Abstract
The simultaneous abuse of alcohol-cocaine is known to cause stronger and more unpredictable cellular damage in the liver, heart, and brain. However, the mechanistic crosstalk between cocaine and alcohol in liver injury remains unclear. The findings revealed cocaine-induced liver injury and inflammation in both marmosets and mice. Of note, co-administration of cocaine and ethanol in mice causes more severe liver damage than individual treatment. The metabolomic analysis confirmed that hippuric acid (HA) is the most abundant metabolite in marmoset serum after cocaine consumption and that is formed in primary marmoset hepatocytes. HA, a metabolite of cocaine, increases mitochondrial DNA leakage and subsequently increases the production of proinflammatory factors via STING signaling in Kupffer cells (KCs). In addition, conditioned media of cocaine-treated KC induced hepatocellular necrosis via alcohol-induced TNFR1. Finally, disruption of STING signaling in vivo ameliorated co-administration of alcohol- and cocaine-induced liver damage and inflammation. These findings postulate intervention of HA-STING-TNFR1 axis as a novel strategy for treatment of alcohol- and cocaine-induced excessive liver damage.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A common pattern of cocaine abuse is the simultaneous use of cocaine and alcohol (Grant and Harford 1990). An epidemiological study showed that the prevalence of alcohol use was 89% higher in cocaine-dependent patients than that in controls (without cocaine) (O'Malley and Johnston 2002). Moreover, alcohol administration increases plasma cocaine concentrations (Herbst et al. 2011). Among cocaine abusers, the estimated prevalence of comorbid alcoholism is 29%, with a lifetime prevalence reaching 62%. In contrast, comorbid alcoholism with opiate dependence has a much lower lifetime prevalence of 35%, suggesting that concurrent alcohol abuse may be an integral component of cocaine abuse (Rounsaville et al. 1991). In addition, liver damage and necrosis increased in the liver histological examination of rats fed ethanol during treatment with cocaine (Odeleye et al. 1993). As a result, alcohol may boost cocaine's bioavailability and toxicity. Reportedly, patients using alcohol and cocaine simultaneously had a higher rate of multiple hepatitis infections than those using only alcohol or cocaine (Bailey 1993). In addition, the use of cocaine and alcohol together is associated with a greater risk of sudden death than cocaine use alone (Rodriguez-Alvarez et al. 2015). However, the mechanism underlying the liver damage caused by the simultaneous use of cocaine and alcohol remains unclear.
Chronic and acute cocaine use activates certain components of the innate immune response (Sil et al. 2019), which, in turn, triggers cytotoxic processes, including alterations in cellular homeostasis in the liver, heart, and brain (Riezzo et al. 2012). Concordant with this cellular damage, several studies have shown that cocaine promotes oxidative stress in these organs, especially in the liver resulting in increased production of reactive oxygen species (ROS) (Moreira et al. 2016), leading to inflammation (Schwabe and Brenner 2006). Furthermore, the self-administration of cocaine increases the number of mitochondrial DNA (mtDNA) copies in the brain of mice (Sadakierska-Chudy et al. 2017). mtDNA acts as damage-associated molecular patterns (DAMPs) and plays an important role in inducing inflammation by activating cellular pattern recognition receptors such as stimulator of interferon genes (STING) (Abe and Barber 2014).
STING (also known as MITA and MPYS, encoded by TMEM173) are signaling molecules residing in the endoplasmic reticulum (ER) that are essential for controlling the transcription of numerous host defense genes, including type I interferons (IFNs) and pro-inflammatory cytokines (Barber 2015). STING form a complex with TBK1 upon activation through recognition of aberrant DNA species or circulating dinucleotides (CDNs) in the cytoplasm. This complex activates IFN regulatory factor 3 (IRF3) and NF-κB (Maekawa et al. 2019), and the activated NF-κB dimer enters the nucleus and transcribes pro-inflammatory factors, including interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF)-α to initiate immune effects (Abe and Barber 2014). STING is expressed and activated in nonparenchymal liver cells, including Kupffer cells (KCs) and hepatic stellate cells (HSCs) (Thomsen et al. 2016). Activation of STING in KCs and HSCs leads to inflammation (Chen et al. 2021), and the release of cytokines through inflammation triggers non-immune responses such as cell autophagy, apoptosis, and necrosis (Liu and Guan 2018). In the liver, cocaine is metabolized to benzoyl acid by cytochrome P450 3A4 (CYP3A4) (Shang et al. 2023). Benzoyl acid is converted into benzoyl-CoA via a reaction between CoA and adenosine triphosphate (ATP). Benzoyl-CoA binds to glycine to form hippuric acid (HA) (Irwin et al. 2016). Accumulating evidence has shown that HA induces mitochondrial dysfunction and apoptosis (Weigand et al. 2019). Necroptosis, a regulated necrotic cell death, is mediated by the receptor-interacting protein kinase 1 (RIP1), RIP3, and mixed lineage kinase domain-like (MLKL). Briefly, upon inhibition of caspases, RIP1 interacts with RIP3 to form a necrotic complex, which initiates necroptosis (Zhou et al. 2022) by recruiting and activating MLKL(Zhao et al. 2012). However, the role and mechanism of how cocaine-induced HA induces liver disease are not clear.
The present study aimed to elucidate the critical role of cocaine in inducing liver injury in marmosets, identify the metabolic pathways of cocaine, and investigate the associated hepatic damage. Additionally, the research sought to examine the synergistic effects of cocaine and alcohol on liver injury and inflammation, in STINGgt/gt mice. The findings of this study will provide insights into the mechanism by which cocaine and alcohol promote liver damage.
Materials and methods
Marmosets
Six (six males) common marmosets (Callithrix jacchus; weighing 280–408 g) were obtained from the Osong Medical Innovation Foundation (Chungbuk, Republic of Korea) and housed in marmoset cages [animal number/date of birth/sex (M: male): Vehicle group 1/29Jun20/M; Vehicle group 2/16Feb19/M; Vehicle group 3/21Jun18/M; Cocaine treated group 1/23Dec18/M; Cocaine treated group 2//27Jun18/M; Cocaine treated group 3/17Sep17/M; (45 × 60 × 60 cm)]. The animal room was maintained at a temperature of 27 ± 2 ℃, relative humidity of 40 ± 10% and a 12:12 h light: dark cycle (lighting 07:00–19:00, lighting ≥ 500 Lux) with 10–15 times air exchange. The animals received breeding/maintenance feed (50 g/day, NO. 0630, Altromin, Lage, Germany) prepared for marmosets and sterile tap water ad libitum from an automatic drinker. Cocaine (Cocaine hydrochloride; MacFarlan Smith Ltd., Edinburgh, UK) was administered subcutaneously for 4 weeks at 10 mg/kg. Vehicle group = Control group, Cocaine treated group = Cocaine group.
Mice
Male WT mice (11 weeks old) were purchased from Samtako Bio (Osan, Republic of Korea). Goldenticket (Tmem173 gt) mice are chemically induced mutants of the Tmem173 (Sting) protein, with a missense mutation in exon 6 that changes isoleucine to asparagine at amino acid 199. In homozygous mice, Western blot analysis of bone marrow-derived macrophages showed no detectable protein. However, these mice are viable and fertile, and their peritoneal macrophages do not produce IFN-β in response to c-di-GMP or Listeria monocytogenes infection (Sauer et al. 2011). The C57BL/6 J-Sting1gt/J(STINGgt/gt) mice were provided by Professor Chan Kim (PhD, MD, CHA University School of Medicine, Seongnam, Republic of Korea). All the mice had a C57BL/6 J background. Mice were housed in the facility maintained with a 12–12 h light–dark cycle at 21 ± 2 °C and then transferred to a specific pathogen-free facility. The laboratory maintained high pressure to prevent equipment contamination.
In the first model, WT mice (11 weeks old) were housed at 3–5 per cage. Cocaine was administered at a dose of 20 mg/kg for 10 days intraperitoneally, and saline was administered (intraperitoneally) as a vehicle. A previously published chronic binge-eating ethanol supply protocol was followed to establish an ethanol diet model(Bertola et al. 2013). Briefly, mice were fed a Lieber DeCarli Regular Control Rat Diet (NO. D710027; Dyets, Pennsylvania, USA) for the first five days as an acclimation phase. Control groups were fed a regular control rat diet, and ethanol groups were fed a Lieber DeCarli Ethanol Rat Diet (NO. D710260; Dyets, Pennsylvania, USA) containing 5–6% ethanol (NO. 041237; OCI, SEOUL, Korea) (v/v) were fed each for 10 days. On the morning of day 11, mice were administered a single dose of ethanol (5 g/kg body weight) and sacrificed 9 h later. Vehicle group = Control group, Cocaine treated group = Cocaine group, Ethanol treated group = EtOH group, Cocaine and Ethanol treated group = Cocaine + EtOH group. The second model was also established by additionally using STINGgt/gt mice under the same conditions as the first model. Vehicle group = Control group, Ethanol treated group = EtOH group, Cocaine and Ethanol treated group = EtOH + Cocaine group.
Cell culture
Immortalized mouse Kupffer cells (ImKCs) at the second passage were purchased from Applied Biological Materials Inc. (Richmond, BC, Canada), and cultured in Dulbecco's Modified Eagle's Medium (DMEM) (NO. 10–013-CVRC; Corning, Jiangsu, China) supplemented with 10% fetal bovine serum (FBS) (NO. 12003C; Sigma, Australia). Hep3B cells (in the second passage) were purchased from American Type Culture Collection (ATCC; Manassas, VA) and cultured in DMEM supplemented with 10% FBS. Cells were incubated in an atmosphere of 5% CO2 at 37 °C and treated with cocaine (250 µM) and mito-TEMPO (NO. SML0737; Sigma) (50 µM, pre-treat 1 h) for 24 h to demonstrate cocaine-induced inflammation.
Primary hepatocytes and KC isolation
To isolate primary hepatocytes, C57BL/6 J mice(10 ~ 11 weeks) were anesthetized with Zoletil (30 mg/kg; Virbac, Carros, France), and a catheter (24G) was inserted into the inferior vena cava (IVC). Livers were perfused with 30 mL EGTA solution (NO. 99,590–86-0; Sigma) maintained at 37 °C using a Masterflex L/S easy-load II (Cole-Parmer Instrument Co., IL, USA). The liver was perfused with 75 mL of enzyme buffer containing collagenase type I (650 μg/mL; Worthington Biochemicals, LA, USA) and collagenase P (50 μg/mL; Roche, Mannheim, Germany). Following this, the liver was dissected, chopped, passed through a 100 μm filter, and washed twice with enzyme buffer. Hepatocytes were then isolated and cultured in complete M199 medium (NO. 10–060-CV; Corning, NY, USA).
To isolate KC from WT and STINGgt/gt mice, the digested hepatocyte suspension was centrifuged at 57 x g for 1 min. The supernatant was then collected and centrifuged at 918 x g for 10 min to obtain the cell suspension. The cell suspension was gently covered with 70% Percoll and centrifuged at 2066 x g for 20 min in an off-brake setting. Non-parenchymal cell (NPCs) were collected, and KCs were isolated using MojoSort™ Streptavidin Nanobeads (BioLegend, San Diego, CA, USA). Isolated KCs were resuspended in RPMI 1640 medium (NO. 10–040-CV, Corning).
HA measurement
HA in the supernatant was measured using high-performance liquid chromatography (HPLC). The operation was performed on an Alliance e2695 Separations Module (Waters, MA, USA) fitted with a YMC-Pack Pro J'Sphere ODS-H80 column (300 mm × 4.6 mm, 5 μm; YMC, Seongnam, Republic of Korea). The separation was achieved using acetonitrile (A) and water (B) as the mobile phase and the following conditions: 80% A and 20% B for 10 min and 100% B for 11 min; flow rate, 1 mL/min. HA was eluted and detected at around 3.6–3.7 min at 230 nm.
Metabolomics analysis
Marmoset blood samples were collected by performing a cardiac puncture. Blood samples (60 µL) were centrifuged at 13,000 rpm for 10 min, the supernatant (20 µL) was collected, and acetonitrile (100 µL) with internal standard (L-Leusine-5,5,5-d3, 50 µg/mL) was added. The mixture was centrifuged at 13,000 rpm for 10 min; the supernatant was used to analyze metabolites using an Agilent 1290 infinity Ultra High Performance Liquid Chromatography (UHPLC) system (Agilent, Santa Clara, CA, USA) coupled with QTRAP 6500 + (hybrid triple quadrupole linear ion trap mass spectrometer) system (SCIEX, Framingham, MA, USA) and separated using a BEH Amide column (2.1 × 100 mm, 1.7 µm) (Waters, Milford, MA, USA). Mobile phases A (10 mM ammonium acetate and 0.1% acetic acid in water) and B (1 mM ammonium acetate and 0.1% acetic acid in acetonitrile) were used at a flow rate of 400 µL/min. Gradient of mobile phase were used as follows: 15% B and 85% A at 0 min, 17.5% B and 82.5% A at 3 min, 30% B and 70% A at 5.5 min, 46% B and 54% A at 7 min, 54% B and 46% A at 7.5 min, 80% B and 20% A at 9.5 min, and 85% B and 15% A at 10 min. The mass spectrometer was operated in Multiple Reaction Monitoring (MRM) in positive mode. The data were collected and analyzed using MultiQuant 3.0 and MarkerView 1.3 software (SCIEX). Metabolomics Relative change (%) was calculated as follows:
p-Toluenesulfonyl chloride colorimetric assay
Mouse blood samples were diluted tenfold with NFW, and 100 μL aliquots were placed into PCR tubes. Each tube received 20 μL of pyridine, followed by 30 μL of a 0.5 M p-TsCl solution (95.33 mg p-TsCl in 1 mL EtOH). The mixture was thoroughly combined until no solids remained visible. 100 μL of each mixture (mouse serum + pyridine) was transferred to a 96-well plate and 0.5 M p-TsCl solution was added, and the absorbance at 570 nm (A570) was measured 2 min later using a microplate reader (Bhattacharyya et al. 2023).
Mitochondrial membrane potential analysis
Mitochondrial membrane potential experiments were performed using JC-1 (5,5',6,6'-tetrachloro-1,1',3,3'-tetraethylbenzimidazolylcarbocyanine iodide) mitochondrial membrane potential assay kit (Cayman Chemical, Ann Arbor, USA). ImKC cells were cultured in the presence of cocaine (250 µM) for 24 h. Afterward, the cells were treated with JC-1 fluorescent dye at 37 °C for 20 min and washed twice with Dulbecco's phosphate buffered saline (DPBS) buffer (100 μL/mL). Fluorescence was measured using a Microplate Reader (Tecan, Männedorf, Switzerland) (red: excitation 550 nm, emission 600 nm; green: excitation 485 nm, emission 535 nm). Mitochondrial depolarization was assessed by measuring the red-to-green fluorescence ratio.
Flow cytometry
ImKC cells were treated with cocaine (250 µM) for 24 h to induce mitochondrial ROS (mtROS) production. Subsequently, the cells were stained with 5 μM MitoSox™ Red mitochondrial peroxide indicator (Invitrogen, Waltham, USA) according to the manufacturer's recommendations. After treatment, the fluorescence intensity of MitoSox™ Red was measured at 580° using a FACS Calibur flow cytometer (Guava® easyCyte™ HT System, Luminex, Austin, USA). Data were analyzed using the Guavasoft software (Luminex, Austin, USA).
Cytotoxicity analysis
Isolated primary hepatocytes were cultured in collagen-coated 12-well plates (2 × 105 cells/well) in filtered M199 medium supplemented with 10% FBS and 1% antibiotic and antifungal agents (Gibco, NY, USA). After 3 h, the medium was replaced with KC-derived conditioned medium (CM) without FBS. After incubation for 24 h, the medium was collected for further analysis. Cytotoxicity was measured using a Quanti-LDH™ Cytotoxicity assay kit (Biomax, Seoul, Republic of Korea).
mtDNA copy number analysis
DNA was isolated from ImKC cells using the MagMAX Cell-Free DNA (cfDNA) Isolation kit (Invitrogen). The DNA was subjected to real-time polymerase chain reaction (PCR) in a CFX Connect Real-Time PCR Detection System (Bio-Rad, Hercules, CA, USA) using SYBR qPCR master mix (TB Green, TAKARA Bio, Kusatsu, Japan) to determine the mtDNA/nuclear DNA ratio to determine the number of mtDNA copies. The primers for real-time PCR are listed in Table S2.
Small interfering RNA (siRNA) transfection
Primary hepatocytes were cultured to 30–50% confluence in 6-well culture dishes. Commercially available mouse scrambled siRNA (IDT, Coralville, IA, USA) and TNFR1 siRNA (IDT, Coralville, IA, USA) were transfected into the cells using Lipofectamine® 3000 (Thermo Fisher Scientific Inc., Waltham, CA, USA) according to the manufacturer's instructions.
Enzyme-linked immunoassay (ELISA)
Protein levels of TNF-α and IL-1β after stimulation with cocaine in ImKC cells for 0, 3, 6, 12, and 24 h were determined using ELISA. The ELISA was performed using Mouse TNF-alpha DuoSet and Mouse IL-1 beta/IL-1F2 DuoSet (DY401, R&D Systems, Minneapolis, Minnesota, USA) kits according to the manufacturer's instructions. The absorbance was measured at 450 and 540 nm using a microplate reader (VersaMax Absorbance Microplate Reader, Molecular Devices). Absorbance was calculated by subtracting the absorbance at 540 nm from that at 450 nm. A four-parameter regression analysis was used to create a standard curve.
Quantitative real-time PCR analysis
Cells and liver tissues were homogenized using RiboEx (NO. 301–001). RNA was isolated from the cells and liver tissues using a Hybrid-R RNA extraction kit (Gene All Biotechnology, Seoul, Republic of Korea). Reverse transcription was performed using RNase-free DNase I (Promega, Madison, WI, USA) and a Capacity cDNA Reverse Transcription Kit (Applied Biosystems, FC, USA) according to the manufacturer's instructions. cDNA was subjected to real-time PCR using a CFX Connect Real-Time PCR Detection System (Bio-Rad) and SYBR qPCR master mix (TB Green)—the primers used are listed in Table S2. Quantification was performed by normalizing the expression of the target gene to that of glyceraldehyde 3-phosphate dehydrogenase (Gapdh; internal control).
Western blot analysis
ImKC cells, primary hepatocytes, and liver tissues were homogenized in RIPA buffer. The lysates were centrifuged at 13,000 rpm for 15 min at 4 °C. Protein concentration in the supernatant was measured using a BCA Protein Assay Kit (Thermo Fisher Scientific Inc.). Equal protein amounts were separated by 10% SDS-PAGE and transferred to a PVDF membrane. The membrane was blocked with 5% skim milk for 1 h at 21–23 °C and with 5% BSA, then incubated overnight at 4 °C. The membrane was then incubated with primary antibodies (1:1000) overnight at 4 °C, followed by secondary antibodies conjugated with horseradish peroxidase at room temperature for 1 h. All antibodies were diluted in Tris-buffered saline/Tween with 2% BSA.
KC conditioned medium (CM) delivery experiment
KCs (2.5 × 105 per well) were incubated in 6-well plates with or without cocaine (250 µM) for 24 h. The KCs supernatant was harvested with pipet, and the remaining cells were pelleted at 600 × g for 5 min, then transferred to hepatocytes (2.5 × 105) in a 6-well plate and incubated at 37 °C. for 24 h.
Biochemical analysis
Mouse blood samples were collected via cardiac puncture and centrifuged at 13,000 rpm for 15 min to obtain serum. AST and ALT levels in the serum were analyzed using a biochemical analyzer (KP&T, Osong, Republic of Korea), while AMY, ALP, and LIPA levels were measured using an Exdia PT10V (Precision Biosensor, Daejeon, Republic of Korea). Marmoset blood samples were taken immediately before the first and after the last cocaine self-administration session, as well as during two consecutive instances of stereotyped behaviors. Blood was collected in EDTA- or heparin-treated tubes (approximately 24 h after cocaine administration), centrifuged at 2,000 × g for 15 min at 4 °C, and the plasma was transferred to microtubes and stored at − 80 °C until analysis.
Histopathological analysis of liver
To collect livers, mice were anesthetized with Zoletil (30 mg/kg). The extracted liver tissues were cleaned, fixed in formalin, and embedded in paraffin. Tissue blocks were cut into 5 μm-thick sections and stained with hematoxylin and eosin (H&E) (NO. 3,801,698, Leica Biosystems). To confirm hepatocyte necrosis, terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) staining was performed using ApopTag® Plus Peroxidase in Situ Apoptosis Kit (NO. S7101, Millipore, Burlington, USA).
Statistical analysis
All data are expressed as the mean ± standard error of the mean (SEM). Statistical analysis by t-test was performed using GraphPad Prism 8 software (GraphPad Software Inc., San Diego, CA, USA). Statistical significance was set at p < 0.05. made available on request.
Results
Cocaine leads to liver damage and inflammation in marmosets
We injected marmosets with cocaine to determine whether cocaine induces liver inflammation and hepatocyte necrosis. Cocaine treatment decreased average weight gain in marmosets. The average weight gain in the control (Con) group was approximately 13.3%. However, cocaine administration resulted in a weight loss of approximately 10% (Fig. 1A). Cocaine increased AST, ALT, and ALP levels by approximately 1.2 to 1.5 times on average, but these changes were not statistically significant. However, it significantly increased the serum levels of LIPA and AMY (Fig. 1B). This suggests that reduced metabolism due to cocaine-induced liver damage leads to the accumulation of AMY and LIPA in blood (Pezzilli et al. 1999). Additionally, cocaine administration increased hepatic inflammation as demonstrated by the increased expression of TNF-α, IL-1β, and IL-6 mRNA in the liver (Fig. 1C). Histopathological analysis revealed cocaine-induced balloon degeneration and hepatocyte death (Figs. 1D and E). Together, these results demonstrate that cocaine induces hepatic apoptosis in marmosets. The marmoset hepatocytes were treated directly with cocaine in vitro to confirm the HA produced by cocaine. To measure HA, a calibration was performed using an HA standard (R2 = 0.9998) (Figures S1A and B). The recovery rate was 89.24% (Figure S2A). HA production increased in a concentration-dependent manner in vitro, with levels more than 11 times higher at the highest concentration of 125 µM compared to the untreated group (Fig. 1F). Furthermore, the metabolic analysis revealed most significant increase in HA levels in the cocaine-treated group compared to that in the control group (Fig. 1G). These data demonstrate that cocaine abuse exacerbates liver damage and inflammation in marmoset species and that cocaine is converted to HA in marmoset hepatocytes and released into the serum (Fig. 1H).
Cocaine leads to liver damage and inflammation in marmosets. Cocaine (10 mg/kg) was administered intraperitoneally to the marmosets for four weeks until the animals were sacrificed. (A) Body weight changes were measured weekly; n = 3, Con group; n = 3, Cocaine group. (B) Serum ALP, LIPA, and AMY levels; n = 3, Con group; n = 3, Cocaine group. (C) IL-1β and TNF-α mRNA levels in liver tissue. mRNA levels were measured using qRT-PCR and expressed as fold change compared to control marmosets. Relative mRNA expression of target genes was normalized to that of marmoset GAPDH; n = 3, Con group; n = 3, Cocaine group. Representative images of liver pathology with (D) H&E and (E) TUNEL staining were acquired at 200x. (F) HA metabolite concentrations measured using HPLC of subsamples from marmoset hepatocytes supernatant treated with various concentrations (31.25, 62.5, and 125 µM) of Cocaine for 24 h; n = 3 per group. (G) Metabolomics analysis of marmoset serum was performed using an Agilent 1290 infinity UHPLC system; n = 6 per group. These show the relative content of various classes of metabolites. (H) Schematic of cocaine metabolism. Data are presented as mean SEM. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001
Cocaine and ethanol induce hepatocyte death and liver inflammation in mice
To determine whether the combined administration of cocaine and alcohol causes worse liver damage, mice were administered cocaine and ethanol diet for 10 days. Combined treatment with cocaine and ethanol showed significant reductions in body and liver weight compared to treatment with cocaine and alcohol alone (Figs. 2A and B). Serum levels of AST, ALT also suggest that combined administration of cocaine and ethanol induces more severe liver damage than individual treatment (Fig. 2C). Likewise, mRNA of inflammatory cytokines and chemokines showed similar trend with other data, showing significant increment of TNF-α, C–C motif chemokine ligand 3 (CCL3), C-X-C motif chemokine Ligand 10 (CXCL10) in co-treatment group (Fig. 2D). Histopathological analysis showed that hepatocyte ballooning and the number of TUNEL-positive cells were significantly increased in the combined treatment with cocaine and ethanol (Figs. 2E-G). To measure HA, calibration was performed using the HA standard (R2 = 0.9518) (Figure S2B). In the cocaine group, HA levels were approximately three times higher compared to the untreated group, while the additional administration of EtOH did not result in a significant increase (Fig. 2H). These results suggest that the combination of ethanol and cocaine dramatically exacerbates hepatocyte death and liver inflammation in mice without significantly altering HA production.
Cocaine and ethanol induce hepatocyte death and liver inflammation in mice. Mouse (n = 28) were divided into four groups. EtOH group was fed an ethanol diet for 10 days and the Cocaine group were intraperitoneally administered cocaine (20 mg/kg) along with an ethanol diet for 10 days; n = 7, Con group; n = 7, EtOH group; n = 8, Cocaine group; n = 6, EtOH + Cocaine group. (A) Body weight and (B) liver weight changes were measured daily for 10 days; n = 7, Con group; n = 7, EtOH group; n = 8, Cocaine group; n = 6, EtOH + Cocaine group. (C) Serum AST and ALT levels; n = 7, Con group; n = 7, EtOH group; n = 8, Cocaine group; n = 6, EtOH + Cocaine group. (D) mRNA levels of IL-1β, IL-6, TNF-α, CCL2, CCL3, and CXCL10 in liver tissue were measured using qRT-PCR. Relative mRNA expression levels of target genes were normalized to that of mouse Gapdh; n = 7, Con group; n = 7, EtOH group; n = 8, Cocaine group; n = 6, EtOH + Cocaine group. Hepatic histopathological analysis was performed using (E) H&E staining and (F and G) TUNEL staining; n = 6 per group. Representative images were acquired at 200x magnification. (H) Cocaine (20 mg/kg) was administered intraperitoneally to the mice for 10 days. Serum was drawn, diluted 10 times with water, and analyzed by p-Toluenesulfonyl chloride colorimetric assay; n = 7, Con group; n = 7, EtOH group; n = 8, Cocaine group; n = 6, EtOH + Cocaine group. Data are presented as mean ± standard error of the mean (SEM). * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001; # p < 0.05, ## p < 0.01, ### p < 0.001, #### p < 0.0001
Cocaine-derived HA and cocaine increase mitochondrial DNA leakage and subsequent inflammation in KCs
HA is known to cause oxidative stress in kidney cells at concentrations of 125uM to 1000uM (Sun et al. 2020). We evaluated mitochondrial damage and inflammation induced by HA in KCs. HA decreased the expression of mitochondrial transmembrane potential proteins, including heat shock protein 60 (HSP60), translocase of the outer mitochondrial membrane 40 (TOM40), and translocase of the inner mitochondrial membrane 23 (TIM23) by more than 50% (Fig. 3A). Treatment of ImKC with various concentrations (0, 62.5, 125, and 250 µM) of HA increased mtROS production (Fig. 3B). Additionally, HA increased the leakage of mtDNA into the cytoplasm of ImKC cells by 1.5 times (Fig. 3C). HA induced a significant decrease in mitochondrial membrane potential (Fig. 3D), suggesting that HA causes mitochondrial damage. Furthermore, HA treatment over various periods (24 h and 48 h) resulted in a 2- to 15-fold increase in mRNA levels of inflammatory cytokines (TNF-α, IL-1β) and chemokines (CCL2, CCL3) in ImKC cells (Fig. 3E).
Cocaine-derived HA and cocaine increase mitochondrial DNA leakage and subsequent inflammation in KCs. (A) HSP60, TOM40, TIM23, and ACTIN expression analyzed using western blot analysis. ImKC cells were treated with HA (250 µM) for 24 h; n = 3 per group. (B) MitoSOX was measured in ImKC cells after treatment with various concentrations (62.5, 125, and 250 µM) of HA for 24 h; n = 4 per group. (C) mtDNA copy number after HA stimulation (250 µM, 24 h) in ImKC cells assessed using RT-PCR; n = 4 per group. (D) ImKC cells were treated with HA (250 µM) for 24 h. Mitochondrial membrane potential was determined using JC-1 staining. The red: green fluorescence ratio was used to quantify the mitochondrial membrane potential; n = 4 per group. (E) TNF-α, IL-1β, CCL2, and CCL3 mRNA levels in ImKC cells. ImKC cells were treated with HA (250 µM) for 24 and 48 h. Relative mRNA expression of target genes was normalized to that of mouse Gapdh; n = 3 per group. (F) HSP60, TOM40, TIM23, and ACTIN expression analyzed using western blot analysis after treatment with cocaine; n = 3 per group. (G) MitoSOX was measured in ImKC cells after treatment with various concentrations (31.25, 62.5, and 250 µM) of cocaine for 24 h; n = 3 per group. (H) mtDNA copy number after cocaine stimulation (250 µM, 24 h) in ImKC cells assessed using RT-PCR; n = 3 per group. (I) ImKC cells were treated with cocaine (250 µM) for 24 h. Mitochondrial membrane potential was determined using JC-1 staining. The red: green fluorescence ratio was used to quantify the mitochondrial membrane potential; n = 3 per group. (J) TNF-α, IL-1β, CXCL10, IFN-α, and IFN-β were measured using qRT-PCR, and relative mRNA expression of target genes was normalized to that of mouse Gapdh; n = 4 per group. Data are presented as mean ± SEM. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001
Interestingly, cocaine decreased mitochondrial membrane protein (Fig. 3F) and increased mtROS production (Fig. 3G) and mtDNA leakage (Fig. 3H). Cocaine induced a significant decrease in mitochondrial membrane potential (Fig. 3I). This suggests that cocaine, like HA, causes mitochondrial damage. Similarly, cocaine treatment increased the mRNA levels of pro-inflammatory cytokines (TNF-α, IL-1β), chemokine (CXCL10), and type I interferons (IFN-α, IFN-β) in ImKCs by 1.5 to 7 times (Fig. 3J). Collectively, these results suggest that HA and cocaine cause mitochondrial dysfunction and inflammation.
Cocaine-derived HA and cocaine promote mitochondrial damage and STING signaling
Previous studies have shown that mitochondrial damage causes inflammation via cyclic GMP-AMP synthase (cGAS)-STING signaling (Krokos et al. 2021). Therefore, we assessed the effects of cocaine-derived HA and cocaine on the STING pathway. HA (250 µM) increased STING protein expression and phosphorylation of TBK1 downstream of STING and upregulated NF-κB phosphorylation. The activation of this cGAS-STING signal was blocked by the STING inhibitor (C-176) in ImKCs (Fig. 4A). Furthermore, HA increased the expression of STING and cGAS and pro-inflammatory cytokines and chemokines (TNF-α, IL-1β, CCL2, CCL3) in mouse KCs, and these effects diminished in STINGgt/gt mouse KCs (Fig. 4B). Consistent with HA, cocaine also increased STING signal, and this increase in STING signal was blocked by C-176 (Fig. 4C).
Cocaine-derived HA and cocaine promote mitochondrial damage and STING signaling. (A) STING, pTBK1, TBK1, pNF-κB, NF-κB, and ACTIN expression analyzed using western blot analysis. ImKC cells were treated with HA (250 µM) and C-176 (STING inhibitor; 750 nM) for 24 h; n = 3 per group. (B) mRNA expression of STING, cGAS, TNF-α, IL-1β, CCL2, and CCL3 in KC isolated from WT and STING-deficient mice. mRNA levels were measured using qRT-PCR and expressed as fold changes compared to that of the control. Relative mRNA expression of target genes was normalized to that of mouse Gapdh; n = 3 per group. (C) STING, pTBK1, TBK1, pNF-κB, NF-κB, and ACTIN expression analyzed using western blot analysis. ImKC cells were treated with Cocaine (250 µM) and C-176 (STING inhibitor; 750 nM) for 24 h; n = 3 per group. (D) ImKC cells were cultured for 24 h after treatment with cocaine (250 µM) and mito-TEMPO (50 µM, pre-treat 1 h). TNF-α, IL-1β, CCL2, and CCL3 were measured using qRT-PCR and relative mRNA expression levels of these genes were normalized to that of mouse Gapdh levels; n = 4 per group. (E) Cocaine (250 µM, 24 h)-induced expression of STING, TNF-α, IL-1β, CCL3, and CXCL10 in KC isolated from WT mice and STINGgt/gt mice measured using qRT-PCR. Relative mRNA expression levels of the target genes were normalized to that of mouse Gapdh levels; n = 4 per group. Data are presented as mean ± SEM. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001; # p < 0.05, ## p < 0.01, ### p < 0.001, #### p < 0.0001
To clarify whether cocaine-induced mtROS production mediated liver inflammation, we investigated the effect of mito-TEMPO, a mitochondria-targeted superoxide dismutase with mimetic superoxide scavenging properties. Mito-TEMPO significantly reduced the mRNA levels of cocaine-induced pro-inflammatory cytokines and chemokines (TNF-α, IL-1β, CCL2, CCL3) (Fig. 4D). Furthermore, the cocaine-induced increase in the expression of the pro-inflammatory cytokines and chemokines mRNAs (TNF-α, IL-1β, CCL3, CXCL10) in KCs were reduced in STING-deficient KCs (Fig. 4E). These results demonstrate that HA- and cocaine-induced inflammation is mediated by STING signaling in KCs.
Cocaine-mediated TNF-α enhances hepatocyte necroptosis
Various cytokines are known to induce hepatocyte death(An et al. 2012). Therefore, we aimed to determine whether cocaine-induced KC-derived cytokines induce hepatic apoptosis. Indeed, in the conditioned media (CM) of ImKC cells treated with cocaine for 24 h, TNF-α protein levels increased more than threefold, and IL-1β protein levels increased more than 20-fold (Fig. 5A). Our study measured hepatocyte cytotoxicity of ImKCs cultured 1 day in CM for 0, 1, 2, and 3 days. As a result, there was no significant difference, suggesting that the CM-1 days used in our experiment had no toxicity that affected the experimental results (Figure S3). Additionally, to confirm that cocaine does not directly affect liver cells, we directly treated liver cells with cocaine and found that there was no toxic effect at 250uM (Figure S4A). Measurement of the cytotoxicity in primary hepatocytes cultured in the CM of cocaine-treated KCs exhibited increased cytotoxicity in primary hepatocytes in a time-dependent manner (Fig. 5B). Furthermore, analysis of the expression of key markers of apoptosis showed that KC-derived CM did not induce the expression of cleaved caspase-3. No change was observed in bcl-2-like protein 4 (Bax) or B-cell lymphoma 2 (Bcl2) expression (Fig. 5C and D); these results show that cell death is not mediated by apoptosis. Nevertheless, the mRNA expression of RIP1 and RIP3, the major biomarkers of cell necroptosis, were significantly upregulated by CM in hepatocytes (Fig. 5E). In addition, the CM from cocaine-treated KCs upregulated MLKL and RIP3 phosphorylation in hepatocytes in a time-dependent manner after cocaine treatment (Fig. 5F). These results suggest that necroptosis is involved in cocaine-induced cell death. Because TNF and TNFR1 signaling have been suggested to be major pathways involved in necroptosis (Shalini et al. 2015), we investigated the effects of TNFR1 knockdown on CM-induced cytotoxicity. The results showed that knocking down TNFR1 by more than 90% blocked CM-induced cytotoxicity (Figs. 5G and H). In addition, the CM-induced phosphorylation of RIP3 and MLKL decreased following the TNFR1 knockdown (Fig. 5I). These findings suggest that cocaine-mediated paracrine regulation of hepatocyte necroptosis depends on TNFR1 signaling.
Cocaine-mediated TNF-α enhances hepatocyte necroptosis. (A) Protein levels of TNF-α and IL-1β after stimulation with cocaine in ImKC cells for 0, 3, 6, 12, and 24 h were determined using ELISA; n = 3 per group. (B) Primary hepatocytes were cultured for for 0, 3, 6, 12, and 24 h after treatment with KC-derived CM. Cytotoxicity was measured using lactate dehydrogenase (LDH) assay via microplate leader; n = 3 per group. (C and D) Western blotting was performed to evaluate the protein levels of caspase3, Bax, Bcl-2, and ACTIN; n = 2 per group. (E) RIP1 and RIP3 mRNA levels were measured using qRT-PCR. Relative mRNA expression levels of target genes were normalized to that of mouse Gapdh; n = 2 per group. (F) RIP3 and MLKL phosphorylation assessed using western blotting. Primary hepatocytes were cultured treatment with KC-derived CM for 0, 3, 6, 12, and 24 h after. (G) mRNA expression of TNFR1 measured using qRT-PCR in primary hepatocytes; n = 4 per group. (H) Primary hepatocytes were cultured for 24 h after treatment with KC-derived CM and transfected with TNFR1 siRNA and scrambled siRNA control. Cytotoxicity was measured using LDH assay via microplate leader; n = 3 per group. (I) Primary hepatocytes were cultured for 24 h after treatment with KC-derived CM and transfected with TNFR1 siRNA and scrambled siRNA control. RIP3 and MLKL phosphorylation assessed using western blotting; n = 2 per group. All data are presented as mean ± SEM. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001. # p < 0.05, ## p < 0.01, ### p < 0.001, #### p < 0.0001
Alcohol increases TNFR-1 expression in hepatocytes and enhances susceptibility to cocaine-mediated hepatic necroptosis
The liver is the main organ responsible for the metabolism of ingested alcohol. therefore, it is most susceptible to alcohol-related damage (Yu et al. 2010). Ethanol impairs mitochondrial energy metabolism and enhances ROS formation (Mansouri et al. 1999). Our study confirmed that alcohol increased hepatocyte cytotoxicity and damaged the mitochondria (Figure S5). Based on these previous studies, we sought to determine whether the co-administration of ethanol and cocaine increases liver damage. Hepatocyte cytotoxicity was increased by co-administration of ethanol and CM from cocaine-treated KCs increased compared with that by administration of CM from cocaine-treated KC alone (Fig. 6A). In addition, in KCs treated with cocaine, the combined administration of ethanol and CM resulted in a twofold increase in RIP3 mRNA expression, and the necrosis marker phospho-MLKL protein expression compared to CM derived from cocaine-treated KCs (Figs. 6B and C). Patients with alcoholic liver disease showed increased expression of TNFR1 in previous studies (Ma et al. 2020), alcohol increased the expression of TNFR1 in hepatocytes by more than tenfold in our study (Fig. 6D). This suggests that the alcohol-induced increase in TNFR1 expression increases hepatocyte necroptosis. Next, we performed TNFR1 knockdown in hepatocytes to confirm that hepatocellular necroptosis by cocaine and alcohol co-use occurs via TNFR1 signaling. Simultaneous treatment with ethanol and cocaine-treated medium significantly increased hepatocellular cytotoxicity compared to treatment with cocaine-treated medium alone, and TNFR1 knockdown downregulated cytotoxicity (Fig. 6E). Furthermore, we confirmed the phosphorylation of RIP3 and MLKL, which are the major biomarkers of necroptosis. Ethanol- and cocaine-treated media increased the phosphorylation of RIP3 and MLKL, whereas TNFR1 knockdown downregulated the phosphorylation of RIP3 and MLKL (Figs. 6F and G). These results demonstrated that alcohol increased the expression of TNFR1 in hepatocytes and that the simultaneous use of alcohol and cocaine further increased cocaine-induced TNF-α-mediated hepatocellular necroptosis.
Alcohol increases TNFR-1 expression in hepatocytes and enhances susceptibility to cocaine-mediated hepatic necroptosis. Primary hepatocytes were treated with cocaine-treated KC-derived CM in the presence of ethanol (50 µM) and then cultured for 24 h. (A) Cytotoxicity was measured using LDH assay; n = 3 per group. (B) mRNA expression of RIP3 was measured using qRT-PCR. Relative mRNA expression of target genes was normalized to that of mouse Gapdh; n = 5 per group (C) Western blotting was performed to evaluate the phosphorylation of MLKL; n = 2 per group (D) Primary hepatocytes were cultured for 24 h in the presence of ethanol (50 µM). The level of mRNA of TNFR1 was measured using qRT-PCR. Relative mRNA expression level of Tnfr1 was normalized to that of mouse Gapdh; n = 3 per group. (E) Primary hepatocytes were transfected with TNFR1 siRNA and scrambled siRNA (negative control). Cytotoxicity was assessed by measuring LDH levels; n = 3 per group (F and G) Western blot was performed to evaluate the phosphorylation of RIP3 and MLKL; n = 3 per group. All data are presented as mean ± SEM. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001. # p < 0.05, ## p < 0.01, ### p < 0.001, #### p < 0.0001
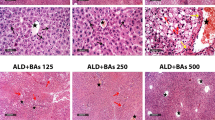
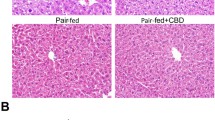
STING regulates cocaine and alcohol-induced liver injury and inflammation
To investigate the role of STING in vivo, we established a model of cocaine- and alcohol-induced liver injury using STINGgt/gt and WT mice. Simultaneous administration of ethanol and cocaine increased serum AST and ALT levels in WT mice. In contrast, STING deletion significantly reduced serum AST and ALT levels compared with those in WT mice (Fig. 7A). Compared with the ethanol diet, the reduced inflammation level by the simultaneous use of ethanol diet and cocaine was confirmed through the mRNA levels of STING, TNF-α, IL-1β, CCL2, and CXCL10 in STINGgt/gt mice (Fig. 7B). To understand how ethanol diet and cocaine induce inflammation, downstream STING was investigated in the livers of WT and STINGgt/gt mice. Simultaneous administration of the ethanol diet and cocaine increased the protein expression of STING and phosphorylation of TBK-1 and NF-κB in WT mice. In contrast, the deletion of STING downregulated the phosphorylation of these proteins (Fig. 7C). This finding indicated that cocaine-induced liver inflammation increased when co-administered with ethanol, suggesting that it proceeds via STING signaling. Next, we attempted to confirm hepatocyte necroptosis caused by the simultaneous use of alcohol and cocaine through histopathological examination. As confirmed by H&E staining and an increase in TUNEL-positive cells, co-administration of the ethanol diet and cocaine increased hepatocyte necroptosis compared with that induced by the ethanol diet alone. In contrast, STING knockdown downregulated hepatocyte necroptosis (Figs. 7D and E). Moreover, hepatocyte necroptosis induced by the combination of the ethanol diet and cocaine was confirmed by increased phosphorylation of RIP3 and MLKL, whereas STING deletion ameliorated hepatocyte necroptosis (Fig. 7F). These data suggest that STING deletion alleviates liver inflammation caused by the simultaneous use of alcohol and cocaine, which may improve hepatocyte necroptosis. Deletion of STING reduces TNF-α secretion in comorbid alcohol and cocaine abuse, suggesting that TNF-α-induced hepatocytes necroptosis can be improved. Taken together, the combination of alcohol and cocaine induces liver inflammation via STING signaling, which may lead to TNF-α-induced hepatocyte necroptosis.
STING regulates cocaine and alcohol-induced liver injury and inflammation. WT (n = 17) and STINGgt/gt (n = 17) mice were divided into three groups: Control (Con, n = 5), Ethanol (EtOH, n = 5), and Ethanol + Cocaine (EtOH + Cocaine, n = 7). The Ethanol and Ethanol + Cocaine groups were fed an ethanol diet for 10 days. Additionally, these mice were administered a single dose of ethanol (5 g/kg body weight). The Ethanol + Cocaine group was also intraperitoneally administered cocaine (20 mg/kg) along with the ethanol diet for 10 days. Additionally, these mice were administered a single dose of ethanol (5 g/kg body weight). (A) Serum AST and ALT levels (B) mRNA levels of STING, TNF-α, IL-1β, CCL2, and CXCL10 in liver tissue were measured using qRT-PCR. Relative mRNA expression levels of target genes were normalized to that of mouse Gapdh (C) TBK1, pTBK1, NF-κB, pNF-κB, and STING in the liver tissue analyzed using western blotting; n = 2 per group. Hepatic histopathological analysis was performed using (D) H&E staining and (E) TUNEL staining Representative images were acquired at 200x magnification. (F) RIP3 and MLKL phosphorylation in liver tissue assessed using western blotting; n = 2 per group. All data are presented as mean ± SEM. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001. # p < 0.05, ## p < 0.01, ### p < 0.001, #### p < 0.0001
Discussion
The present study explores the effects of co-administration of alcohol and cocaine, a common pattern of cocaine abuse, on liver damage and sheds light into the underlying mechanisms. Because primates have fewer genetic differences from humans than rodents, we established a cocaine administration plan in marmosets for a more clinical approach (Cardoso-Moreira et al. 2020). Cocaine-administered marmosets exhibited gradual weight loss, increased liver damage, and pro-inflammation, indicating that cocaine causes liver inflammation and damage in rodents and primates. Kupffer cells are generally less involved in drug metabolism compared to hepatocytes. Their primary functions are immune response and inflammation regulation, though some studies suggest that Kupffer cells may also participate in drug metabolism (Ding et al. 2004). Compared to Kupffer cells, hepatocytes exhibit high expression of cytochrome P450 2E1 (CYP2E1), playing a crucial role in the metabolism of various drugs and toxins. Hepatocytes typically express multiple cytochrome P450 enzymes, including CYP2E1, essential for metabolic processes. In contrast, Kupffer cells have inherently low CYP2E1 expression, which can be significantly induced by substances like acetone. Once induced, Kupffer cells also contribute to the metabolism of exogenous substances in the liver (Koop et al. 1991). However, this involvement is relatively minor compared to the metabolic processes occurring in hepatocytes (Zhong et al. 1994) Theoretically, cocaine is metabolized to HA in the liver (Krokos et al. 2021). However, to our knowledge, the measurement of HA has not been assessed in vivo (Cone et al. 1998). Metabolic analysis revealed the highest levels of the cocaine metabolite, HA, in the serum of cocaine-administered marmosets. In this study, we quantified HA using HPLC after administering cocaine to marmoset hepatocytes. In marmoset hepatocytes treated with 125 µM of cocaine, HA levels increased more than tenfold compared to the untreated group.
Generally, people consume cocaine together with ethanol (Grant and Harford 1990), and we established a cocaine and ethanol co-administration model to evaluate the risk of consuming cocaine and ethanol. Furthermore, the administration of cocaine concurrently with or after alcohol has been shown to increase blood cocaine levels by up to 30% compared to the administration of cocaine alone (Pennings et al. 2002). In this model, although we did not measure alcohol and acetaldehyde levels during necrosis, it is well known that alcohol is converted to acetaldehyde by ADH and then metabolized to acetic acid by ALDH during alcohol consumption. Cocaine interferes with alcohol metabolism, leading to increased accumulation of acetaldehyde, thereby enhancing toxicity. Furthermore, the combination of cocaine and alcohol forms a toxic metabolite called cocaethylene. These characteristics suggest that cocaine disrupts alcohol metabolism and promotes the accumulation of toxic metabolites, thereby increasing necroptosis (Gossop et al. 2006; Singh 2019). In addition, the combined administration of alcohol and cocaine led to a more severe increase in liver damage (AST, ALT) than the administration of alcohol and cocaine alone and even induced the activation of pro-inflammatory factors (IL-1β, TNF-α, CCL3, CXCL3). Hepatocyte ballooning and TUNEL-positive cell area, which are indicators of liver damage, also increased. This shows that the synergistic effect of combining alcohol and cocaine has been proven to cause serious liver damage. Additionally, like the marmoset model, the group of mice administered cocaine for 10 days showed an average HA concentration of 150 µM, which was more than 3 times higher than that of the untreated group. This demonstrated that cocaine is metabolized to HA in hepatocytes. HA is involved in mitochondrial dysfunction and oxidative stress (Deng et al. 2021). Our results also showed a reduction in mitochondrial protein levels and an increase in mtROS levels. Given that mitochondrial dysfunction and oxidative stress can contribute to STING signaling, we hypothesize that HA enhances pro-inflammation by inducing the accumulation of mtROS to activate STING signaling. Consistent with the previously reported results, our results demonstrated an inflammatory effect of cocaine on KCs activation via the HA-mediated STING-TBK1-NFKB axis. Cocaine-induced mtROS increases pro-inflammation by activating STING-TBK1-NFKB signaling. This study demonstrated that cocaine and the cocaine metabolite HA induce liver inflammation, leading to mitochondrial damage in KCs. Collectively, our findings highlight that cocaine and HA-mediated inflammation are important factors in regulating pro-inflammatory cytokine (TNF-α, IL-1β) and chemokine (CCL2, CCL3) secretion through the regulation of STING signaling. Several lines of evidence support the mechanism by which cocaine- and HA-induced liver inflammation via STING signaling induce hepatocyte necrosis via TNFR signaling. First, the induction of mitochondrial damage by cocaine and HA in KCs in our study is consistent with previous studies indicating that oxidative stress is involved in the mechanism of cocaine- and HA-induced liver damage and that this process involves mitochondrial modifications (Vitcheva 2012). Second, our study showed that cocaine increased the mtDNA copies and induced liver inflammation after STING activation. We isolated KCs from WT and STINGgt/gt mice and observed cocaine- and HA-induced inflammation. These findings are consistent with those of previous reports showing that mtDNA is recognized as an endogenous DAMP when released into the cytoplasmic and extracellular environments, activating the innate immune response, and promoting inflammation (Yu et al. 2019).
To clarify whether the cocaine-induced liver injury occurred through the interaction of KC with hepatocytes, we investigated cocaine-induced hepatocyte damage. Before that, we conducted a toxicity evaluation to distinguish the suitability of the CM model derived from the ImKCs we used. There was no significant difference from the control in the CM derived from ImKCs, proving that the model was suitable for use. Furthermore, cocaine did not significantly increase liver cytotoxicity. Similarly, we showed that cocaine might not directly induce changes in hepatocyte membrane potential, mtROS production, or mitophagy (Figure S4). Therefore, we prove that cocaine-induced liver injury is mediated by KC-induced liver inflammation. In this study, hepatocyte cytotoxicity was measured to examine the effect of alcohol on hepatocytes, which revealed that alcohol exposure increased hepatocyte cytotoxicity in a dose-dependent manner (Figure S5A). Moreover, alcohol significantly downregulated the mitochondrial membrane potential and attenuated TIM23 expression in hepatocytes (Figures S5B and C) and increased mtROS levels (Figure S5D). Hepatocellular necrosis is a major etiological phenomenon of alcoholic liver disease (Mansouri et al. 1999). In this study, we showed that alcohol treatment also increased the phosphorylation of MLKL, a key biomarker of necroptosis (Figure S5E). Consistent with a previous study (Xue et al. 2020), we showed that cocaine- and HA-induced TNF-α induces hepatocyte necrosis (Fig. 5). In addition, alcohol increased TNFR1 expression in hepatocytes (Fig. 6D). Alcohol increases the expression of TNFR1 in hepatocytes and exacerbates TNF-α-mediated hepatocellular necrosis (Rodriguez et al. 2004). This is supported by studies showing that the combination of alcohol and cocaine increases cocaine-induced toxicity (Bailey 1993; Herbst et al. 2011; Odeleye et al. 1993). Taken together, our results suggest that cocaine- and HA-induced liver inflammation through STING signaling causes hepatocellular necrosis through TNF-α signaling, which can be exacerbated by alcohol-enhanced TNFR.
In this study, we demonstrated that cocaine-induced liver inflammation could be induced in KC cultured at a high concentration of 250 µM. In human volunteers, serum cocaine levels range from 0.1 to 1 μM after a dose of 0.5 mg/kg, but cocaine abusers often reach 0.1 mM (Drummer 2004; Jatlow 1988). Moreover, reports of cocaine-related deaths have shown postmortem blood levels ranging from 1 µM to 1 mM(Karch et al. 1998; Mackey-Bojack et al. 2000). In general, the organ concentrations of cocaine are higher than those in the blood, with maximum concentrations typically found in the brain, lungs, liver, spleen, and kidneys (Amoedo et al. 1999; Kump et al. 1994; Poklis et al. 1987). Collectively, these studies suggest that the physiological relevance of the findings of the present study, which show that hepatocellular necrosis occurs via cocaine-induced inflammation, is reasonable.
Conclusions
Cocaine consumption activates hepatocytes to produce HA, which triggers mtDNA leakage and STING activation in KCs. This pathway plays a pivotal role in hepatocyte necroptosis in alcoholic liver disease. Furthermore, we showed that KCs mainly produce TNF-α in response to HA and initiate hepatocyte necroptosis in a paracrine manner. Our findings demonstrate for the first time that a cocaine insult promotes liver injury and inflammation via HA-dependent activation of STING and TNFR1 (Fig. 8). Understanding cocaine-HA-induced inflammation and necroptosis will offer valuable insights into preventing and treating simultaneous cocaine- and alcohol-mediated liver injuries.
Data Availability
No datasets were generated or analysed during the current study.
References
Abe T, Barber GN. Cytosolic-DNA-mediated, STING-dependent proinflammatory gene induction necessitates canonical NF-kappaB activation through TBK1. J Virol. 2014;88:5328–41. https://doi.org/10.1128/JVI.00037-14.
Amoedo ML, Craver L, Marco MP, Fernandez E. Cocaine-induced acute renal failure without rhabdomyolysis. Nephrol Dial Transplant. 1999;14:2970–1. https://doi.org/10.1093/ndt/14.12.2970.
An L, Wang X, Cederbaum AI. Cytokines in alcoholic liver disease. Arch Toxicol. 2012;86:1337–48. https://doi.org/10.1007/s00204-012-0814-6.
Bailey DN. Plasma cocaethylene concentrations in patients treated in the emergency room or trauma unit. Am J Clin Pathol. 1993;99:123–7. https://doi.org/10.1093/ajcp/99.2.123.
Barber GN. STING: infection, inflammation and cancer. Nat Rev Immunol. 2015;15:760–70. https://doi.org/10.1038/nri3921.
Bertola A, Mathews S, Ki SH, Wang H, Gao B. Mouse model of chronic and binge ethanol feeding (the NIAAA model). Nat Protoc. 2013;8:627–37. https://doi.org/10.1038/nprot.2013.032.
Bhattacharyya D, LeVatte MA, Wishart DS. A fast and accurate colorimetric assay for quantifying hippuric acid in human urine. Anal Biochem. 2023;680:115303. https://doi.org/10.1016/j.ab.2023.115303.
Cardoso-Moreira M, Sarropoulos I, Velten B, Mort M, Cooper DN, Huber W, Kaessmann H. Developmental Gene Expression Differences between Humans and Mammalian Models. Cell Rep. 2020;33:108308. https://doi.org/10.1016/j.celrep.2020.108308.
Chen C, Yang RX, Xu HG. STING and liver disease. J Gastroenterol. 2021;56:704–12. https://doi.org/10.1007/s00535-021-01803-1.
Cone EJ, Tsadik A, Oyler J, Darwin WD. Cocaine metabolism and urinary excretion after different routes of administration. Ther Drug Monit. 1998;20:556–60. https://doi.org/10.1097/00007691-199810000-00019.
Deng M, Li X, Li W, Gong J, Zhang X, Ge S, Zhao L. Short-Chain Fatty Acids Alleviate Hepatocyte Apoptosis Induced by Gut-Derived Protein-Bound Uremic Toxins. Front Nutr. 2021;8:756730. https://doi.org/10.3389/fnut.2021.756730.
Ding H, Tong J, Wu SC, Yin DK, Yuan XF, Wu JY, Chen J, Shi GG. Modulation of Kupffer cells on hepatic drug metabolism. World J Gastroenterol. 2004;10:1325–8. https://doi.org/10.3748/wjg.v10.i9.1325.
Drummer OH. Postmortem toxicology of drugs of abuse. Forensic Sci Int. 2004;142:101–13. https://doi.org/10.1016/j.forsciint.2004.02.013.
Gossop M, Manning V, Ridge G. Concurrent use and order of use of cocaine and alcohol: behavioural differences between users of crack cocaine and cocaine powder. Addiction. 2006;101:1292–8. https://doi.org/10.1111/j.1360-0443.2006.01497.x.
Grant BF, Harford TC. Concurrent and simultaneous use of alcohol with cocaine: results of national survey. Drug Alcohol Depend. 1990;25:97–104. https://doi.org/10.1016/0376-8716(90)90147-7.
Herbst ED, Harris DS, Everhart ET, Mendelson J, Jacob P, Jones RT. Cocaethylene formation following ethanol and cocaine administration by different routes. Exp Clin Psychopharmacol. 2011;19:95–104. https://doi.org/10.1037/a0022950.
Irwin C, van Reenen M, Mason S, Mienie LJ, Westerhuis JA, Reinecke CJ. Contribution towards a Metabolite Profile of the Detoxification of Benzoic Acid through Glycine Conjugation: An Intervention Study. PLoS ONE. 2016;11:e0167309. https://doi.org/10.1371/journal.pone.0167309.
Jatlow P. Cocaine: analysis, pharmacokinetics, and metabolic disposition. Yale J Biol Med. 1988;61:105–13.
Karch SB, Stephens B, Ho CH. Relating cocaine blood concentrations to toxicity–an autopsy study of 99 cases. J Forensic Sci. 1998;43:41–5.
Koop DR, Chernosky A, Brass EP. Identification and induction of cytochrome P450 2E1 in rat Kupffer cells. J Pharmacol Exp Ther. 1991;258:1072–6.
Krokos A, Deda O, Virgiliou C, Gika H, Raikos N, Aggelidou E, Kritis A, Theodoridis G. Evaluation of Cocaine Effect on Endogenous Metabolites of HepG2 Cells Using Targeted Metabolomics. Molecules. 2021;26. https://doi.org/10.3390/molecules26154610
Kump DF, Matulka RA, Edinboro LE, Poklis A, Holsapple MP. Disposition of cocaine and norcocaine in blood and tissues of B6C3F1 mice. J Anal Toxicol. 1994;18:342–5. https://doi.org/10.1093/jat/18.6.342.
Liu S, Guan W. STING Signaling Promotes Apoptosis, Necrosis, and Cell Death: An Overview and Update. Mediators Inflamm. 2018;2018:1202797. https://doi.org/10.1155/2018/1202797.
Ma HY, Yamamoto G, Xu J, Liu X, Karin D, Kim JY, Alexandrov LB, Koyama Y, Nishio T, Benner C, Heinz S, Rosenthal SB, Liang S, Sun M, Karin G, Zhao P, Brodt P, McKillop IH, Quehenberger O, Dennis E, Saltiel A, Tsukamoto H, Gao B, Karin M, Brenner DA, Kisseleva T. IL-17 signaling in steatotic hepatocytes and macrophages promotes hepatocellular carcinoma in alcohol-related liver disease. J Hepatol. 2020;72:946–59. https://doi.org/10.1016/j.jhep.2019.12.016.
Mackey-Bojack S, Kloss J, Apple F. Cocaine, cocaine metabolite, and ethanol concentrations in postmortem blood and vitreous humor. J Anal Toxicol. 2000;24:59–65. https://doi.org/10.1093/jat/24.1.59.
Maekawa H, Inoue T, Ouchi H, Jao TM, Inoue R, Nishi H, Fujii R, Ishidate F, Tanaka T, Tanaka Y, Hirokawa N, Nangaku M, Inagi R. Mitochondrial Damage Causes Inflammation via cGAS-STING Signaling in Acute Kidney Injury. Cell Rep. 2019;29(1261–73):e6. https://doi.org/10.1016/j.celrep.2019.09.050.
Mansouri A, Gaou I, De Kerguenec C, Amsellem S, Haouzi D, Berson A, Moreau A, Feldmann G, Letteron P, Pessayre D, Fromenty B. An alcoholic binge causes massive degradation of hepatic mitochondrial DNA in mice. Gastroenterology. 1999;117:181–90. https://doi.org/10.1016/s0016-5085(99)70566-4.
Moreira FP, Medeiros JR, Lhullier AC, Souza LD, Jansen K, Portela LV, Lara DR, da Silva RA, Wiener CD, Oses JP. Cocaine abuse and effects in the serum levels of cytokines IL-6 and IL-10. Drug Alcohol Depend. 2016;158:181–5. https://doi.org/10.1016/j.drugalcdep.2015.11.024.
Odeleye OE, Watson RR, Eskelson CD, Earnest D. Enhancement of cocaine-induced hepatotoxicity by ethanol. Drug Alcohol Depend. 1993;31:253–63. https://doi.org/10.1016/0376-8716(93)90008-e.
O'Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. J Stud Alcohol Suppl. 2002:23–39. https://doi.org/10.15288/jsas.2002.s14.23
Pennings EJ, Leccese AP, Wolff FA. Effects of concurrent use of alcohol and cocaine. Addiction. 2002;97:773–83. https://doi.org/10.1046/j.1360-0443.2002.00158.x.
Pezzilli R, Andreone P, Morselli-Labate AM, Sama C, Billi P, Cursaro C, Barakat B, Gramenzi A, Fiocchi M, Miglio F, Bernardi M. Serum pancreatic enzyme concentrations in chronic viral liver diseases. Dig Dis Sci. 1999;44:350–5. https://doi.org/10.1023/a:1026662719514.
Poklis A, Maginn D, Barr JL. Tissue disposition of cocaine in man: a report of five fatal poisonings. Forensic Sci Int. 1987;33:83–8. https://doi.org/10.1016/0379-0738(87)90143-5.
Riezzo I, Fiore C, De Carlo D, Pascale N, Neri M, Turillazzi E, Fineschi V. Side effects of cocaine abuse: multiorgan toxicity and pathological consequences. Curr Med Chem. 2012;19:5624–46. https://doi.org/10.2174/092986712803988893.
Rodriguez DA, Moncada C, Nunez MT, Lavandero S, Ponnappa BC, Israel Y. Ethanol increases tumor necrosis factor-alpha receptor-1 (TNF-R1) levels in hepatic, intestinal, and cardiac cells. Alcohol. 2004;33:9–15. https://doi.org/10.1016/j.alcohol.2004.03.001.
Rodriguez-Alvarez T, Racamonde I, Gonzalez-Marino I, Borsotti A, Rodil R, Rodriguez I, Zuccato E, Quintana JB, Castiglioni S. Alcohol and cocaine co-consumption in two European cities assessed by wastewater analysis. Sci Total Environ. 2015;536:91–8. https://doi.org/10.1016/j.scitotenv.2015.07.016.
Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff BA, Gawin F. Psychiatric diagnoses of treatment-seeking cocaine abusers. Arch Gen Psychiatry. 1991;48:43–51. https://doi.org/10.1001/archpsyc.1991.01810250045005.
Sadakierska-Chudy A, Kotarska A, Frankowska M, Jastrzebska J, Wydra K, Miszkiel J, Przegalinski E, Filip M. The Alterations in Mitochondrial DNA Copy Number and Nuclear-Encoded Mitochondrial Genes in Rat Brain Structures after Cocaine Self-Administration. Mol Neurobiol. 2017;54:7460–70. https://doi.org/10.1007/s12035-016-0153-3.
Sauer JD, Sotelo-Troha K, von Moltke J, Monroe KM, Rae CS, Brubaker SW, Hyodo M, Hayakawa Y, Woodward JJ, Portnoy DA, Vance RE. The N-ethyl-N-nitrosourea-induced Goldenticket mouse mutant reveals an essential function of Sting in the in vivo interferon response to Listeria monocytogenes and cyclic dinucleotides. Infect Immun. 2011;79:688–94. https://doi.org/10.1128/IAI.00999-10.
Schwabe RF, Brenner DA. Mechanisms of Liver Injury. I. TNF-alpha-induced liver injury: role of IKK, JNK, and ROS pathways. Am J Physiol Gastrointest Liver Physiol. 2006;290:G583–9. https://doi.org/10.1152/ajpgi.00422.2005
Shalini S, Dorstyn L, Dawar S, Kumar S. Old, new and emerging functions of caspases. Cell Death Differ. 2015;22:526–39. https://doi.org/10.1038/cdd.2014.216.
Shang L, Jin Z, Wei H, Park S, Zhan CG, Zheng F. Catalytic activities of a highly efficient cocaine hydrolase for hydrolysis of biologically active cocaine metabolites norcocaine and benzoylecgonine. Sci Rep. 2023;13:640. https://doi.org/10.1038/s41598-022-27280-x.
Sil S, Niu F, Tom E, Liao K, Periyasamy P, Buch S. Cocaine Mediated Neuroinflammation: Role of Dysregulated Autophagy in Pericytes. Mol Neurobiol. 2019;56:3576–90. https://doi.org/10.1007/s12035-018-1325-0.
Singh AK. Alcohol Interaction with Cocaine, Methamphetamine, Opioids, Nicotine, Cannabis, and gamma-Hydroxybutyric Acid. Biomedicines. 2019;7. https://doi.org/10.3390/biomedicines7010016
Sun B, Wang X, Liu X, Wang L, Ren F, Wang X, Leng X. Hippuric Acid Promotes Renal Fibrosis by Disrupting Redox Homeostasis via Facilitation of NRF2-KEAP1-CUL3 Interactions in Chronic Kidney Disease. Antioxidants (Basel). 2020;9. https://doi.org/10.3390/antiox9090783
Thomsen MK, Nandakumar R, Stadler D, Malo A, Valls RM, Wang F, Reinert LS, Dagnaes-Hansen F, Hollensen AK, Mikkelsen JG, Protzer U, Paludan SR. Lack of immunological DNA sensing in hepatocytes facilitates hepatitis B virus infection. Hepatology. 2016;64:746–59. https://doi.org/10.1002/hep.28685.
Vitcheva V. Cocaine toxicity and hepatic oxidative stress. Curr Med Chem. 2012;19:5677–82. https://doi.org/10.2174/092986712803988929.
Weigand KM, Schirris TJJ, Houweling M, van den Heuvel J, Koenderink JB, Dankers ACA, Russel FGM, Greupink R. Uremic solutes modulate hepatic bile acid handling and induce mitochondrial toxicity. Toxicol in Vitro. 2019;56:52–61. https://doi.org/10.1016/j.tiv.2019.01.003.
Xue C, Gu X, Li G, Bao Z, Li L. Mitochondrial Mechanisms of Necroptosis in Liver Diseases. Int J Mol Sci. 2020;22. https://doi.org/10.3390/ijms22010066
Yu HS, Oyama T, Isse T, Kitagawa K, Pham TT, Tanaka M, Kawamoto T. Formation of acetaldehyde-derived DNA adducts due to alcohol exposure. Chem Biol Interact. 2010;188:367–75. https://doi.org/10.1016/j.cbi.2010.08.005.
Yu Y, Liu Y, An W, Song J, Zhang Y, Zhao X. STING-mediated inflammation in Kupffer cells contributes to progression of nonalcoholic steatohepatitis. J Clin Invest. 2019;129:546–55. https://doi.org/10.1172/JCI121842.
Zhao J, Jitkaew S, Cai Z, Choksi S, Li Q, Luo J, Liu ZG. Mixed lineage kinase domain-like is a key receptor interacting protein 3 downstream component of TNF-induced necrosis. Proc Natl Acad Sci U S A. 2012;109:5322–7. https://doi.org/10.1073/pnas.1200012109.
Zhong Z, Goto M, Hijioka T, Oide H, Kauffman FC, Thurman RG. Role of Kupffer cells in storage and metabolism of benzo(a)pyrene in the liver. Drug Metab Dispos. 1994;22:680–7.
Zhou Y, Wu R, Wang X, Bao X, Lu C. Roles of necroptosis in alcoholic liver disease and hepatic pathogenesis. Cell Prolif. 2022;55:e13193. https://doi.org/10.1111/cpr.13193.
Acknowledgements
We extend our deepest gratitude to the editors and reviewers for their invaluable insights and constructive feedback on this manuscript.
Funding
This study was supported by National Research Foundation of Korea (2017R1A5A2015541), Korean Food and Drug Administration (20182MFDS425), Regional Innovation Strategy (RIS) of National Research Foundation of Korea (2021RIS-001).
Author information
Authors and Affiliations
Contributions
H.M and G.R.L established the hypothesis, conducted the experiments, analyzed the data, and wrote the manuscript. J.S.P, J.L, F.W, Y.M, G.Y.S, N.R, S.H.K and Y.S.J conducted the experiments and analyzed the data. H.S.Y, S.B.H, J.T.H, J.S.Y, and Y.S.R designed the experiments, analyzed the data, and wrote and edited the manuscript. Y.S.R is the guarantor and accepts full responsibility for the work and conduct of the study, has access to the data, and controls the decision to publish. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Marmoset experiments were performed at the Osong Medical Innovation Foundation Laboratory Animal Center (Chungbuk, Republic of Korea) with the approval of the Animal Control Committee (KBIO-IACUC-2020–148) of the animal testing institution. Mice experimental were performed according to the guidelines of the Institutional Animal Care and Use Committee (IACUC) and approved by the animal experimental animal care of Chungbuk National University, Cheongju, Republic of Korea (ethical approval NO. CBNUA-1203–18-02).
Competing interests
The authors declare no competing interests.
Conflict of Interest statement
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hwan Ma and Gyu Rim Lee have made equal contributions to this work and therefore should be acknowledged as co first authors.
Corresponding authors Correspondence to Jaesuk Yun or Yoon Seok Roh
Highlights
• Hippuric acid is the most abundant metabolite in serum of cocaine-abused marmosets.
• Cocaine and hippuric acid induce mitochondrial damage and mtDNA leakage.
• STING signaling mediates mtDNA-induced TNF-α production in Kupffer cells.
• KCs-derived TNF-α promotes hepatocytes necroptosis by TNFR1, whose expression increased by alcohol.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, H., Lee, GR., Park, JS. et al. Cocaine-derived hippuric acid activates mtDNA-STING signaling in alcoholic liver disease: Implications for alcohol and cocaine co-abuse. Cell Biol Toxicol 40, 71 (2024). https://doi.org/10.1007/s10565-024-09901-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10565-024-09901-5