of acceptability predicted treatment outcome. Across all sessions, parents indicated greater satisfaction with treatment compared to youth. Swain et al. (2019) also assessed satisfaction in treatment targeting emotional problems and emotion regulation, and found that treatment satisfaction did not differ between treatment responders and non-responders.
Youth-Therapist Alliance
Eight studies measured therapeutic alliance between therapists and youth; six of which measured alliance at multiple time points during treatment, one which measured at one point during treatment (Brown et al., 2015), and one which measured post-treatment (Kerns et al., 2018). Four studies used independent-observer ratings based on the TPOCS-A (McLeod & Weisz, 2005), which collectively reported good to excellent inter-rater reliability across items (Albaum et al., 2020; Brown et al., 2015; Burnham Riosa et al., 2019; Kang et al., 2021), good to excellent internal consistencies across subscales (Albaum et al., 2020; Burnham Riosa et al., 2019), temporal stability of ratings (Kang et al., 2021), and strong convergence with single-item therapist ratings of alliance (Burnham Riosa et al., 2019), although no convergence with youth-rated alliance (Kang et al., 2021). Brewe et al. (2021) also relied on independent-observer reports of youth-therapist alliance based on the Vanderbilt Therapeutic Alliance Scales Revised (Shelef & Diamond, 2008), which was found to have good internal consistency and excellent interrater reliability. Three studies used therapist and/or youth reports of alliance based on the TASC-R (Shirk & Saiz, 1992), and reported good to excellent internal consistencies (Kang et al., 2021; Kerns et al., 2018; Klebanoff et al., 2019), temporal stability (Kang et al., 2021), and moderate convergence between therapist and youth ratings of alliance (Kerns et al., 2018; Klebanoff et al., 2019). The two studies derived from the same larger clinical trial also used a single-item to assess therapist ratings of youth-therapist alliance as part of a psychometric evaluation of therapeutic alliance measures (Burnham Riosa et al., 2019), or as an indicator of treatment feasibility (Thomson et al., 2015).
Five studies focused on the relation between youth-therapist alliance and treatment outcome (Albaum et al., 2020; Brewe et al., 2021; Kang et al., 2021; Kerns et al., 2018; Klebanoff et al., 2019). Across studies, there was some association between youth-therapist alliance and improvement in mental health outcomes for autistic youth following psychosocial intervention. Two studies employed measures that relied on therapist and youth reports of therapeutic alliance (Kerns et al., 2018; Klebanoff et al., 2019), which found that higher therapist ratings of youth-therapist alliance were related to greater reduction in parent- and clinician-rated youth anxiety and global symptom severity. Comparatively, results from both studies indicated that youth-reported alliance was not significantly related to treatment outcome. Kerns et al. (2018) also found that therapist-reported alliance was stronger for treatment responders compared to non-responders (categorized based on clinician-ratings of symptom improvement), but there was no significant difference between groups in terms of youth-reported alliance. These findings were consistent with results from Kang et al. (2021), who reported a non-significant association between youth-reported alliance and changes in youth self-reported social anxiety. Three studies (Albaum et al., 2020; Brewe et al., 2021; Kang et al., 2021) used measures of therapeutic alliance that relied on independent-observer ratings and found some associations with improvements in emotion regulation. Brewe et al. (2021) indicated that stronger observer-reported alliance was associated with reduced feelings of dysphoria, but not with changes in emotional reactivity, while Albaum et al. (2020) found that observer ratings of therapeutic alliance taken late in treatment, but not early, were related to improvements in parent-reported emotional lability and negativity post-treatment. However, observer-reported alliance did not predict youth-reported treatment outcomes (Albaum et al., 2020; Kang et al., 2021). Two studies further examined specific components of therapeutic alliance relative to treatment outcomes with mixed results; findings from Albaum et al. (2020) indicated task-collaboration, but not therapeutic bond, was a significant predictor of treatment outcome, while Klebanoff et al. (2019) found that bond predicted treatment outcome, but agreement on therapeutic tasks did not. Notably, the two studies differed in terms of reporting source (i.e., therapist-report vs. independent-observer) and the mental health outcome assessed (i.e., anxiety and global symptom severity vs. emotion dysregulation). Two other studies reported on associations between youth-therapist alliance and other process factors. Observer-reported alliance was not related to pre-treatment youth ratings of treatment readiness (Albaum et al., 2020). Burnham Riosa et al. (2019) found moderate to strong correlations between observer ratings of alliance and therapist-rated treatment adherence (i.e., homework completion) and youth involvement in therapy sessions.
Youth Treatment Engagement
Eight studies assessed different aspects of treatment engagement, none of which examined associations between engagement and outcome. All eight studies described indicators of treatment adherence, including rates of homework completion or between-session skills practice, and collected information regarding adherence following each therapy session. Adherence was most often rated using therapist-report on a single-item with “yes/no” or similar categorical response format (e.g., “Did the client complete the assigned homework?”). Four studies also included therapist-reported youth in-session involvement; three of which were derived from the same sample (Burnham Riosa et al., 2019; Thomson et al., 2015; Weiss et al., 2018). As with treatment adherence, in-session involvement was measured using a single-item (e.g., “How involved was the client during the session?”) completed by therapists at the end of each session. None of the included studies reported analytic results of treatment engagement beyond basic descriptive statistics (i.e., frequency; mean and SD).
Youth Treatment Expectations
Treatment expectation was assessed in one study (Backman et al., 2018), which measured adolescents’ perceptions of treatment credibility regarding the autism-specific psychoeducation program being provided. The authors did not examine the relation between treatment credibility and mental health outcome but found a large- sized improvement in treatment credibility from pre- to post-intervention (η2 = 0.30). Psychometric information about the measure used to assess treatment credibility was not provided.
Youth Treatment Readiness
One study included a measure of youth treatment readiness (Albaum et al., 2020), which was assessed pre-treatment using three items that asked children to rate their interest, readiness, and willingness to participate in therapy. The authors examined the association between treatment readiness and youth-therapist alliance both early (i.e., first half) and late (i.e., second half) in treatment, and found no significant relation. Psychometric information of validity and reliability were not provided, and the authors did not evaluate treatment readiness in relation to outcome.
Process Factors Described in Qualitative Studies
Four of the included studies conducted qualitative analyses to evaluate participants’ experiences with mental health interventions (Chlebowski et al., 2018; Drmic et al., 2017; Edgington et al., 2016; London et al., 2020), which resulted in several emerging themes of process-related factors. Three studies identified themes related to parent involvement in mental health treatment for autistic youth. For example, strong, consistent support from stakeholders (including parents), such as parent enthusiasm for their child’s treatment, was described as an important factor for facilitating and implementing CBT for anxiety in autistic adolescents (Drmic et al., 2020). Themes related to challenges with parent involvement also emerged, such as difficulties with obtaining information from adolescents when parents are not directly involved in treatment (Edgington et al., 2016), and different perceptions between therapists and parents in terms of the expected role parents play in mental health treatment for children (e.g., expecting child to take part in sessions independently, without parent involvement; Chlebowski et al., 2018). Youth motivation was a relevant theme in considering the feasibility of implementing an intervention program, and participants’ acceptability and skill application. Identifying motivated adolescents to participate in treatment was important for establishing positive rapport and facilitating enjoyable sessions (Drmic et al., 2020), and self-motivation was relevant for unprompted use of coping strategies (Edgington et al., 2016). Relatedly, a lack of readiness from adolescents to participate in groups was described as a barrier for coaches to facilitate sessions smoothly (Drmic et al., 2020). Other process factors that were mentioned in qualitative themes included group cohesion (e.g., importance of group dynamics; Edgington et al., 2016), therapist direct influence skills (e.g., ability to carry out program delivery; Drmic et al., 2020), the relationship between parents and therapists (Chlebowski et al., 2018), and youth engagement in relation to treatment progress (London et al., 2020).
Discussion
Therapeutic process factors are known predictors of treatment outcome and may serve as mechanisms for fostering change in psychosocial interventions. Research evaluating process factors has largely involved youth without autism, restricting the generalizability of findings to interventions that target mental health concerns for autistic children and adolescents. The current literature search yielded 25 studies that involved autistic youth (i.e., under 18 years of age) who took part in psychosocial interventions to address the emotional and psychological aspects of mental health issues, such as anxiety, depression, or related challenges (e.g., emotion dysregulation, stress-related behaviour). Across studies, various factors were described or assessed that can be classified into three overarching domains: relational factors (e.g., therapeutic alliance); expectations, readiness, and satisfaction; and treatment engagement (e.g., involvement; adherence).
Relational Factors
Relational factors comprise constructs that describe different aspects of the relationships between therapists, clients, and caregivers, both within and outside therapy sessions. Consistent with the non-autism literature (Fjermestad et al., 2009; Karver et al., 2006), relational factors appear to be the most well-understood aspect of the therapeutic process in mental health treatment for autistic youth. Several studies examined therapeutic alliance between therapists and autistic youth. Therapeutic alliance refers to the working relationship between therapist and client, based on bond, collaboration on therapeutic tasks, and agreed upon treatment goals (Bordin, 1979). Preliminary psychometric evidence suggests that youth-therapist alliance can be validly assessed through different informants (e.g., youth, therapist, independent-observer) at multiple points during treatment, making it possible to conduct longitudinal analyses using multiple perspectives. Within the general child literature, variation in alliance-outcome associations has been attributed in part to reporting source (e.g., youth vs. therapist; Karver et al., 2018). Researchers should, therefore, consider incorporating measures that rely on multiple perspectives when evaluating alliance with autistic clients to help determine the predictive validity of ratings provided by different informants. Findings across studies indicate that it is not only possible for clinicians to form a strong working relationship, but that therapeutic alliance may be an important contributor to improvements in anxiety (Kerns et al., 2018; Klebanoff et al., 2019) and emotion regulation (Albaum et al., 2020; Brewe et al., 2021) for autistic children and adolescents. Therapeutic alliance with autistic youth was also found to be positively associated with youth involvement during therapy sessions, and treatment adherence outside of sessions (Burnham Riosa et al., 2019), though further research is needed to understand the transactional pattern that occurs between these factors over the course of therapy. Given the inherent social-communication challenges associated with autism that can make it difficult for youth to form meaningful relationships, it is critical to consider therapist factors that may contribute to establishing and maintaining alliance with these clients. For example, clinicians’ lack of knowledge and experience, poor competence, and low confidence about working with autistic adults have been identified as barriers to treatment for these clients (Maddox et al., 2020). A recent study also found that therapists are less likely to treat autistic youth compared to youth with ADHD, which was partly explained by differences in therapist attitudes about working with each population, their knowledge about mental health for autistic clients, and the normative pressures they felt about treating autistic youth (Roudbarani et al., in press). In light of the association between therapist attitudes and intention to treat, and the proposed theoretical connection between therapist attitudes and process factors (Karver et al., 2005), it is important to evaluate how these attitudes may influence relational aspects of the therapeutic process that are relevant for treatment outcome. For instance, researchers may aim to answer questions such as: Do more favourable therapist attitudes predict stronger therapeutic alliance? Does the formation of therapeutic alliance strengthen therapist attitudes about working with autistic clients? Are more favourable therapist attitudes related to greater improvement in treatment outcome, and is this association mediated by the quality of therapeutic alliance? Addressing these research questions may involve assessing therapist attitudes prior to beginning therapy, and then repeatedly measuring attitudes and therapeutic alliance over the course of treatment to determine whether there is a shift in therapist attitudes, and if there is bidirectional link between attitudes and alliance. In addition, therapists may find it beneficial to have youth and parents complete brief measures of therapeutic alliance (e.g., TASC-R) to monitor their perspectives on the relationship, and then actively work to strengthen the relationship with autistic clients by addressing areas of concern that have been indicated.
Review findings suggest that family accommodation may also be a relevant relational factor to consider when addressing mental health concerns with this population. Family accommodation refers to parent and other family members’ behaviour that abets the child in avoiding anxiety-inducing experiences (Lebowitz et al., 2012, 2014). Previous reviews of the general child literature (e.g., Karver et al., 2006) have not considered family accommodation as part of the therapy process, though it may be a pertinent factor to consider when parents and family members are involved in a child’s treatment. For youth without autism, family accommodation is positively related to child anxiety levels, and reductions in family accommodation have been linked to greater symptom improvement (Lebowitz et al., 2014; Merlo et al., 2009). Three studies identified through the review indicated progressive reduction in parent-reported family accommodation over the course of therapy (Jassi et al., 2021; Jones & Jassi, 2020; Storch et al., 2015), with one study finding a negative association between family accommodation and treatment response (i.e., treatment responders reported lower levels of accommodation compared to non-responders; Storch et al., 2015). Shifts in family accommodation may be particularly relevant to the therapeutic process when parents are involved in their child’s treatment, as is often the case for autistic youth (Reaven, 2011). However, based on literature currently available, it is still unclear whether changes in family accommodation are related to changes in mental health outcomes, and if family accommodation is associated with other aspects of the therapeutic process, such as parent-therapist alliance or parent beliefs about treatment.
Expectations, Readiness and Satisfaction
Client expectations regarding the efficacy, relevance, and importance of treatment, as well as their readiness or motivation to participate, are thought to be key factors related to treatment attendance and adherence (Karver et al., 2005; King et al., 2014). Although treatment expectations have been considered pre-treatment characteristics (Karver et al., 2005), evidence from the current review suggests that beliefs about treatment may not necessarily be fixed, as Backman et al. (2018) found that participants’ perceptions of treatment credibility shifted over the course of therapy. Within the context of interventions for children and adolescents without autism, both youth and parent expectations and readiness may have a dynamic association with treatment participation, in turn influencing therapeutic outcome (Karver et al., 2006). Minimal research has explored these processes for autistic youth, either in terms of construct validity or treatment outcome. None of the studies identified in the review assessed parent expectations and willingness to participate in their child’s treatment. Qualitative analyses indicate that youth motivation may be relevant to therapist capacity to establish rapport and facilitate sessions, and treatment adherence on the part of the youth outside of therapy sessions. Parent expectations regarding their role in their child’s treatment was also described as pertinent to the provision of mental health treatment for autistic adolescents (Chlebowski et al., 2018). As noted above, Backman et al. (2018) quantitatively assessed youth perceptions of treatment credibility during the receipt of psychoeducation about autism, and found that perceived credibility improved over the course of the intervention. However, the authors did not examine whether credibility was associated with changes in youth anxiety or depression. Similarly, a second study assessed children’s readiness and willingness to take part in treatment prior to participating in CBT and found a non-significant relation between treatment readiness and child-therapist alliance (Albaum et al., 2020). The authors reported a considerable range in the degree of child readiness across participants, suggesting that autistic youth who take part in mental health intervention likely vary in their willingness and commitment to participate; however, they did not assess the association between treatment readiness and changes in mental health outcomes following treatment completion. Thus, there is a lack of empirical evidence available on the expectations autistic youth and their parents have regarding therapy, and how motivation or readiness for treatment is related to the therapy process and positive outcomes. It may be worthwhile for researchers to evaluate client beliefs about therapy prior to starting treatment, and track expectations and motivation during treatment. Findings from research of this nature could help to determine whether there are common patterns in the ways autistic clients’ beliefs about therapy change over the course of treatment, and if certain trajectories are associated with better outcomes. Establishing an evidence base on the connection between clients’ beliefs and treatment outcome could help inform adaptations to therapeutic techniques, such as motivational interviewing (Feinberg et al., 2021; Rogers et al., 2019), which can be used by clinicians to promote expectations, motivation, and treatment readiness for autistic youth and their parents.
Related to client expectations is the extent to which these expectations are met, and whether they are satisfied in their therapeutic experience, based on perceived helpfulness, relevance, and enjoyment. It has been hypothesized that treatment satisfaction may contribute to active involvement and better compliance, though the mechanistic pathway between these process-related variables is poorly understood (Karver et al., 2005). Within the autism literature, it appears that treatment satisfaction is often reported as an indicator of overall feasibility or acceptability of the intervention. Satisfaction was often analyzed descriptively, with various studies reporting high ratings of satisfaction from both parents and youth. Only two studies reported on relations between treatment satisfaction and symptom improvement (Swain et al., 2019; Walsh et al., 2018), with mixed results. Researchers who are evaluating interventions and choose to include measures of treatment satisfaction should consider exploring shifts in satisfaction that may occur throughout treatment, and possible interactions with other key therapeutic processes (e.g., compliance, adherence) that may contribute to variation in treatment effectiveness.
Treatment Engagement
Engagement in treatment is considered critical for successful outcomes (Becker et al., 2018). Within the general youth literature, the term “engagement” tends to be used interchangeably with “involvement” or “participation”, and refers to the active, effortful, and collaborative role that youth and parents have during and between therapy sessions (Karver et al., 2005). Research has yet to explore treatment engagement in relation to outcome within the context of mental health intervention for autistic youth. Several studies identified through the review provided quantitative descriptions of treatment adherence, generally operationalized as homework completion outside of sessions (e.g., Gordon et al., 2015; Pahnke et al., 2014); however, homework completion or between-session practice was typically dichotomized as “complete” or “incomplete”, failing to consider other factors, such as ease or difficulty of assigned practice, that may be relevant to the overarching construct of engagement. Youth involvement within therapy sessions was also described in several studies (e.g., Weiss et al., 2018; White et al., 2013), but relied solely on global therapist ratings on a single-item. Developing valid and reliable measures that consider nuanced behavioural indications of in-session participation can lead to greater understanding of how engagement contributes to treatment success, and can equip clinicians with the knowledge and skills needed to promote participation during sessions with autistic clients.
Parent involvement was an overarching theme in multiple studies that employed qualitative methods (Chlebowski et al., 2018; Drmic et al., 2017; Edgington et al., 2016). Direct parent involvement may be particularly important for parents to learn how to best assist their child in practicing the skills being taught (Drmic et al., 2017; Edgington et al., 2016). For younger children, parents may be expected to take on various roles in their children’s therapy, such as co-therapists. Incongruence between therapist and parent expectations about the extent of parent involvement can potentially hinder the quality of parent participation both within and outside of sessions (Chlebowski et al., 2018). Prior to beginning therapy, establishing clear, agreed upon expectations between therapists and parents about participation may augment engagement in their child’s treatment. Some studies have empirically examined therapeutic alliance between therapists and caregivers of autistic youth who participate in their children’s therapy. There is emerging support for the valid measurement of parent-therapist alliance; however, findings are inconsistent in terms of process-outcome associations. Klebanoff et al. (2019) found parent-therapist alliance was associated with greater reduction in anxiety post-treatment, whereas Kerns et al. (2018) did not find a significant process-outcome association. Given that parent involvement is a recommended modification to psychosocial intervention for autistic youth (Reaven, 2011; Walters et al., 2016), it is important to establish stronger empirical knowledge about how parents contribute to their child’s treatment success.
Limitations
Review findings should be interpreted within the context of the study’s limitations. The current review only offers a narrative synthesis of process factors; meta-analysis of effect sizes was not calculated, thus preventing comparison of potential process-outcome associations. This review only included studies published in English, and additional empirical evidence regarding process factors may be available in other languages. In regard to client characteristics, several studies included samples for which a portion of participants were over the age of 18 years (Backman et al., 2018; Brewe et al., 2021; Hillier et al., 2012; London et al., 2020; Pahnke et al., 2014), but did not conduct analyses to evaluate potential effects of age (e.g., separating < 18 vs. 18 +; including age as covariate). Samples were also limited in terms of ethnic diversity, with most studies reporting that the majority of the sample comprised participants who identified as White/Caucasian. Finally, results are based on samples that almost exclusively involve autistic youth without co-occurring intellectual disabilities and may not be equally relevant for mental health treatment for youth with limited cognitive abilities and adaptive skills.
Conclusions
There is a limited, albeit growing, body of high-quality research evaluating the role of process factors in the treatment of mental health issues for young autistic people. Researchers have begun to examine constructs related to therapeutic relationships, treatment expectations and satisfaction, and youth engagement throughout treatment, though there is still little understanding of how exactly these factors contribute to therapeutic outcomes. Future studies should continue to focus on better understood process factors, such as therapeutic alliance, and address gaps around less well-known factors, such as in-session participation and parent involvement. Specifically, researchers should examine process-outcome associations, providing metrics of effect size that can eventually be included in meta-analyses once a sufficient pool of results exists. Considering associations amongst process factors over the course of therapy, such as the youth-therapist and parent-therapist alliance, or youth and parent engagement, may also be a fruitful research direction to pursue. Further, validation of measurement tools that accurately capture process-related constructs within the context of treatment for autistic youth is necessary. It will be important for researchers to explore process factors with samples of autistic youth who represent the full spectrum of functioning in regard to social-communicative skills, and intellectual and adaptive functioning. Immediate and direct implications for clinical practice include establishing a strong therapeutic alliance with autistic youth and their parents, clarifying expectations about parent involvement in their child’s therapy, and encouraging active involvement from both youth and parents during and between therapy sessions. Greater understanding of therapy processes can provide a knowledge base that allows for evidence-informed strategies to be implemented by clinicians to promote positive expectations, relationships, and engagement. By addressing process-related barriers, therapists may be able to improve the effectiveness of mental health treatment for autistic youth.
Data Availability
Data sharing is not applicable to this article as no new data were created and no datasets were generated or analysed during the current study. Additional information is available from the corresponding author upon request.
Notes
The term “youth” is used here to describe young people under the age of 18 years. “Children” refers to youth 12 years of age and younger, and “adolescents” refers to youth between 13 and 17 years of age.
References
Articles included in systematic review marked with asterisk
Adelman, H. S., Kaser-Boyd, N., & Taylor, L. (1984). Children’s participation in consent for psychotherapy and their subsequent response to treatment. Journal of Clinical Child & Adolescent Psychology, 13(2), 170–178. https://doi.org/10.1080/15374418409533186
Albaum, C., Chan, V., Sellitto, T., Vashi, N., Hastings, R. P., & Weiss, J. A. (2021). Redressing the balance: A systematic review of positive psychology in the intellectual disability literature. International Review of Research in Developmental Disabilities, 60, 1–53. https://doi.org/10.1016/bs.irrdd.2021.08.003
*Albaum, C., Tablon, P., Roudbarani, F., & Weiss, J. A. (2020). Predictors and outcomes associated with therapeutic alliance in cognitive behaviour therapy for children with autism. Autism, 24(1), 211–220. https://doi.org/10.1177/1362361319849985
Ameis, S. H., Kassee, C., Corbett-Dick, P., Cole, L., Dadhwal, S., Lai, M. C., Veenstra-VanderWeele, J., & Correll, C. U. (2018). Systematic review and guide to management of core and psychiatric symptoms in youth with autism. Acta Psychiatrica Scandinavica, 138(5), 379–400. https://doi.org/10.1111/acps.12918
*Backman, A., Mellblom, A., Norman-Claesson, E., Keith-Bodros, G., Frostvittra, M., Bölte, S., & Hirvikoski, T. (2018). Internet-delivered psychoeducation for older adolescents and young adults with autism spectrum disorder (SCOPE): An open feasibility study. Research in Autism Spectrum Disorders, 54, 51–64. https://doi.org/10.1016/j.rasd.2018.07.001
Becker, K. D., Boustani, M., Gellatly, R., & Chorpita, B. F. (2018). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47(1), 1–23. https://doi.org/10.1080/15374416.2017.1326121
Benito, K. G., Caporino, N. E., Frank, H. E., Ramanujam, K., Garcia, A., Freeman, J., Kendall, P. C., Geffken, G., & Storch, E. A. (2015). Development of the pediatric accommodation scale: Reliability and validity of clinician-and parent-report measures. Journal of Anxiety Disorders, 29, 14–24. https://doi.org/10.1016/j.janxdis.2014.10.004
Bordin, E. S. (1979). The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research and Practice, 16(3), 252–260. https://doi.org/10.1037/h0085885
Borkovec, T. D., & Nau, S. D. (1972). Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry, 3(4), 257–260. https://doi.org/10.1016/0005-7916(72)90045-6
*Brewe, A. M., Mazefsky, C. A., & White, S. W. (2021). Therapeutic alliance formation for adolescents and young adults with autism: Relation to treatment outcomes and client characteristics. Journal of Autism and Developmental Disorders, 51(5), 1446–1457. https://doi.org/10.1007/s10803-020-04623-z
Brookman-Frazee, L., Stadnick, N., Chlebowski, C., Baker-Ericzén, M., & Ganger, W. (2018). Characterizing psychiatric comorbidity in children with autism spectrum disorder receiving publicly funded mental health services. Autism, 22(8), 938–952. https://doi.org/10.1177/1362361317712650
Brown, J. (2015). Specific techniques vs. common factors Psychotherapy integration and its role in ethical practice. American Journal of Psychotherapy, 69(3), 301–316. https://doi.org/10.1176/appi.psychotherapy.2015.69.3.301
*Brown, R., Iqbal, Z., Reynolds, L., Press, D. A., Shaker-Naeeni, H., Scrivener, L., et al. (2015). Inter-rater reliability of treatment fidelity and therapeutic alliance measures for psychological therapies for anxiety in young people with autism spectrum disorders. International Journal of Developmental Disabilities, 61(4), 190–199. https://doi.org/10.1179/2047387714Y.0000000050
*Burnham Riosa, P., Khan, M., & Weiss, J. A. (2019). Measuring therapeutic alliance in children with autism during cognitive behavior therapy. Clinical Psychology & Psychotherapy, 26(6), 761–767. https://doi.org/10.1002/cpp.2404
Calvocoressi, L., Lewis, B., Harris, M., Trufan, S. J., Goodman, W. K., McDougle, C. J., & Price, L. H. (1995). Family accommodation in obsessive-compulsive disorder. The American Journal of Psychiatry, 152(3), 441–443. https://doi.org/10.1176/ajp.152.3.441
*Chlebowski, C., Magaña, S., Wright, B., & Brookman-Frazee, L. (2018). Implementing an intervention to address challenging behaviors for autism spectrum disorder in publicly-funded mental health services: Therapist and parent perceptions of delivery with Latinx families. Cultural Diversity and Ethnic Minority Psychology, 24(4), 552–563. https://doi.org/10.1037/cdp0000215
Demetriou, E. A., Lampit, A., Quintana, D. S., Naismith, S. L., Song, Y. J., Pye, J. E., Hickie, I., & Guastella, E. A. (2018). Autism spectrum disorders: A meta-analysis of executive function. Molecular Psychiatry, 23(5), 1198–1204. https://doi.org/10.1038/mp.2017.75
Dew-Reeves, S. E., & Athay, M. M. (2012). Validation and use of the youth and caregiver Treatment Outcome Expectations Scale (TOES) to assess the relationships between expectations, pretreatment characteristics, and outcomes. Administration and Policy in Mental Health and Mental Health Services Research, 39(1–2), 90–103. https://doi.org/10.1007/s10488-012-0406-z
Doherty, A. J., Atherton, H., Boland, P., Hastings, R., Hives, L., Hood, K., James-Jenkinson, L., Leavey, R., Randell, E., Reed, J., Taggart, L., Wilson, N., & Chauhan, U. (2020). Barriers and facilitators to primary health care for people with intellectual disabilities and/or autism: An integrative review. BJGP Open. https://doi.org/10.3399/bjgpopen20X101030
*Drmic, I. E., Aljunied, M., & Reaven, J. (2017). Feasibility, acceptability and preliminary treatment outcomes in a school-based CBT intervention program for adolescents with ASD and anxiety in Singapore. Journal of Autism and Developmental Disorders, 47(12), 3909–3929. https://doi.org/10.1007/s10803-016-3007-y
*Edgington, L., Hill, V., & Pellicano, E. (2016). The design and implementation of a CBT-based intervention for sensory processing difficulties in adolescents on the autism spectrum. Research in Developmental Disabilities, 59, 221–233. https://doi.org/10.1016/j.ridd.2016.09.004
Feinberg, E., Kuhn, J., Eilenberg, J. S., Levinson, J., Patts, G., Cabral, H., & Broder-Fingert, S. (2021). Improving family navigation for children with autism: A comparison of two pilot randomized controlled trials. Academic Pediatrics, 21(2), 265–271. https://doi.org/10.1016/j.acap.2020.04.007
Fjermestad, K. W., Mowatt Haugland, B. S., Heiervang, E., & Öst, L. G. (2009). Relationship factors and outcome in child anxiety treatment studies. Clinical Child Psychology and Psychiatry, 14(2), 195–214. https://doi.org/10.1177/1359104508100885
*Gordon, K., Murin, M., Baykaner, O., Roughan, L., Livermore-Hardy, V., Skuse, D., & Mandy, W. (2015). A randomised controlled trial of PEGASUS, a psychoeducational programme for young people with high-functioning autism spectrum disorder. Journal of Child Psychology and Psychiatry, 56(4), 468–476. https://doi.org/10.1111/jcpp.12304
Hartley, M., Dorstyn, D., & Due, C. (2019). Mindfulness for children and adults with autism spectrum disorder and their caregivers: A meta-analysis. Journal of Autism and Developmental Disorders, 49(10), 4306–4319. https://doi.org/10.1007/s10803-019-04145-3
*Hillier, A., Greher, G., Poto, N., & Dougherty, M. (2012). Positive outcomes following participation in a music intervention for adolescents and young adults on the autism spectrum. Psychology of Music, 40(2), 201–215. https://doi.org/10.1177/0305735610386837
Hong, Q. N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., et al. (2018). The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information, 34(4), 285–291. https://doi.org/10.3233/EFI-180221
*Jassi, A., de la Cruz, L. F., Russell, A., & Krebs, G. (2021). An evaluation of a new autism-adapted cognitive behaviour therapy manual for adolescents with obsessive-compulsive disorder. Child Psychiatry & Human Development, 52, 916–927. https://doi.org/10.1007/s10578-020-01066-6
*Jones, G., & Jassi, A. (2020). Modified cognitive behavior therapy for severe, treatment resistant obsessive-compulsive disorder in an adolescent with autism spectrum disorder: The importance of parental involvement. Journal of Cognitive Psychotherapy, 34(4), 319–335. https://doi.org/10.1002/jclp.22396
*Kang, E., Gioia, A., Pugliese, C. E., Islam, N. Y., Martinez-Pedraza, F. D. L., Girard, R. M., McLeod, B. D., Carter, A. S., & Lerner, M. D. (2021). Alliance-outcome associations in a community-based social skills intervention for youth with autism spectrum disorder. Behavior Therapy, 52(2), 324–337. https://doi.org/10.1016/j.beth.2020.04.006
Karver, M. S., De Nadai, A. S., Monahan, M., & Shirk, S. R. (2018). Meta-analysis of the prospective relation between alliance and outcome in child and adolescent psychotherapy. Psychotherapy, 55(4), 341–355. https://doi.org/10.1037/pst0000176
Karver, M. S., Handelsman, J. B., Fields, S., & Bickman, L. (2005). A theoretical model of common process factors in youth and family therapy. Mental Health Services Research, 7(1), 35–51. https://doi.org/10.1007/s11020-005-1964-4
Karver, M. S., Handelsman, J. B., Fields, S., & Bickman, L. (2006). Meta-analysis of therapeutic relationship variables in youth and family therapy: The evidence for different relationship variables in the child and adolescent treatment outcome literature. Clinical Psychology Review, 26(1), 50–65. https://doi.org/10.1016/j.cpr.2005.09.001
Kazantzis, N., Whittington, C., Zelencich, L., Kyrios, M., Norton, P. J., & Hofmann, S. G. (2016). Quantity and quality of homework compliance: A meta-analysis of relations with outcome in cognitive behavior therapy. Behavior Therapy, 47(5), 755–772. https://doi.org/10.1016/j.beth.2016.05.002
*Kerns, C. M., Collier, A., Lewin, A. B., & Storch, E. A. (2018). Therapeutic alliance in youth with autism spectrum disorder receiving cognitive-behavioral treatment for anxiety. Autism, 22(5), 636–640. https://doi.org/10.1177/1362361316685556
King, G., Currie, M., & Petersen, P. (2014). Child and parent engagement in the mental health intervention process: A motivational framework. Child and Adolescent Mental Health, 19(1), 2–8. https://doi.org/10.1111/camh.12015
*Klebanoff, S. M., Rosenau, K. A., & Wood, J. J. (2019). The therapeutic alliance in cognitive-behavioral therapy for school-aged children with autism and clinical anxiety. Autism, 23(8), 2031–2042. https://doi.org/10.1177/1362361319841197
Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., Mandy, W., Szatmari, P., & Ameis, S. H. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. The Lancet Psychiatry, 6(10), 819–829. https://doi.org/10.1016/S2215-0366(19)30289-5
Lebowitz, E. R., Panza, K. E., Su, J., & Bloch, M. H. (2012). Family accommodation in obsessive-compulsive disorder. Expert Review of Neurotherapeutics, 12(2), 229–238. https://doi.org/10.1586/ern.11.200
Lebowitz, E. R., Scharfstein, L. A., & Jones, J. (2014). Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and nonanxious children. Depression and Anxiety, 31(12), 1018–1025. https://doi.org/10.1002/da.22251
Lewin, A. B., Peris, T. S., Bergman, R. L., McCracken, J. T., & Piacentini, J. (2011). The role of treatment expectancy in youth receiving exposure-based CBT for obsessive compulsive disorder. Behaviour Research and Therapy, 49(9), 536–543. https://doi.org/10.1016/j.brat.2011.06.001
*London, M. D., Mackenzie, L., Lovarini, M., Dickson, C., & Alvarez-Campos, A. (2020). Animal assisted therapy for children and adolescents with autism spectrum disorder: Parent perspectives. Journal of Autism and Developmental Disorders, 50(12), 4492–4503. https://doi.org/10.1007/s10803-020-04512-5
*Lordo, D. N., Bertolin, M., Sudikoff, E. L., Keith, C., Braddock, B., & Kaufman, D. A. (2017). Parents perceive improvements in socio-emotional functioning in adolescents with ASD following social skills treatment. Journal of Autism and Developmental Disorders, 47(1), 203–214. https://doi.org/10.1007/s10803-016-2969-0
Maddox, B. B., Crabbe, S., Beidas, R. S., Brookman-Frazee, L., Cannuscio, C. C., Miller, J. S., Nicolaidis, C., & Mandell, D. S. (2020). “I wouldn’t know where to start”: Perspectives from clinicians, agency leaders, and autistic adults on improving community mental health services for autistic adults. Autism, 24(4), 919–930. https://doi.org/10.1177/1362361319882227
Mattila, M. L., Hurtig, T., Haapsamo, H., Jussila, K., Kuusikko-Gauffin, S., Kielinen, M., Linna, S. L., Ebeling, H., Bloigu, R., Joskitt, L., Pauls, D. L., & Moilanen, I. (2010). Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: A community- and clinic-based study. Journal of Autism and Developmental Disorders, 40(9), 1080–1093. https://doi.org/10.1007/s10803-010-0958-2
Mazefsky, C. A., & White, S. W. (2014). Emotion regulation: Concepts & practice in autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America, 23(1), 15–24. https://doi.org/10.1016/j.chc.2013.07.002
McLeod, B. D. (2011). Relation of the alliance with outcomes in youth psychotherapy: A meta-analysis. Clinical Psychology Review, 31(4), 603–616. https://doi.org/10.1016/j.cpr.2011.02.001
McLeod, B. D., & Weisz, J. R. (2005). The therapy process observational coding system-alliance scale: Measure characteristics and prediction of outcome in usual clinical practice. Journal of Consulting and Clinical Psychology, 73(2), 323. https://doi.org/10.1037/0022-006X.73.2.323
*McNally Keehn, R. H., Lincoln, A. J., Brown, M. Z., & Chavira, D. A. (2013). The Coping Cat program for children with anxiety and autism spectrum disorder: A pilot randomized controlled trial. Journal of Autism and Developmental Disorders, 43(1), 57–67. https://doi.org/10.1007/s10803-012-1541-9
Merlo, L. J., Lehmkuhl, H. D., Geffken, G. R., & Storch, E. A. (2009). Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. Journal of Consulting and Clinical Psychology, 77(2), 355–360. https://doi.org/10.1037/a0012652
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Prisma Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Orlinsky, D. E. (2001). Psychotherapy process research. In N. J. Smelser & P. B. Baltes (Eds.), International Encyclopedia of the Social and Behavioral Sciences (pp. 12499–12504). Elsevier. https://doi.org/10.1016/B0-08-043076-7/01334-6
*Pahnke, J., Lundgren, T., Hursti, T., & Hirvikoski, T. (2014). Outcomes of an acceptance and commitment therapy-based skills training group for students with high-functioning autism spectrum disorder: A quasi-experimental pilot study. Autism, 18(8), 953–964. https://doi.org/10.1177/1362361313501091
Reaven, J. (2011). The treatment of anxiety symptoms in youth with high-functioning autism spectrum disorders: Developmental considerations for parents. Brain Research, 1380, 255–263. https://doi.org/10.1016/j.brainres.2010.09.075
Rogers, S. J., Estes, A., Vismara, L., Munson, J., Zierhut, C., Greenson, J., et al. (2019). Enhancing low-intensity coaching in parent implemented Early Start Denver Model intervention for early autism: A randomized comparison treatment trial. Journal of Autism and Developmental Disorders, 49(2), 632–646. https://doi.org/10.1007/s10803-018-3740-5
Roudbarani, F., Tablon Modica, P., Maddox, B. B., Bohr, Y., & Weiss, J. (In-press). Clinician factors related to the delivery of psychotherapy for autistic youth and youth with attention-deficit hyperactivity disorder. Autism: The International Journal of Research and Practice.
Salazar, F., Baird, G., Chandler, S., Tseng, E., O’sullivan, T., Howlin, P., Pickles, A., & Simonoff, E. (2015). Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2283–2294. https://doi.org/10.1007/s10803-015-2361-5
Shelef, K., & Diamond, G. M. (2008). Short form of the revised Vanderbilt Therapeutic Alliance Scale: Development, reliability, and validity. Psychotherapy Research, 18(4), 433–443. https://doi.org/10.1080/10503300701810801
Shirk, S. E., & Karver, M. (2011). Alliance in child and adolescent psychotherapy. In J. C. Norcross (Ed.), Psychotherapy relationships that work: Evidenced-based responsiveness (2nd ed., pp. 70–91). Oxford University Press.
Shirk, S. R., & Saiz, C. C. (1992). Clinical, empirical, and developmental perspectives on the therapeutic relationship in child psychotherapy. Development and Psychopathology, 4(4), 713–728. https://doi.org/10.1017/S0954579400004946
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/CHI.0b013e318179964f
Sprenkle, D. H., & Blow, A. J. (2004). Common factors and our sacred models. Journal of Marital and Family Therapy, 30(2), 113–129. https://doi.org/10.1111/j.1752-0606.2004.tb01228.x
*Storch, E. A., Zavrou, S., Collier, A. B., Ung, D., Arnold, E. B., Mutch, P. J., Lewin, A. B., & Murphy, T. K. (2015). Preliminary study of family accommodation in youth with autism spectrum disorders and anxiety: Incidence, clinical correlates, and behavioral treatment response. Journal of Anxiety Disorders, 34, 94–99. https://doi.org/10.1016/j.janxdis.2015.06.007
*Swain, D., Murphy, H. G., Hassenfeldt, T. A., Lorenzi, J., & Scarpa, A. (2019). Evaluating response to group CBT in young children with autism spectrum disorder. The Cognitive Behaviour Therapist, 12, 17. https://doi.org/10.1017/S1754470X19000011
Thomas, M. L. (2006). The contributing factors of change in a therapeutic process. Contemporary Family Therapy, 28(2), 201–210. https://doi.org/10.1007/s10591-006-9000-4
*Thomson, K., Riosa, P. B., & Weiss, J. A. (2015). Brief report of preliminary outcomes of an emotion regulation intervention for children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(11), 3487–3495. https://doi.org/10.1007/s10803-015-2446-1
Vasa, R. A., Carroll, L. M., Nozzolillo, A. A., Mahajan, R., Mazurek, M. O., Bennett, A. E., et al. (2014). A systematic review of treatments for anxiety in youth with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44, 3215–3229. https://doi.org/10.1007/s10803-014-2184-9
*Walsh, C. E., Moody, E., Blakeley-Smith, A., Duncan, A., Hepburn, S., Keefer, A., Klinger, L., Meyer, A., O’Kelley, S., & Reaven, J. (2018). The relationship between treatment acceptability and youth outcome in group CBT for youth with ASD and anxiety. Journal of Contemporary Psychotherapy, 48(3), 123–132. https://doi.org/10.1007/s10879-018-9380-4
Walters, S., Loades, M., & Russell, A. (2016). A systematic review of effective modifications to cognitive behavioural therapy for young people with autism spectrum disorders. Review Journal of Autism and Developmental Disorders, 3(2), 137–153. https://doi.org/10.1007/s40489-016-0072-2
Warwick, H., Reardon, T., Cooper, P., Murayama, K., Reynolds, S., Wilson, C., & Creswell, C. (2017). Complete recovery from anxiety disorders following Cognitive Behavior Therapy in children and adolescents: A meta-analysis. Clinical Psychology Review, 52, 77–91. https://doi.org/10.1016/j.cpr.2016.12.002
Weiss, J. A. (2014). Transdiagnostic case conceptualization of emotional problems in youth with ASD: An emotion regulation approach. Clinical Psychology: Science and Practice, 21(4), 331–350. https://doi.org/10.1111/cpsp.12084
*Weiss, J. A., Thomson, K., Burnham Riosa, P., Albaum, C., Chan, V., Maughan, A., Tablon, P., & Black, K. (2018). A randomized waitlist-controlled trial of cognitive behavior therapy to improve emotion regulation in children with autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 59(11), 1180–1191. https://doi.org/10.1111/jcpp.12915
Wergeland, G. J., Fjermestad, K. W., Marin, C. E., Haugland, B. S., Silverman, W. K., Öst, L. G., Havik, O. E., & Heiervang, E. R. (2015). Predictors of dropout from community clinic child CBT for anxiety disorders. Journal of Anxiety Disorders, 31, 1–10. https://doi.org/10.1016/j.janxdis.2015.01.004
Weston, L., Hodgekins, J., & Langdon, P. E. (2016). Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: A systematic review and meta-analysis. Clinical Psychology Review, 49, 41–54. https://doi.org/10.1016/j.cpr.2016.08.001
*White, S. W., Ollendick, T., Albano, A. M., Oswald, D., Johnson, C., Southam-Gerow, M. A., Kim, I., & Scahill, L. (2013). Randomized controlled trial: Multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(2), 382–394. https://doi.org/10.1007/s10803-012-1577-x
Wood, J. J., Drahota, A., Sze, K., Har, K., Chiu, A., & Langer, D. A. (2009). Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of Child Psychology and Psychiatry, 50(3), 224–234. https://doi.org/10.1111/j.1469-7610.2008.01948.x
Wood, J. J., Kendall, P. C., Wood, K. S., Kerns, C. M., Seltzer, M., Small, B. J., Lewin, A. B., & Storch, E. A. (2020). Cognitive behavioral treatments for anxiety in children with autism spectrum disorder: A randomized clinical trial. JAMA Psychiatry, 77(5), 474–483. https://doi.org/10.1001/jamapsychiatry.2019.4160
Acknowledgements
This work was supported by the York University Research Chair in Autism and Neurodevelopmental Disability Mental Health. Carly Albaum was funded by Canadian Institutes of Health Research Frederick Banting and Charles Best Canada Graduate Scholarship, Susan Mann Dissertation Scholarship, and Autism Scholars Doctoral Award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article. Funding sources were not involved in study design; collection, analysis, or interpretation of data; writing the manuscript; nor in the decision to submit the article for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albaum, C.S., Vashi, N., Bohr, Y. et al. A Systematic Review of Therapeutic Process Factors in Mental Health Treatment for Autistic Youth. Clin Child Fam Psychol Rev 26, 212–241 (2023). https://doi.org/10.1007/s10567-022-00409-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-022-00409-0