Abstract
Tetracaine, a local anesthetic, exhibits potent cytotoxic effects on multiple cancer; however, the precise underlying mechanisms of its anti-cancer activity remain uncertain. The anti-cancer activity of tetracaine was found to be the most effective among commonly used local anesthetics in this study. After tetracaine treatment, the differentially expressed genes in melanoma cells were identified by the RNAseq technique and enriched in the lysosome signaling pathway, cullin family protein binding, and proteasome signaling pathway through Kyoto Encyclopedia of Genes and Genomes. Additionally, the ubiquitin-like neddylation signaling pathway, which is hyperactivated in melanoma, could be abrogated due to decreased NAE2 expression after tetracaine treatment. The neddylation of the pro-oncogenic Survivin, which enhances its stability, was significantly reduced following treatment with tetracaine. The activation of neddylation signaling by NEDD8 overexpression could reduce the antitumor efficacy of tetracaine in vivo and in vitro. Furthermore, vemurafenib-resistant melanoma cells showed higher level of neddylation, and potential substrate proteins undergoing neddylation modification were identified through immunoprecipitation and mass spectrometry. The tetracaine treatment could reduce drug resistance via neddylation signaling pathway inactivation in melanoma cells. These findings demonstrate that tetracaine effectively inhibits cell proliferation and alleviates vemurafenib resistance in melanoma by suppressing the neddylation signaling pathway, providing a promising avenue for controlling cancer progression.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Melanoma is the most deadly kind of skin cancer, with a 5-year relative survival rate of only 32% for individuals diagnosed with stage IV (Markus et al. 2024). A retrospective study has suggested that patients may benefit from local anesthetics administered during cancer surgery (Tedore 2015). Through interactions with cancer cells, local anesthetics affect a variety of processes, including cell death pathways and epigenetics (Xuan et al. 2015). Tetracaine hydrochloride (TTC) has been shown to be safe and effective when used during eye surgery or skin laceration healing (Harman et al. 2013; Soltani et al. 2009). In addition to its analgesic effect, TTC also exhibits anti-tumor activity. For example, Yoon et al. have showed that TTC prevented the aggregation and reattachment of breast cancer cells by preventing the elongation of tubulin microtentacles (Yoon et al. 2011). Our previous research showed that TTC downregulates hnRNAP1 and thus disrupts cell cycle progression in melanoma (Huang et al. 2022). Patients with advanced melanoma may be accompanied by significant cancer pain in the course of conventional treatment, which seriously affects the quality of life. Hence, TTC can be considered as an adjuvant therapeutic strategy, exerting effective tumor-suppressive effect along with analgesia. However, this adjuvant therapeutic strategy needs further validation in clinical trials.
Ubquitinylation is a common post-translational modification that leads to the degradation of proteins in the proteasome. Several additional ubiquitin-like modifications, including neddylation and sumoylation, are generally involved in the onset and progression of cancer (Rong et al. 2013; Sanoj et al. 2020). Recently, researchers have discovered that neddylation effects protein function by binding NEDD8 (a ubiquitin-like protein) to the substrate protein (Vijayasimha and BP 2021). Adenylation initiates the neddylation cascade, which is then followed by activation of mature NEDD8 by NEDD8-activating enzyme (NAE), a complex made up of the subunits of UBA3 and NAE1. Thereafter, activated NEDD8 is transferred by a trans-thiolation process to either UBC12 or UBE2F. (Walden et al. 2003). Ultimately, the E3 ligase covalently attaches the NEDD8 to lysine residue on the substrate protein and thus completes the neddylation process (Gai et al. 2021). Recent studies demonstrated that the neddylation pathway considerably influences the functions of macrophages (Chang et al. 2012; Li et al. 2013), cancer-associated fibroblasts (CAFs) (Zhou et al. 2019), and tumor angiogenesis (Yao et al. 2014), eventually regulating tumorigenesis and the metastasis of tumor cells. Considering the vital role of the neddylation in cancer progression, suppressing this process may become a feasible therapeutic option for cancer. Our previous study indicated that the TTC-induced downregulation of hnRNPA1 might be associated with ubiquitination-like modifications of hnRNPA1. Thus, TTC might affect the neddylation signaling in melanoma cells. However, little relevant attention by researchers to studying the relationship between TTC and neddylation signaling has been paid to date.
Survivin is poorly expressed (barely detectable) in most normal tissues. However, it is remarkably increased in the majority of human cancers (Beate et al. 2022; Tianyou et al. 2017; Wenmei et al. 2019) and melanoma (Haixia et al. 2020), indicating that Survivin can be a tumor-associated antigen (TAA). Previous research has demonstrated that Survivin promoted the progression of UV-induced melanoma in vivo (Thomas et al. 2007) and enhanced the migration and invasion of melanoma cells probably through the modulation of Akt-dependent α5 integrin (McKenzie et al. 2010). Moreover, previous study has showed that MLN4924, a small molecule inhibitor of NAE, reduces Survivin expression, suggesting the neddylation signaling may be involved in regulating Survivin stability (Jin et al. 2018). However, more research is needed to elucidate the relationship between neddylation signaling and Survivin.
In recent years, BRAF inhibitors have demonstrated promising efficacy in melanoma patients (Chapman et al. 2011). However, about half of melanoma patients receiving BRAF inhibitor therapy have disease progression six to seven months after starting treatment. Moreover, intrinsic or acquired resistance to BRAF inhibitors limits their therapeutic utility (Flaherty et al. 2012; Sosman et al. 2012). Therefore, the investigation of the mechanisms underlying resistance to BRAF inhibitors, as well as the potential of drug combination strategies in BRAF-inhibitor-resistant melanoma is essential to improve patient outcomes.
Herein, TTC was demonstrated to exhibit the highest potential in suppressing melanoma proliferation. TTC could effectively inhibit the expression of NEDD8, which is overexpressed in melanoma and involved in the posttranslational modification of Survivin. Further experimental results also confirmed that the NEDD8 overexpression blocked the anti-tumor activity of TTC. Moreover, we studied the inhibitory effect of TTC on vemurafenib-resistant A375 (A375R) cells and investigated whether the combination of TTC and vemurafenib resulted in synergistic inhibition. The results indicated that TTC might be an efficient adjuvant agent in melanoma therapy.
Materials and methods
Cell culture
B16 cells (RRID: CVCL_F936) and A375 cells (RRID: CVCL_0132) were purchased from the Stem Cell Bank (Shanghai, China). Normal human epidermal melanocytes cells NHEM (RRID: CVCL_B447), A2058 cells (RRID: CVCL_1059), and SK-MEL-28 cells (RRID: CVCL_0526) were acquired from Procell Life Science & Technology Co., Ltd. (Wuhan, China). These cells were grown in RPMI-1640 or DMEM media (Hyclone, China) with 1% antibiotics (Beyotime, China) and 10% fetal bovine serum (PEAK SERUM, US) added as supplements. Parental A375 cells received treatment with successively increasing concentrations of vemurafenib (MCE, USA) from 0.1 to 2.0 μM in order to generate A375R cells.
Viability assay, immunostaining, and colony formation assay
Viability assay, immunostaining, and colony formation assay were conducted as previously described (Huang et al. 2022).
Immunohistochemistry (IHC)
Cutaneous melanoma and melanoma adjacent normal skin tissue array were obtained from US Biomax (ME241b). Sections were heated to induce epitope retrieval using antigen repair solution (Beyotime, Shanghai, China) after deparaffinization and rehydration. After that, the sections were treated overnight at 4 °C with primary antibodies (NEDD8, 1:100, Cell Signaling Technology). The sections were then allowed to react with streptavidin–biotin complex (SABC) after being treated for 30 min at 37 °C with biotin-labeled goat anti-rabbit IgG antibody. Color was developed using DAB substrate followed by hematoxylin counterstaining.
Western blot and qRT-PCR
Melanoma cells were treated with TTC (200 or 400 μM) or MLN4924 (0.1 μM) for 24 h. Western blotting and qRT-PCR were performed to detect the protein expression and mRNA expression as previously described (Huang et al. 2022). Main antibodies were as follows: β-actin (1:5000, catalog 4967, Cell Signaling Technology), NEDD8 (1:1000, catalog 2754, Cell Signaling Technology), NAE1 (1:1000, catalog 14,321, Cell Signaling Technology), UBA3 (1:500, catalog sc-377272, Santa Cruz Biotechnology), UBC12 (1:1000, catalog 14,520–1-AP, proteintech), cullin1 (1:1000, catalog R24008, Zen-Bioscience), and Survivin (1:1000, catalog R381056, Zen-Bioscience). Primer sequences were as follows: survivin (F: GAGGCTGGCTTCATCCACTG, R: ATGCTCCTCTATCGGGTTGTC); β-actin (F: GGCTGTATTCCCCTCCATCG, R: CCAGTTGGTAACAATGCCATGT).
Sequencing of RNA
A375 cells were treated with 400 μM TTC or vehicle for 24 h. According to manufacturer instructions, TRIzol reagent (Invitrogen, USA) was used to extract total RNA of A375 cells. The RNA was sequenced using the DNBseq platform in BGI (Shenzhen, China). Raw data was uploaded to GEO database (accession number: GSE273497).
Immunoprecipitation
The fragments of survivin (UniProt: O15392-1, 142 amino acids) were PCR-amplified with high-fidelity DNA polymerase (NEB, UK) using the cDNA from A375 cells as the template. Thereafter, the amplified gene was cloned into pcDNA3.1-Flag vector to construct recombinant plasmids pcDNA3.1-survivin-Flag, which were further confirmed by sequencing (Beijing Genomics Institute, China). A375 cells were transfected with recombinant plasmids pcDNA3.1-survivin-Flag until 70–80% confluence. After 2 days, the transfected cells were collected and lysed in iced NP40 lysis buffer with 1 mM PMSF. The NEDD8 primary antibody was added into the lysates for incubation at 4 °C overnight, and then for another 4 h incubation on a rotator with 50 μL protein A/G magnetic beads (Beyotime, China, P2108) addition to each sample. Beads were washed thrice with sterilized PBS buffer. Then the expression of survivin was detected using Western blot.
Lentiviral-mediated NEDD8 overexpression in melanoma cells
The NEDD8 gene was subjected to reverse-PCR amplification and inserted into the pLVX-DsRed-Monomer-N1 plasmid with BamH1 and Xba1 enzyme sites. Thus, the recombinant lentivirus plasmid pLVX-NEDD8 was generated, which was confirmed by sequencing (Beijing Genomics Institute, China). The lentiviral plasmid pLVX-NEDD8 or the control vector pLVX-DsRed-Monomer-N1 was co-transfected with packaging vectors pCMV-VSV-G (Addgene, USA, 8454) and pCMV-dR8.2 dvpr (Addgene, USA, 8455) into HEK293T cells for lentivirus production using Effectene Transfection Reagent (Qiagen, USA, 301,427). The lentivirus supernatant was then applied for melanoma cell infection. Melanoma cells were screened using 2 µg/mL puromycin (Beyotime, China, ST551) for 7 days. Melanoma cells with stable NEDD8 overexpression were validated by Western blot.
Establishment of melanoma subcutaneous tumor model
4-week-old C57BL/6 male mice were purchased from Chengdu Dossy Experimental Animals Co., Ltd and housed at the Animal Experimental Center of Southwest Medical University. The melanoma subcutaneous tumor model was constructed following the method described in our previous report (Huang et al. 2022). Briefly, melanoma cells (1 × 106) were subcutaneously injected into C57BL/6 mice. When the tumor volume reaches approximately 30 mm3, TTC (10 mg/kg), MLN4924 (30 mg/kg), or the same dose of normal saline (NS) was administered by intraperitoneal injection once a day. After continuously observing the growth of the subcutaneous tumor for seven days, the mice were euthanized with pentobarbital sodium and subcutaneous melanoma were removed.
Mass spectrometry
A375 and A375R cell lysates were homogenized and incubated with the NEDD8 primary antibody overnight at 4 °C, followed by immunoprecipitation with protein A/G magnetic beads (Beyotime, China, P2108) for 4 h at 4 °C. After three washes with sterile PBS. Coimmunoprecipitates were resolved by SDS-PAGE and immunoblotted through Western blotting. The gels were silver-stained (Beyotime, China, P0017S) and bands with significant differences were precisely excised for mass spectrometry. In-gel tryptic digestion was performed before analysis by ion trap mass spectrometry (Applied Protein Technology China). Tandem mass spectrometry coupled with database searching was used to determine the amino acid sequences of precipitated proteins.
Statistics
The statistical analysis was performed using GraphPad Prism 8.0. The data are expressed as mean ± standard deviation (SD). Comparisons between the two groups were performed by an unpaired two-tailed student’s t-test. Comparisons among multiple groups were performed using a one-way analysis of variance (ANOVA). Post-hoc analysis was performed by using Tukey’s post-hoc test following ANOVA. The statistical significance level was set at P < 0.05.
Results
TTC exerted a potent anti-cancer effect in melanoma among common local anesthetics
To test the anti-cancer effect of local anesthetics (tetracaine, procaine, lidocaine, bupivacaine, and ropivacaine) on melanoma cell viability, B16, and A375 cells were exposed to different local anesthetics at indicated concentrations and their viability was estimated by CCK-8 assay. Local anesthetics inhibited the cell viability of A375 and B16 cells in a dose-dependent manner (Fig. 1A and B). In addition, the results demonstrated that TTC exhibited the most prominent inhibitory effect on the viability of melanoma cells compared to other local anesthetics. Consistent with the results of CCK8, colony formation assays also demonstrated TTC was the most potent anti-cancer agent among common local anesthetics (Fig. 1C and D; Fig. S1).
Tetracaine hydrochloride (TTC) exhibited the most pronounced potential to suppress melanoma proliferation melanoma. A, B Melanoma cells (B16 and A375 cells) were treated with different local anesthetic drugs (tetracaine, procaine, lidocaine, bupivacaine, and ropivacaine) for 24 h and cell viability was normalized against the vehicle control group and expressed in percentage. Cell viability (%) = 100 × (absorbance (local anesthetics)—absorbance (cell-free control)) / (absorbance (vehicle control)—absorbance (cell-free control)). C, D B16 and A375 cells were exposed to 50 or 100 μM TTC, then the number of colonies was counted under the optical microscope. Data are expressed as the mean ± SD. Statistical differences were determined using an unpaired two-tailed student’s t-test, ***P < 0.001 vs the control group
Neddylation signaling pathway inactivation was involved in the anti-tumor activity of TTC according to RNAseq data
To understand the plausible mechanism of the anti-cancer activity of TTC and identify potential functional targets, A375 cells were treated in triplicate for 24 h with 400 μM TTC or vehicle. Then total RNA of A375 cells was isolated and sequenced. 841 upregulated and 287 downregulated genes were identified in the TTC group compared to the control group using the limma R package (Fig. 2A and Table. S1). These differentially expressed genes (DEGs) were mainly enriched in the lysosome signaling pathway (Fig. 2B). Lysosomes are acidic degradative organelles that play an important role in protein degradation and recycling. The KEGG analysis indicated that TTC might affect the degradation process of proteins. Additionally, further GSEA revealed that the cullin family protein binding and proteasome signaling pathway were enriched (Fig. 2C and D). The cullin family protein are the most common substrates of neddylation. Neddylation is a ubiquitination-like process in which NEDD8 is conjugated to particular substrates, and this process regulates the stability of proteins. Because of the close relationships between the neddylation signaling pathway and the three enriched biological processes or aforementioned pathways, the neddylation signaling pathway was probably involved in the anti-tumor activity of TTC.
The gene alteration and significantly enriched pathways after TTC treatment. A Differentially expressed genes (DEGs) were identified using the R package limma, and the criteria for differential analysis were set as follows: P < 0.05 and |log2 FC|> 1. B Based on these DEGs, the KEGG enrichment analysis was performed by the R package clusterProfiler. C, D GSEA was performed by the GSEA software (Version: 4.2.3) based on our transcript RNA high-throughput sequencing
Neddylation signaling is highly activated in melanoma
Neddylation is a crucial post-translational modification that is over-activated in multiple cancers and has been validated as an attractive therapeutic target for anti-cancer strategies (Daniel et al. 2023; Gai et al. 2021; Jin et al. 2018). To evaluate the role of NEDD8 in melanoma tumorigenesis, the NEDD8 expression level in cutaneous melanoma and adjacent areas of cutaneous melanoma was measured. Immunohistochemical staining confirms that the NEDD8 expression level is significantly higher in cutaneous melanoma than in the adjacent normal skin tissue (Fig. 3A). Furthermore, the expression level of NEDD8-conjugated proteins in different melanoma cell lines (B16, A375, SK-MEL-28, A2058) and normal melanocytes was detected (Fig. 3B). The western blot analysis (Fig. 3C) indicates an increased expression of NEDD8-conjugated proteins in melanoma cell lines compared to normal human melanocytes. Comprehensively, these results encourage efforts to treat human melanoma by pharmacological inhibition of the neddylation pathway.
NEDD8 protein expression was significantly higher in melanoma than in normal skin tissues. A IHC (immunohistochemical) staining showed that the NEDD8 expression level was significantly higher in melanoma tissues (n = 20) than in the adjacent normal skin tissues (n = 4). Scale bar = 200 μm. B, C NEDD8-conjugated protein expression levels in normal human epidermal melanocytes (NHEM) cells and melanoma cells (B16, A375, SK-MEL-28, and A2058) were determined by western blotting analysis. Data are expressed as the mean ± SD. Statistical differences were determined using one-way ANOVA, followed by post hoc Tukey's test, **P < 0.01, and ***P < 0.001 vs. NHEM group
TTC inhibited neddylation in melanoma cells
Based on the findings of the high throughput transcriptome sequencing and the correlation between NEDD8 and melanoma malignant progression, the effect of TTC on the neddylation pathway was investigated. MLN4924, a well-identified specific inhibitor of the enzymatic action of NAE, served as the positive control in the subsequent experiments. First, the post-TTC treatment expression levels of the NEDD8-conjugated proteins were measured. As shown in Fig. 4A, TTC reduced the expression of NEDD8-conjugated proteins in both B16 and A375 cells. Neddylation occurs through a ubiquitylation-like enzymatic cascade in which NEDD8 is activated by NAE and is subsequently transferred to the UBC12. Therefore, the effect of TTC on NAE1, UBA3, and UBC12 in both B16 and A375 cells was analyzed (Fig. 4B and C). Our experimental results demonstrated that TTC downregulated the UBA3 expression but had no effect on NAE1 and UBC12 expressions (Fig. 4D and E). In addition, the neddylation level of cullin1, one of the most typical target proteins for neddylation, significantly decreased in B16 and A375 cells after TTC treatment (Fig. 4D and E). These results comprehensively indicate that TTC downregulates the neddylation signaling pathway by inhibiting UBA3 expression. Additionally, both MLN4924 and TTC exhibited significant anti-tumor activity in vivo (Fig. 4F and G).
Effect of TTC treatment on neddylation in melanoma cells. A B16 and A375 cells were treated with 200 μM or 400 μM TTC for 24 h, and the western blot analysis showed TTC reduced the expression levels of NEDD8-conjugated proteins. B-C Melanoma cells were treated with MLN4924 (0.1 μM) or TTC (200 or 400 μM) for 24 h, cullin1 neddylation, and protein levels of NAE1, UBA3, and UBC12 were estimated by western blotting analysis. D-E The relative levels of each protein expression were determined by ImageJ software. F A mice subcutaneous tumor model was established by the subcutaneous injection of B16 cells. When the tumors reached a volume of approximately 30 mm3, the mice received seven daily intraperitoneal injections of either MLN4924 (30 mg/kg) or TTC (10 mg/kg). The tumors from each group were photographed with a millimeter ruler (n = 6). G The weight of individual tumors in each group was measured by an electronic balance (n = 6). Data are expressed as the mean ± SD. Statistical differences were determined using one-way ANOVA, followed by post hoc Tukey's test, *P < 0.05, **P < 0.01, and ***P < 0.001 vs. control group
TTC exerts anti-tumor activity by downregulating the neddylation signaling pathway in melanoma
To further investigate the effects of neddylation signaling pathway activation on the TTC-induced inhibition of melanoma, NEDD8 was overexpressed via the recombinant lentivirus approach to increase the ratio of free NEDD8 in B16 cells and activate the neddylation signaling pathway as previously reported (Hjerpe et al. 2012). The cell lines stably overexpressing GFP served as a control group. Both the cell viability and colony number of B16 cells stably overexpressing NEDD8 were higher compared to the control group (Fig. 5A-C). Moreover, the anti-tumor activity of TTC is partially weakened by overexpression of NEDD8 (Fig. 5A-C). Similar result was obtained when cell proliferation was measured by immunofluorescence staining for Ki67 and EDU staining assay (Fig. S2 and Fig. S3). Thereafter, the expression of NEDD8-conjugated proteins and Survivin were detected by immunoblotting assay. The results indicated a significantly higher expression level of NEDD8-conjugated proteins in the LV-NEDD8 group than that in the LV-GFP group (Fig. 5D), validating the overexpression of NEDD8 in the LV-NEDD8 group. However, there was no significant difference in Survivin expression between LV-NEDD8 and LV-GFP groups (Fig. 5E). Moreover, NEDD8 overexpression was found to diminish the effects of TTC on downregulating Survivin expression (Fig. 5E). These finds suggest that neddylation plays a crucial role in mediating the anti-tumor effect of TTC on melanoma.
NEDD8 overexpression impeded the anti-tumor activity of TTC. A The B16 cell line with stable NEDD8 overexpression was established via lentivirus infection, and the GFP-stable expression cell line was used as a control. After TTC treatment, the viability of B16 cells with NEDD8 or GFP overexpression were detected by CCK-8 assay. B, C After TTC treatment, the colony-forming ability of B16 cells with NEDD8 or GFP overexpression were detected by colony-formation assay. D, E Expression levels of NEDD8-conjugated proteins and Survivin were measured by western blot analysis. Data are expressed as the mean ± SD. Statistical differences were determined using one-way ANOVA, followed by post hoc Tukey's test, **P < 0.01, ***P < 0.001 vs. LV-GFP without TTC group; #P < 0.05, ##P < 0.01 vs. LV-GFP + TTC group. $$$P < 0.001 vs. LV-NEDD8 without TTC group
TTC decreased the stability of Survivin
Survivin, a member of inhibitor of apoptosis protein (IAP) family, is upregulated in human melanoma and contributes to the onset and progression of melanoma (Dallaglio et al. 2012). Its degradation is mediated by Fbxl7 via ubiquitylation (Yuan et al. 2015). The neddylation is capable of antagonizing ubiquitylation and enhances protein stability (Junhong et al. 2017; Tingting et al. 2014). Furthermore, X-linked inhibitor of apoptosis protein (XIAP), another member of IAP family, can undergo neddylation modification (Taiki et al. 2012). Therefore, our focus lies on elucidating the role of the Survivin and its neddylation in melanoma. Herein, whether TTC regulates Survivin expression was determined. TTC significantly downregulated the protein expression level of Survivin (Fig. 6A and B) and slightly reduced the mRNA expression level of Survivin (Fig. 6C), indicating that TTC treatment mainly influences the expression of Survivin at the protein level. To further explore the role of TTC in regulating Survivin expression, the expression of Survivin in melanoma cells treated with the protein synthesis inhibitor cycloheximide (CHX) and TTC was measured (Fig. 6D). The results showed that TTC enhanced the degradation of Survivin in B16 and A375 cells (Fig. 6E and G). Furthermore, TTC-induced Survivin degradation could be partially blocked by MG132, suggesting that proteasome degradation plays a critical role in modulating Survivin stability (Fig. 6F and H). Considering the regulatory role of TTC in the neddylation pathway, we next investigated whether TTC modulates the stability of Survivin by regulating its neddylation. The results of the coimmunoprecipitation (Co-IP) demonstrated the interaction between Survivin and NEDD8 (Fig. 6I), supporting the hypothesis that TTC decreased Survivin level via promoting the degradation of Survivin.
TTC affected the stability of Survivin. A, B B16 and A375 cells were treated with 200 or 400 μM TTC. After 24 h, western blot analysis was performed to detect Survivin expression at the protein level. C After the treatment of TTC (200 or 400 μM), the mRNA expression level of Survivin was detected by qRT-PCR. D, E, and G Stability of the Survivin protein was detected in CHX-treated cells in the presence or absence of TTC. F, H Following the administration of MG132 and TTC, immunoblotting was performed to measure the Survivin expression level. I A375 cells were transfected with pcDNA3.1-survivin-Flag constructs for 48 h. Result of Co-IP showed that Survivin interacts with NEDD8. In Fig. 6B, C, E, and G, data are expressed as the mean ± SD. Statistical differences were determined using an unpaired two-tailed student’s t-test, *P < 0.05, **P < 0.01, and ***P < 0.001 vs. the control group. In Fig. 6H, data are expressed as the mean ± SD. Statistical differences were determined using one-way ANOVA, followed by post hoc Tukey's test, **P < 0.01, and ***P < 0.001 vs. control group; ###P < 0.001 vs. TTC group
Activating the neddylation signaling pathway alleviated TTC-induced melanoma growth suppression in the mouse subcutaneous tumor model
The macroscopic appearance shows that TTC significantly inhibited melanoma growth in the LV-GFP or the LV-NEDD8 group (Fig. 7A). In LV-GFP groups, the weight of tumors in the TTC group decreased by approximately 54% (P = 0.031) compared to the NS group. In LV-NEDD8 groups, the weight of melanoma in the TTC group decreased by approximately 34% (P = 0.037) compared to the NS group (Fig. 7B). In addition, the tumors formed in the LV-NEDD8 group were approximately 63% heavier than those in the LV-GFP group when NS was injected intraperitoneally (P = 0.016). Conversely, When TTC was injected intraperitoneally, the tumors developed from NEDD8-transfected cells were approximately 148% heavier than those from GFP-transfected cells (P = 0.013). Similar result was obtained when cell proliferation was measured by Ki67 immunohistochemistry (Fig. S4). Moreover, TTC suppressed the expression levels of both NEDD8-conjugated proteins and Survivin in the mouse subcutaneous melanoma model, which was consistent with the in vitro findings (Fig. 7C and D). Additionally, NEDD8 overexpression attenuated Survivin downregulation mediated by TTC (Fig. 7C and D). These results implied that TTC suppressed the neddylation pathway and downregulated Survivin, thereby inhibiting melanoma growth in the mouse subcutaneous tumor model.
TTC suppressed melanoma cell growth by inhibiting neddylation in vivo. A mice subcutaneous tumor model was established by the subcutaneous injection of B16 cells with overexpressed NEDD8 or GFP. When the tumors reached a volume of approximately 30 mm3, the mice received seven daily intraperitoneal injections of either NS or TTC (10 mg/kg). A The tumors from each group were photographed with a millimeter ruler (n = 6). B The weight of individual tumors in each group was measured by an electronic balance (n = 6). C, D Expression levels of NEDD8-conjugated proteins and Survivin in melanoma tissues were detected by western blot analysis. Data are expressed as the mean ± SD. Statistical differences were determined using one-way ANOVA, followed by post hoc Tukey's test, *P < 0.05, **P < 0.01 vs. LV-GFP group; #P < 0.05 vs. LV-NEDD8 group. $P < 0.05 vs. LV-GFP + TTC group.
Anti-tumor activity of TTC in vemurafenib-resistance melanoma
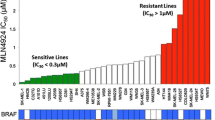
A2058 cells exhibit intrinsic vemurafenib resistance. The CCK-8 assay also indicated that vemurafenib had little effect on the viability of A2058 cells (Fig. 8A). Notably, the expression of NEDD8-conjugated proteins in A2058 cells was higher than that in other melanoma cells (Fig. 3C). Hence, the association of the activation of the neddylation signaling pathway with vemurafenib resistance was studied. First, A375R cells were obtained by continuously exposing the cells to 2 μM vemurafenib for more than 3 months. Thereafter, CCK-8 assays confirmed that at concentrations up to 4 μM, vemurafenib had no significant effect on the viability ofA375R cells (Fig. 8B). Additionally, the immunofluorescence indicated significant activation of the neddylation signaling pathway in A375R cells (Fig. 8D). To investigate the proteins exhibiting elevated neddylation modification levels in A375R cells, we conducted silver staining following immunoprecipitation of NEDD8 from A375 and A375R cell lysates (Fig. 8E). Subsequently, the silver-stained gel bands with significant alteration at approximately 25 kDa, 35 kDa and 45 kDa were observed and subjected to mass spectrometry analysis. Numerous proteins were identified as the potential substrates for neddylation modification, including hnRNPA1, Rps4x, Aldob, etc. (Table. S2). These proteins were enriched through KEGG pathway analysis and found to be mainly associated with the Ribosome, Spliceosome, and Glycolysis/Gluconeogenesis pathway (Fig. 8F and Table. S3).
Anti-tumor activity of TTC in vemurafenib-resistant melanoma. A Effect of vemurafenib on the activity of A2058 cells. B Effect of vemurafenib on the activity of vemurafenib-resistant A375 (A375R) cells. C CCK-8 assay was performed to detect the effect of TTC or (and) vemurafenib on the cell viability of A375R cells in vitro. D Immunofluorescence showed that the NEDD8 expression was higher in A375R cells than that in A375 cells. Scale bar = 100 μm. E Samples obtained from co-immunoprecipitation experiments in A375 and A375R cell lysates using the NEDD8 primary antibody were subjected to SDS-PAGE, followed by silver staining, and the significantly altered bands were marked with red boxes (approximately at 25 kDa, 35 kDa and 45 kDa). F The proteins within the altered bands were identified by mass spectrometry and then enriched by KEGG analysis. G, H, and I After the TTC or vemurafenib treatment, the expression levels of vital proteins for the neddylation pathway (NAE1, UBA3, UBC12, and Cullin1) were assessed by western blot analysis and quantitatively analyzed by ImageJ software. Data are expressed as the mean ± SD. Statistical differences were determined using one-way ANOVA, followed by post hoc Tukey's test, *P < 0.05, ***P < 0.001 vs. control group; ###P < 0.001 vs. PLX group; $P < 0.05 vs. TTC group; &P < 0.05, &&&P < 0.001 vs. control group (A375R cells)
As TTC significantly inhibited the activation of the neddylation signaling pathway in melanoma, the anti-tumor activity of TTC in A375R cells was further explored via cell viability analysis. The findings demonstrated that TTC could significantly decrease the cell viability of A375R cells. TTC in combination with vemurafenib achieved a better anti-tumor effect compared to the treatment with vemurafenib or TTC alone (Fig. 8C). Thereafter, the expression of the key proteins associated with neddylation in A375R cells were detected. As shown in Fig. 8G-I, TTC decreased the NEDD8 conjunction, UBA3 expression, and cullin1 neddylation, without affecting the NAE1 and UBC12 expression levels. Furthermore, the combined administration of TTC and vemurafenib induced more pronounced suppression of global NEDD8 conjunction, UBA3 expression, and cullin1 neddylation than TTC alone. These results comprehensively suggest a significant anti-tumor effect of TTC via neddylation signaling inactivation in A375R cells.
Discussion
Local anesthetics have been shown in several recent investigations to have anti-tumor effect against several tumor cell types (Chang et al. 2014a, 2014b; Yang et al. 2022; Zhao et al. 2021). These findings are of considerable clinical significance in guiding the anesthetic protocol of oncological surgery and the drug selection for postoperative analgesia. Herein, the anti-tumor activity of several common local anesthetics on melanoma cells was determined, suggesting that TTC exhibited the highest inhibitory effect (Fig. 1). This result is supported by a previous study (Yoon et al. 2011) and our published article (Huang et al. 2022). Survivin is upregulated in several cancers including melanoma (Gunaldi et al. 2018; Haixia et al. 2020; Li et al. 2018), which may be associated with tumor metastasis and chemoresistance (Mak et al. 2017). Our experimental findings indicate that TTC treatment can effectively inhibit the expression of Survivin. Hence, this may be a plausible mechanism via which TTC inhibits the proliferation of melanoma cells. Additionally, TTC slightly reduced the mRNA expression level of Survivin, indicating that TTC treatment mainly influences the Survivin stability. To further elucidate the probable mechanism, protein stability assay and CoIP experiments were performed. The results demonstrated that TTC could regulate Survivin expression by reducing Survivin stability. This explained why Survivin was not included in the DEGs in our RNAseq analysis results (Table S1). The aforementioned results indicate that TTC inhibits melanoma cell vaibility by regulating the post-translational modifications of Survivin. This is consistent with the finding of KEGG enrichment analysis, which suggest that the DEGs were significantly enriched in the lysosome pathway (Fig. 2). Furthermore, some researchers have reported that local anesthetics can affect epigenetic modifications, such as DNA methylation in tumor cells (Lirk et al. 2014; Lirk et al. 2012).
Neddylation and lysosomes have been linked in multiple biological processes, particularly in the degradation of proteins. For example, polyneddylation contributes to autophagic degradation in lysosomes, wherein this process is regulated by the scaffolding function of HYPK. HYPK regulates aggrephagy by specifically binding to NEDD8 and LC3 (Debasish and A 2021). MLN4924 is also reported to induce autophagy in liver cancer cells (Zhong et al. 2012). Furthermore, neddylation modification of Coro1a regulated lysosomal targeting of multivesicular bodies (MVBs) (Xuefeng et al. 2021), which may be a contributing factor to the effect of neddylation modifications on protein stability. These facts suggest a strong connection between neddylation and lysosomes, but further exploration is needed to uncover the underlying details.
Aberrant activation of neddylation signaling pathway was reported in several cancers, including melanoma (Fang et al. 2014; Jia et al. 2019; Jin et al. 2018; Li et al. 2014a; Xu et al. 2015). Herein, our results also indicated the activation of neddylation signaling pathway in multiple melanoma cells compared to normal human melanocytes. Since TTC significantly inhibited the neddylation modification (Fig. 4 and Fig. 7), further investigation was conducted to discover the crucial enzymes involved in this pathway. Our results imply that TTC may suppress neddylation modification by decreasing UBA3 expression (Fig. 4). Notably, the concentrations of TTC used in this study were 200 or 400 μM, which is much higher than what is used for most of the small molecule inhibitors. These observations suggest that TTC may not directly target NAE2. In addition, molecular docking was performed, revealing low binding affinity between TTC and NAE (Fig. S5). The aforementioned results suggest that TTC downregulates the neddylation signaling pathway possibly through other enzymes or indirectly inhibiting UBA3 expression. TTC has been shown to inhibit the mitochondrial ATPase activity and therefore the production of ATP (Aaron et al. 1984). As neddylation is an ATP-dependent process, TTC may inhibit the neddylation modification levels in melanoma by suppressing mitochondrial ATPase activity.
A previous study indicated a crucial part of Survivin in the development and metastasis of melanoma (Thomas et al. 2007). Since the ubiquitination of Survivin has been extensively investigated (Chandrasekaran et al. 2022; Li et al. 2020; Li et al. 2014), the possibility of a ubiquitination-like modification of Survivin was investigated. The CoIP experiment confirmed the interaction between Survivin and NEDD8 (Fig. 5). However, identification of the specific modification sites of Survivin and the interaction mechanism between Survivin and NEDD8 still requires further investigation. In addition, our previous research indicated that TTC may affect the neddylation of hnRNPA1 (Huang et al. 2022), indicating that the neddylation modification may be affected by TTC. Therefore, identifying specific neddylation substrates affected by TTC will help to explain the mechanism underlying the anti-tumor activity of TTC.
The current study also discovered a significant association between neddylation signaling and vemurafenib resistance. Firstly, the expression of NEDD8-conjugated proteins was compared, demonstrating activated neddylation signaling in melanoma cells. Additionally, a distinct protein band at approximately 45 kD was observed when detecting NEDD8-conjugated proteins in A2058 cells (Fig. 3). Notably, the A2058 cells exhibits intrinsic resistance to vemurafenib (Feng et al. 2016), suggesting that the activation of neddylation signaling may contribute to vemurafenib resistance. The immunoblotting assay results also indicated the activation of neddylation signaling and a similar distinct protein band at approximately 45 kD in A375R cells (Fig. 8). Furthermore, the potential substrate proteins undergoing neddylation modification were also identified through immunoprecipitation and mass spectrometry in A375R cells. These results suggested a strong correlation between the neddylation modification and vemurafenib resistance in melanoma, representing novel evidence highlighting the role of neddylation in conferring vemurafenib-resistance in melanoma. Thus, these results provide theoretical support for utilizing a neddylation inhibitor (MLN4924) as a therapeutic agent for patients with vemurafenib-resistant melanoma. Furthermore, these findings offer a rational basis for combining vemurafenib with MLN4924 as a treatment strategy for BRAF-mutated melanoma, thereby preventing the development of drug resistance.
MLN4924, discovered via high-throughput screening, demonstrated promise for cancer treatment (Soucy et al. 2009). Subsequent studies suggested more plausible mechanisms for the anti-tumor activity of MLN4924, including triggering protective autophagy and upregulation of the c-Myc-Noxa axis (Jia et al. 2019; Luo et al. 2012). Currently, several studies investigating the clinical utility of MLN4924 (NCT03772925, NCT04800627, NCT03965689, NCT03238248) are underway. Herein, the melanoma suppressive efficacy of MLN4924 was confirmed in vivo and in vitro. Interestingly, TTC exhibited better anti-tumor activity (Fig. 4), suggesting that TTC may exert anti-tumor activity through other potential mechanisms apart from the inhibition of the neddylation signaling pathway. For example, our previous research has demonstrated that TTC arrests the G0/G1 cell cycle and inhibits melanoma proliferation (Huang et al. 2022). Despite the potential cardiotoxicity and neurotoxicity of high concentrations of TTC, it is expected to find new anti-tumor targets by investigating the potential mechanisms underlying the anti-tumor activity of TTC. Developing computer-aided drug designs based on these targets is promising to enhance the efficacy of anti-tumor therapies. In addition, the molecular modification or detoxification of TTC will be favorable for its clinical anti-tumor application. A group of Turkish scientists have designed several new drugs based on the molecular structure of TTC and finally screened a small molecule, which effectively suppressed the growth of HepG2 and A549 cells at low concentrations (İhsan et al. 2022). However, the anti-tumor effects of this small molecule still require further confirmation in other tumor cells and animal models, and the underlying molecular mechanisms of anti-tumor activity need to be thoroughly investigated. Engineered nanomaterials and targeted extracellular vesicles for drug delivery can achieve more precise drug targeting (Gudbergsson 2020; Palombo et al. 2014), which can provide novel insights to expand the clinical application of TTC as an adjuvant agent in combination with other conventional therapies.
In conclusion, TTC exhibits pronounced proliferation suppressive potential against melanoma. Inhibition of the neddylation pathway might be the potential mechanism underlying this anti-tumor activity of TTC. Furthermore, it was proposed for the first time in this study that activation of the neddylation pathway may be a potential mechanism of vemurafenib resistance in melanoma. Additionally, TTC inhibits the neddylation pathway and cell viability in A375R cells.
Data availability
Sequence data that supports the findings of this study is deposited in the GEO database (accession number: GSE273497). Other data are available from the corresponding author upon reasonable request.
Abbreviations
- A375R:
-
Vemurafenib-resistant A375
- BCA:
-
Bicinchoninic acid
- CAFs:
-
Cancer-associated fibroblasts
- CHX:
-
Cycloheximide
- CoIP:
-
Coimmunoprecipitation
- DEGs:
-
Differentially expressed genes
- GSEA:
-
Gene set enrichment analysis
- IC50:
-
Half-maximal inhibitory concentration
- IHC:
-
Immunohistochemistry
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- NAE:
-
NEDD8-activating enzyme
- NS:
-
Normal saline
- OS:
-
Overall survival
- RFS:
-
Relapse-free survival
- SABC:
-
Strept avidin–biotin complex
- SD:
-
Standard deviation
- TAA:
-
Tumor-associated antigen
- TTC:
-
Tetracaine hydrochloride
- UBA3:
-
Ubiquitin like modifier activating enzyme 3
References
Aaron A, Chignell D, Vanderkooi G. Local anesthetics: A new class of partial inhibitors of mitochondrial ATPase. J Bioenerg Biomembr. 1984;16(5–6):353–63. https://doi.org/10.1007/bf00743231.
Beate V, Bhowmick R, Greiwe L, Schäffer V, Eilers M, Reinkens T, et al. MicroRNA-449a Inhibits Triple Negative Breast Cancer by Disturbing DNA Repair and Chromatid Separation. Int J Mol Sci. 2022;23(9):5131. https://doi.org/10.3390/ijms23095131.
Chandrasekaran AP, Tyagi A, Poondla N, Sarodaya N, Karapurkar JK, Kaushal K, et al. Dual role of deubiquitinating enzyme USP19 regulates mitotic progression and tumorigenesis by stabilizing survivin. Mol Ther. 2022;30(11):3414–29. https://doi.org/10.1016/j.ymthe.2022.07.019.
Chang FM, Reyna SM, Granados JC, Wei SJ, Innis-Whitehouse W, Maffi SK, et al. Inhibition of neddylation represses lipopolysaccharide-induced proinflammatory cytokine production in macrophage cells. J Biol Chem. 2012;287(42):35756–67. https://doi.org/10.1074/jbc.M112.397703.
Chang YC, Liu CL, Chen MJ, Hsu YW, Chen SN, Lin CH, et al. Local anesthetics induce apoptosis in human breast tumor cells. Anesth Analg. 2014a;118(1):116–24. https://doi.org/10.1213/ANE.0b013e3182a94479.
Chang YC, Hsu YC, Liu CL, Huang SY, Hu MC, Cheng SP. Local anesthetics induce apoptosis in human thyroid cancer cells through the mitogen-activated protein kinase pathway. PLoS ONE. 2014b;9(2):e89563. https://doi.org/10.1371/journal.pone.0089563.
Chapman PB, Hauschild A, Robert C, Haanen JB, Ascierto P, Larkin J, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507–16. https://doi.org/10.1056/NEJMoa1103782.
Dallaglio K, Marconi A, Pincelli C. Survivin: a dual player in healthy and diseased skin. J Invest Dermatol. 2012;132(1):18–27. https://doi.org/10.1038/jid.2011.279.
Daniel S, Zacharias NM, Tripathi DN, Karki M, Bertocchio J, Soeung M, et al. Neddylation inhibition sensitises renal medullary carcinoma tumours to platinum chemotherapy. Clinical and Translational Medicine. 2023;13(5): https://doi.org/10.1002/ctm2.1267.
Debasish G, Ranjan A. HYPK coordinates degradation of polyneddylated proteins by autophagy. Autophagy. 2021;18(8):1763–84. https://doi.org/10.1080/15548627.2021.1997053.
Fang C, He R, Zhang L, Li H, Zhang W, Xiao J, et al. Expression of neddylation-related proteins in melanoma cell lines and the effect of neddylation on melanoma proliferation. Oncol Lett. 2014;7(5):1645–50. https://doi.org/10.3892/ol.2014.1953.
Feng JH, Nakagawa-Goto K, Lee KH, Shyur LF. A Novel Plant Sesquiterpene Lactone Derivative, DETD-35, Suppresses BRAFV600E Mutant Melanoma Growth and Overcomes Acquired Vemurafenib Resistance in Mice. Mol Cancer Ther. 2016;15(6):1163–76. https://doi.org/10.1158/1535-7163.mct-15-0973.
Flaherty KT, Infante JR, Daud A, Gonzalez R, Kefford RF, Sosman J, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N Engl J Med. 2012;367(18):1694–703. https://doi.org/10.1056/NEJMoa1210093.
Gai W, Peng Z, Liu CH, Zhang L, Jiang H. Advances in Cancer Treatment by Targeting the Neddylation Pathway. Front Cell Dev Biol. 2021;9:653882. https://doi.org/10.3389/fcell.2021.653882.
Gudbergsson JM. Extracellular vesicles for targeted drug delivery: triumphs and challenges. Future Med Chem. 2020;12(14):1285–7. https://doi.org/10.4155/fmc-2020-0117.
Gunaldi M, Isiksacan N, Kocoglu H, Okuturlar Y, Gunaldi O, Topcu TO, et al. The value of serum survivin level in early diagnosis of cancer. J Cancer Res Ther. 2018;14(3):570–3. https://doi.org/10.4103/0973-1482.171369.
Haixia F, Hu Z, Wang S, Wu W, Liu X, Geng H. 5-aminolevulinic-acid-mediated sonodynamic therapy improves the prognosis of melanoma by inhibiting survivin expression. Cancer Biomark. 2020;28(3):301–8. https://doi.org/10.3233/cbm-190681.
Harman S, Zemek R, Duncan MJ, Ying Y, Petrcich W. Efficacy of pain control with topical lidocaine-epinephrine-tetracaine during laceration repair with tissue adhesive in children: a randomized controlled trial. Can Med Assoc J. 2013;185(13):E629-634. https://doi.org/10.1503/cmaj.130269.
Hjerpe R, Thomas Y, Chen J, Zemla A, Curran S, Shpiro N, et al. Changes in the ratio of free NEDD8 to ubiquitin triggers NEDDylation by ubiquitin enzymes. Biochem J. 2012;441(3):927–36. https://doi.org/10.1042/bj20111671.
Huang X, Chen Y, Yi J, Yi P, Jia J, Liao Y, et al. Tetracaine hydrochloride induces cell cycle arrest in melanoma by downregulating hnRNPA1. Toxicol Appl Pharmacol. 2022;434:115810. https://doi.org/10.1016/j.taap.2021.115810.
İhsan H, Yeşil B, Başaran G, Sezer G, Telci D, Küçükgüzel G. Design, synthesis and anticancer activity studies of novel 4-butylaminophenyl hydrazide-hydrazones as apoptotic inducers. Tetrahedron. 2022;115:132797. https://doi.org/10.1016/j.tet.2022.132797.
Jia X, Li C, Li L, Liu X, Zhou L, Zhang W, et al. Neddylation Inactivation Facilitates FOXO3a Nuclear Export to Suppress Estrogen Receptor Transcription and Improve Fulvestrant Sensitivity. Clin Cancer Res. 2019;25(12):3658–72. https://doi.org/10.1158/1078-0432.ccr-18-2434.
Jin Y, Zhang P, Wang Y, Jin B, Zhou J, Zhang J, et al. Neddylation Blockade Diminishes Hepatic Metastasis by Dampening Cancer Stem-Like Cells and Angiogenesis in Uveal Melanoma. Clin Cancer Res. 2018;24(15):3741–54. https://doi.org/10.1158/1078-0432.ccr-17-1703.
Junhong G, Yu S, Zheng X. NEDDylation antagonizes ubiquitination of proliferating cell nuclear antigen and regulates the recruitment of polymerase η in response to oxidative DNA damage. Protein Cell. 2017. https://doi.org/10.1007/s13238-017-0455-x.
Li L, Liu B, Dong T, Lee HW, Yu J, Zheng Y, et al. Neddylation pathway regulates the proliferation and survival of macrophages. Biochem Biophys Res Commun. 2013;432(3):494–8. https://doi.org/10.1016/j.bbrc.2013.02.028.
Li Z, Pei XH, Yan J, Yan F, Cappell KM, Whitehurst AW, et al. CUL9 mediates the functions of the 3M complex and ubiquitylates survivin to maintain genome integrity. Mol Cell. 2014;54(5):805–19. https://doi.org/10.1016/j.molcel.2014.03.046.
Li L, Wang M, Yu G, Chen P, Li H, Wei D, et al. Overactivated neddylation pathway as a therapeutic target in lung cancer. J Natl Cancer Inst. 2014;106:dju083. https://doi.org/10.1093/jnci/dju083.
Li XJ, Pang JS, Li YM, Ahmed FA, He RQ, Ma J, et al. Clinical value of survivin and its underlying mechanism in ovarian cancer: A bioinformatics study based on GEO and TCGA data mining. Pathol Res Pract. 2018;214(3):385–401. https://doi.org/10.1016/j.prp.2017.12.020.
Li M, Gao F, Yu X, Zhao Q, Zhou L, Liu W, et al. Promotion of ubiquitination-dependent survivin destruction contributes to xanthohumol-mediated tumor suppression and overcomes radioresistance in human oral squamous cell carcinoma. J Exp Clin Cancer Res. 2020;39(1):88. https://doi.org/10.1186/s13046-020-01593-z.
Lirk P, Berger R, Hollmann MW, Fiegl H. Lidocaine time- and dose-dependently demethylates deoxyribonucleic acid in breast cancer cell lines in vitro. Br J Anaesth. 2012;109(2):200–7. https://doi.org/10.1093/bja/aes128.
Lirk P, Hollmann MW, Fleischer M, Weber NC, Fiegl H. Lidocaine and ropivacaine, but not bupivacaine, demethylate deoxyribonucleic acid in breast cancer cells in vitro. Br J Anaesth. 2014;113:i32-38. https://doi.org/10.1093/bja/aeu201.
Luo Z, Pan Y, Jeong LS, Liu J, Jia L. Inactivation of the Cullin (CUL)-RING E3 ligase by the NEDD8-activating enzyme inhibitor MLN4924 triggers protective autophagy in cancer cells. Autophagy. 2012;8(11):1677–9. https://doi.org/10.4161/auto.21484.
Mak CS, Yung MM, Hui LM, Leung LL, Liang R, Chen K, et al. MicroRNA-141 enhances anoikis resistance in metastatic progression of ovarian cancer through targeting KLF12/Sp1/survivin axis. Mol Cancer. 2017;16(1):11. https://doi.org/10.1186/s12943-017-0582-2.
Markus R, Leiter U, Nanz L, Amaral T, Flatz L, Garbe C, et al. Long-term survival of stage IV melanoma patients: evaluation on 640 melanoma patients entering stage IV between 2014 and 2017. Journal of Cancer Research and Clinical Oncology. 2024;150(1): https://doi.org/10.1007/s00432-023-05533-0.
McKenzie JA, Liu T, Goodson AG, Grossman D. Survivin enhances motility of melanoma cells by supporting Akt activation and α5 integrin upregulation. Cancer Res. 2010;70(20):7927–37. https://doi.org/10.1158/0008-5472.can-10-0194.
Palombo M, Deshmukh M, Myers D, Gao J, Szekely Z, Sinko PJ. Pharmaceutical and toxicological properties of engineered nanomaterials for drug delivery. Annu Rev Pharmacol. 2014;54:581–98. https://doi.org/10.1146/annurev-pharmtox-010611-134615.
Rong L, Wei J, Jiang C, Liu D, Deng L, Zhang K, et al. Akt SUMOylation Regulates Cell Proliferation and Tumorigenesis. Can Res. 2013;73(18):5742–53. https://doi.org/10.1158/0008-5472.can-13-0538.
Sanoj N, Lam E, Parija M, Prakash S, Jiramongkol Y, Adhya A, et al. NEDDylation negatively regulates ERRβ expression to promote breast cancer tumorigenesis and progression. Cell Death Dis. 2020;11(8): https://doi.org/10.1038/s41419-020-02838-7.
Soltani AE, Ganji M, Goodarzi M, Moghimi S. Cooling tetracaine to reduce pain of instillation before surgery. Eye. 2009;23(6):1470. https://doi.org/10.1038/eye.2009.75.
Sosman JA, Kim KB, Schuchter L, Gonzalez R, Pavlick AC, Weber JS, et al. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N Engl J Med. 2012;366(8):707–14. https://doi.org/10.1056/NEJMoa1112302.
Soucy TA, Smith PG, Milhollen MA, Berger AJ, Gavin JM, Adhikari S, et al. An inhibitor of NEDD8-activating enzyme as a new approach to treat cancer. Nature. 2009;458(7239):732–6. https://doi.org/10.1038/nature07884.
Taiki N, Hashimoto T, Nakashima A, Kikkawa U, Kamada S. X-linked inhibitor of apoptosis protein mediates neddylation by itself but does not function as a NEDD8–E3 ligase for caspase-7. FEBS Lett. 2012;586(11):1612–6. https://doi.org/10.1016/j.febslet.2012.04.056.
Tedore T. Regional anaesthesia and analgesia: relationship to cancer recurrence and survival. Br J Anaesth. 2015;115:ii34-45. https://doi.org/10.1093/bja/aev375.
Thomas J, Liu T, Cotter MA, Florell SR, Robinette K, Hanks AN, et al. Melanocyte expression of survivin promotes development and metastasis of UV-induced melanoma in HGF-transgenic mice. Cancer Res. 2007;67(11):5172–8. https://doi.org/10.1158/0008-5472.can-06-3669.
Tianyou W, Liu Z, Zhang Z, Tang S, Yue M, Feng S, et al. Evaluation of antitumor activity of survivin short interfering RNA delivered by lipid nanoparticles in colon cancer in vitro and in vivo. Oncology Letters. 2017;14:2001–8. https://doi.org/10.3892/ol.2017.6404.
Tingting L, Guan J, Huang Z, Hu X, Zheng X. RNF168-mediated H2A neddylation antagonizes its ubiquitination and regulates DNA damage repair. J Cell Sci. 2014. https://doi.org/10.1242/jcs.138891.
Vijayasimha K, Dolan BP. The Many Potential Fates of Non-Canonical Protein Substrates Subject to NEDDylation. Cells. 2021;10(10):2660. https://doi.org/10.3390/cells10102660.
Walden H, Podgorski MS, Huang DT, Miller DW, Howard RJ, Minor DL, et al. The structure of the APPBP1-UBA3-NEDD8-ATP complex reveals the basis for selective ubiquitin-like protein activation by an E1. Mol Cell. 2003;12(6):1427–37. https://doi.org/10.1016/s1097-2765(03)00452-0.
Wenmei C, Dong W, Wang J, Wen Z, Hao X. Elevated Expressions of Survivin and Endoglin in Patients with Hepatic Carcinoma. Cancer Biother Radiopharm. 2019;34(1):7–12. https://doi.org/10.1089/cbr.2018.2539.
Xu J, Li L, Yu G, Ying W, Gao Q, Zhang W, et al. The neddylation-cullin 2-RBX1 E3 ligase axis targets tumor suppressor RhoB for degradation in liver cancer. Mol Cell Proteomics. 2015;14(3):499–509. https://doi.org/10.1074/mcp.M114.045211.
Xuan W, Hankin J, Zhao H, Yao S, Ma D. The potential benefits of the use of regional anesthesia in cancer patients. Int J Cancer. 2015;137(12):2774–84. https://doi.org/10.1002/ijc.29306.
Xuefeng F, Li Z, Yang D, Kong X, Lu X, Shen Y, et al. 2021 Neddylation of Coro1a determines the fate of multivesicular bodies and biogenesis of extracellular vesicles. Journal of Extracellular Vesicles, 10(12): https://doi.org/10.1002/jev2.12153.
Yang MH, Mohan CD, Deivasigamani A, Chinnathambi A, Alharbi SA, Rangappa KS, et al. Procaine Abrogates the Epithelial-Mesenchymal Transition Process through Modulating c-Met Phosphorylation in Hepatocellular Carcinoma. Cancers. 2022;14(20):4978. https://doi.org/10.3390/cancers14204978.
Yao WT, Wu JF, Yu GY, Wang R, Wang K, Li LH, et al. Suppression of tumor angiogenesis by targeting the protein neddylation pathway. Cell Death Dis. 2014;5(e1059. https://doi.org/10.1038/cddis.2014.21.
Yoon JR, Whipple RA, Balzer EM, Cho EH, Matrone MA, Peckham M, et al. Local anesthetics inhibit kinesin motility and microtentacle protrusions in human epithelial and breast tumor cells. Breast Cancer Res Treat. 2011;129(3):691–701. https://doi.org/10.1007/s10549-010-1239-7.
Yuan L, Lear T, Iannone O, Shiva S, Corey C, Rajbhandari S, et al. The Proapoptotic F-box Protein Fbxl7 Regulates Mitochondrial Function by Mediating the Ubiquitylation and Proteasomal Degradation of Survivin. J Biol Chem. 2015;290(19):11843–52. https://doi.org/10.1074/jbc.M114.629931.
Zhao L, Han S, Hou J, Shi W, Zhao Y, Chen Y. The local anesthetic ropivacaine suppresses progression of breast cancer by regulating miR-27b-3p/YAP axis. Aging. 2021;13:16341–52. https://doi.org/10.18632/aging.203160.
Zhong G, Yu G, Lee H, Li L, Wang L, Yang D, et al. The Nedd8-Activating Enzyme Inhibitor MLN4924 Induces Autophagy and Apoptosis to Suppress Liver Cancer Cell Growth. Can Res. 2012;72(13):3360–71. https://doi.org/10.1158/0008-5472.can-12-0388.
Zhou L, Jiang Y, Luo Q, Li L, Jia L. Neddylation: a novel modulator of the tumor microenvironment. Mol Cancer. 2019;18(1):77. https://doi.org/10.1186/s12943-019-0979-1.
Acknowledgements
The authors would like to thank the staff and postgraduate students at Southwest Medical University for their assistance in carrying out the animal melanoma model study.
Funding
The work was supported by the National Natural Science Foundation of China (81902796), Sichuan Science and Technology Program (2022YFS0632, 2022NSFSC1594), the joint foundation of Luzhou Government and Southwest Medical University (2021LZXNYD-D08), and the Scientific Research Foundation of Southwest Medical University (2021ZKZD011).
Author information
Authors and Affiliations
Contributions
XH, PY, WG, CW and JF designed and conducted the study. XH, PY wrote the main manuscript. RZ, CW, LL, YH supervised the data collection, analyzed the data, interpreted the data. XJ and JF provided methodology, software, conceptualization, and funding acquisition.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethical Approval for Research Involving Animals at Southwest Medical University (approval number: SWMU20220028). The study was performed in accordance with the guidelines of the Institutional Animal Care and Use Committee. The maximal tumor size/burden of 20 mm was permitted by these ethics committees and the maximal tumor size/burden in this study was not exceeded.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, X., Yi, P., Gou, W. et al. Neddylation signaling inactivation by tetracaine hydrochloride suppresses cell proliferation and alleviates vemurafenib-resistance of melanoma. Cell Biol Toxicol 40, 81 (2024). https://doi.org/10.1007/s10565-024-09916-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10565-024-09916-y