Abstract
To report the clinical results on the use of corneas frozen in Eusol-C as tectonic corneal grafts.Retrospective review of medical records of patients who received frozen corneas as emergency tectonic grafts from 2013 to 2020. Corneas had been stored in Eusol-C preservation media at − 78 °C for a mean time of 6.9 months. Diagnosis, transplant characteristics, microbial culture results, anatomic integrity, epithelial healing, neovascularization, transparency, infection and need for additional surgeries were registered. Fifty corneas were used in 40 patients (mean age 60.5 years, 20 males) with a median follow-up of 27.3 months after surgery. Need for tectonic graft was due to: perforation secondary to immune diseases (6, 12%), neurotrophic ulcer (11, 22%), trauma (3, 6%), corneal infection (11, 22%), chronic disorders of the ocular surface (9, 18%) and previous corneal graft failure (10, 22%). Mean size of grafts was 5.6 mm and 36 cases (72%) also received an amniotic membrane graft. Thirty-eight corneas achieved epithelization (76%), 25 (50%) were clear and 19 (38%) developed neovascularization. None of the corneas were rejected. Seventeen corneas (34%) failed: 7 (14%) due to reactivation of baseline disease and 10 (20%) due to primary graft failure. Four corneas (8%) had positive microbial cultures suggestive of contamination and 2 (4%) developed a cornea abscess non-related to a positive microbial culture. Long-term preservation of donor corneas in Eusol-C at − 78 °C is a viable technique to meet the needs of emergency grafts with minimal equipment.
Similar content being viewed by others
Introduction
Around 40 million people worldwide are blind, corneal-related blindness, such as trachoma and corneal opacities, representing the third cause of blindness, behind cataracts and glaucoma. (GBD 2019 Blindness and Vision Impairment Collaborators & Vision Loss Expert Group of the Global Burden of Disease Study 2021; Pascolini and Mariotti 2012) The great majority of patients with visual impairment due to corneal disease can be treated with corneal transplantation. Most common causes for transplant are Fuchs dystrophy, keratoconus and sequalae of infectious keratitis (Gain et al. 2016).
Corneal transplant is considered the world's most frequent type of transplantation and more than 185,000 corneal transplants are performed every year (Gain et al. 2016). Nevertheless, there are millions of patients worldwide who are waitlisted and around 50% of the world's population have no access to corneal transplantation (Gain et al. 2016; GBD 2019 Blindness and Vision Impairment Collaborators & Vision Loss Expert Group of the Global Burden of Disease Study 2021) Corneal tissue shortage has thus been an ongoing issue, which has worsened due to the Covid-19 pandemic (Aiello et al. 2021; Servin-Rojas et al. 2021).
Efforts have been made to optimize the use of available corneal tissue, with individual corneas being implanted in two and even three different recipients (Heindl et al. 2011; Vajpayee et al. 2007). Furthermore, the use of long term stored corneas has also helped reduce this tissue shortage. Cryopreservation is the only current long-term storage method that can virtually preserve tissue structure (Armitage 2009; Chaurasia et al. 2020). Also, ophthalmic emergencies such as corneal perforation or impending corneal perforation require immediate detection and prompt intervention. In this context, the use of frozen corneas is promising because it allows simple, fast and low cost amassing of sizable amounts of material with long storage time (Kim et al. 2016; Robert et al. 2012).
For the past years, unused corneal lenticules have been stored in Eusol-C (Corneal Chamber, Alchimia, Ponte San Nicolo, Italy) at − 78 °C in our hospital in order to have corneas stored for urgent transplants in cases of corneal perforations. However, this technique has not been widely described. Given the low cost and easiness of this conservation method, it could be useful to reflect our good results for Eye Banks in developing countries or those with fewer resources. Therefore, we hereby report the clinical results regarding efficacy and safety on the use of corneas frozen in Eusol-C as tectonic corneal grafts in a tertiary centre in Spain.
Methods
For this retrospective study, the medical records of patients who received frozen corneas as emergency tectonic grafts from 2013 to 2020 at the Hospital Clinico San Carlos in Madrid, Spain were reviewed. The protocol was approved by the hospital’s Ethics Committee and no informed consent was necessary.
All corneas that had been stored in Eusol-C preservation media (Corneal Chamber, Alchimia, Ponte San Nicolo, Italy) at − 78 °C and later used in corneal transplant surgeries were included. The only exclusion criterion was insufficient follow-up data in the medical history.
All donors are routinely tested for human immunodeficiency virus, hepatitis B virus, and hepatitis C virus, syphilis, toxoplasma gondii, brucella, Epstein-Barr virus, herpes simplex types I and II, varicella-zoster, cytomegalovirus and human T cell lymphotropic virus (HTLV) I.
Age, sex and cause of death of the donor were noted. Diagnosis, transplant characteristics (size of tectonic graft, adjuvant use of amniotic membrane graft), microbial culture results, anatomic integrity, epithelial healing, neovascularization, transparency, infection, rejection, need for additional surgeries and follow-up time were registered, as well as storage time of the cornea.
The primary efficacy endpoint was whether reepithelization was achieved, while secondary endpoints were transparency, neovascularization, rejection and need for additional surgeries. Safety endpoint was positivity of microbial cultures. All removed failed grafts were tested for microbiology.
Statistical analysis was performed using SPSS v25.0 (SPSS, Chicago, IL). Quantitative variables are represented by their mean, along with their standard deviation (SD), while qualitative variables are shown as proportions.
Results
Fifty corneas that had been stored in Eusol-C preservation media and stored at − 78 °C for a mean time of 6.9 months (range 15 days to 12 months) were included. The fifty corneas were used in forty patients (mean age 60.5 years, 20 males) with a median follow-up of 27.3 months after surgery.
Need for tectonic graft was due to: perforation secondary to immune diseases (6, 12%), neurotrophic ulcer (11, 22%), trauma (3, 6%), corneal infection (11, 22%), chronic conditions of the ocular surface (9, 18%) and failure of previous corneal graft (10, 22%). Mean size of grafts was 5.6 mm (range 3 to 11) and 36 cases (72%) also received an amniotic membrane graft. The surgeries were successful in all cases with restitution of the globe integrity.
Thirty-eight corneas achieved epithelization (76%), 25 (50%) were clear and 19 (38%) developed neovascularization. None of the corneas were rejected. 17 corneas (34%) failed, thus requiring a new surgery: 7 (14%) due to reactivation of baseline disease, 8 (16%) due to primary failure of the graft and 2 (4%) due to perforation of a corneal abscess. In 10 of these 17 failures, a new frozen cornea was used due to a lack of fresh tissue at that moment.
Four corneas (8%) had positive microbial cultures suggestive of contamination and 2 (4%) developed a corneal abscess non-related to a positive microbial culture, both corneas.
Discussion
Shortage of corneal tissue for transplant is an ongoing issue, which has worsened in the past years, when many potential donors have been discarded due to the pandemic and the difficulty in booking ocular surgeries. We present a viable method of conservation for emergencies that requires little material and is thus suitable for eye banks with few resources. In addition, the use of frozen corneas in Eusol-C may serve as an efficient temporary measure for tectonic restoration of perforated corneas (Fig. 1).
A 50-year-old patient, with a DSAEK 5 years earlier due to bullous keratopathy, presented with central corneal perforation (A). A 4 mm tectonic graft was sutured along with an amniotic membrane graft. Reepithelization was achieved, with no corneal neovascularization and good transparency. There was no graft rejection or infection. Images illustrate graft appearance on the first day (B), 2 weeks (C), 6 weeks (D), 6 months (E) and 12 months (F) after surgery
During the last decades, with the development of new corneal storage media, an important improvement in the corneal tissue conservation has been achieved. Optisol-GS (Bausch & Lomb, Inc., Rochester, NY, USA) is the most widely used storage medium in the United States, while in Europe it is Eusol-C. Eusol-C is an intermediate-term storage media which has dextran as osmotic agent, sodium pyruvate and glucose as energetic sources, amino acids, mineral salts and vitamins as nutrients, along with gentamicin as antibiotic, Hepes and bicarbonate as buffers, and phenol red as pH indicator (Yüksel et al. 2016).
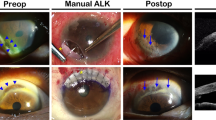
Long-term corneal storage techniques are much more elaborate than short-term ones and include glycerol preservation, lyophilization, gamma irradiation, and cryopreservation. These techniques are generally limited by lack of viable cells in the tissue, the longer time to epithelialization and the graft opacification (Fig. 2).
A 59-year-old patient with ocular pemphigoid, which had required multiple previous amniotic membrane grafts in the past, presented with corneal perforation (A) due to reactivation of the disease. A 4 mm corneal graft combined with amniotic membrane was performed. Reepithelization was achieved, although there was corneal neovascularization and loss of transparency. Images of the first day (B), first month (C) and third month (D) are shown. Despite good results, further corneal grafts were needed at 6 and 8 months due to relapse of the disease
However, advantages of long-term corneal preservation include the limited expression of MHC antigens, reducing the risk of rejection and that keratocytes and endothelial cells of the donor can repopulate the acellular cornea (Lynch and Ahearne 2013). In some cases, frozen and fresh corneal donors have even proven to be equally efficient and safe, with similar recuperation of visual acuity and no untoward complications, such as melting, leaks, or endophthalmitis (Fig. 3) (Robert et al. 2012).
An 83-year-old patient presented in the Emergency Room with corneal perforation due to pellucid marginal degeneration (A). A horseshoe shaped graft with an external diameter of 10 mm was cut and an amniotic membrane graft was also sutured. Reepithelization was achieved, with no neovessels and excellent transparency. No graft rejection or failure was noted during 3 years of follow-up. Images of the first day (B), 1 week (C), 1 month (D), 8 months (E) and 2 years (F) after surgery are shown
The present case series proves that storage of cornea in Eusol-C at − 78 °C is a simple technique, requiring minimal equipment, which avoids wasting viable tissue more suited for elective surgeries and can effectively be used in tectonic grafts. The reason to include Eusol-C as medium, instead of a more suitable medium for cryopreservation or with glycerol, was because of its wide availability in most hospitals not necessarily performing corneal transplantation.
All of the surgeries were successful in terms of restitution of the globe integrity. Overall, 76% of the corneas achieved epithelization (38 patients), 25 (50%) were clear and 19 (38%) developed neovascularization. None of the corneas were rejected. However, 17 corneas (34%) failed: 7 (14%) due to reactivation of baseline disease and 10 (20%) due to primary failure of the graft.
In long-term techniques the graft tends to remain opaque and cosmetically unsatisfactory. However spontaneous graft clearing is also possible in cases where the surrounding host endothelium is healthy and migrates into the graft (Sharma et al. 2001). In a series of 195 patients who underwent therapeutic penetrating keratoplasty with cryopreserved corneas without endothelium, 18 patients (9.23%) achieved a clear graft postoperatively (Ying et al. 2022). Despite graft sizes ranging from 7.0 to 9.5 mm, a mean cell density of 991 cells/mm2 (range, 782–1531 cells/mm2) was reached. The greater graft size is probably responsible for a lower proportion of endothelial regeneration and thus less patients with clear grafts. In smaller grafts like those here presented, cell proliferation and cell migration are probably more easily achieved and explain the better outcomes.
One of the main risk factors for corneal transplants is donor cornea contamination. The use of antibiotics in storage media remains as one of the most important safety measures in order to minimize the contamination risk in corneal preservation. In the present study, four corneas (8%) had positive microbial cultures suggestive of contamination and 2 (4%) developed a cornea abscess non-related to a positive microbial culture. These results are quite similar to other series (Gruenert et al. 2017, Li et al. 2019; Ling et al. 2019). Li et al. (2019) reported 8.2% of positive cultures in 111 donor corneas, most common bacteria and fungi being Acinetobacter baumannii complex (19.8%) and Candida spp. (9.0%), respectively. Only two patients (1.8%) who received contaminated corneal buttons developed postoperative infections. Death due to cardiac disease and longer preservation time was associated with increasing contamination rates. In another series including 3306 donor corneas, (Gruenert et al. 2017) the overall contamination rate was 7.8% and, in this case, younger donor age, a death-to-explantation interval of more than 24 h, hospitalization prior to death and death caused by sepsis were associated with a higher risk of contamination. Most common microbes were Enterococci (19%), Staphylococci (10.8%) and Candida (37.4%). On the other hand, Vignola et al. (2019) tested 100 donor corneas for microbial contamination after cold storage, corneal culture and corneal deswelling at the Eye Bank of Rome. Tissue contamination was unexpectedly high given that 67% of the Eusol-C samples were contaminated, mainly by Staphylococcus spp.
Some limitations of the method hereby described should be acknowledged. A relatively high number of patients suffered graft failure (34%), although many of them (14%) were due to worsening of baseline disease. Therefore, it might not be the perfect technique for elective surgeries, but can be a useful option in emergency tectonic grafts. Also, despite graft opacifications in some cases, this technique may circumvent the problem of corneal shortage and serve as an intermediary procedure with a definitive optical transplant with fresh tissue at a later date, avoiding having to discard unused corneas.
In conclusion, long-term preservation of donor corneas in Eusol-C at − 78 °C is a viable technique to meet the needs of emergency grafts with minimal equipment and in corneal shortage scenarios.
References
Aiello F, Genzano Besso F, Pocobelli G, Gallo Afflitto G, Colabelli Gisoldi RAM, Nucci C, Ponzin D, Italian Society Eye Bank Group (SIBO) (2021) Corneal transplant during COVID-19 pandemic: the Italian Eye Bank national report. Cell Tissue Bank 22:697–702
Armitage J (2009) Cryopreservation for corneal storage. Dev Ophthalmol 43:63–69
Chaurasia S, Das S, Roy A (2020) A review of long-term corneal preservation techniques: relevance and renewed interests in the COVID-19 era. Indian J Ophthalmol 68:1357–1363
Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, Thuret G (2016) global survey of corneal transplantation and eye banking. JAMA Ophthalmol 134:167–173
GBD 2019 Blindness and Vision Impairment Collaborators & Vision Loss Expert Group of the Global Burden of Disease Study (2021) Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health 9:e130–e143
Gruenert AK, Rosenbaum K, Geerling G, Fuchsluger TA (2017) The influence of donor factors on corneal organ culture contamination. Acta Ophthalmol 95:733–740
Heindl LM, Riss S, Bachmann BO, Laaser K, Kruse FE, Cursiefen C (2011) Split cornea transplantation for 2 recipients: a new strategy to reduce corneal tissue cost and shortage. Ophthalmology 118:294–301
Kim KY, Jung JW, Kim EK, Seo KY, Kim TI (2016) Tectonic lamellar keratoplasty using cryopreserved cornea in a large descemetocele. Yonsei Med J 57:269–271
Li S, Zhong J, Tan Y, Deng Y, Huang H, Wang B, Peng L, Zhang H, Yuan J (2019) Microbiological screening of hypothermic preserved donor corneas in keratoplasty. Curr Eye Res 44:1067–1074
Ling MLH, Wells M, Petsoglou C, Luo K, Georges P, Devasahayam R, Hodge C, Treloggen J, Sutton G, Zhu M (2019) Factors affecting corneal organ culture contamination: a 6-year study at the new south wales tissue bank. Cornea 38:829–835
Lynch AP, Ahearne M (2013) Strategies for developing decellularized corneal scaffolds. Exp Eye Res 108:42–47
Pascolini D, Mariotti SP (2012) Global estimates of visual impairment: 2010. Br J Ophthalmol 96:614–618
Robert M-C, Biernacki K, Harissi-Dagher M (2012) Boston keratoprosthesis type 1 surgery: use of frozen versus fresh corneal donor carriers. Cornea 31:339–345
Servin-Rojas M, Olivas-Martinez A, Ramirez Del Val F, Torres-Gomez A, Navarro-Vargas L, García-Juárez I (2021) Transplant trends in Mexico during the COVID-19 pandemic: disparities within healthcare sectors. Am J Transpl 21:4052–4060
Sharma A, Gupta P, Narang S, Ram J, Gupta A (2001) Clear tectonic penetrating graft using glycerine-preserved donor cornea. Eye 15:345–347
Vajpayee RB, Sharma N, Jhanji V, Titiyal JS, Tandon R (2007) One donor cornea for 3 recipients: a new concept for corneal transplantation surgery. Arch Ophthalmol (chicago, Ill 1960) 125:552–554
Vignola R, Giurgola L, Colabelli Gisoldi RAM, Gaudio M, D’Amato Tóthová J, Pocobelli A (2019) Monitoring the microbial contamination of donor cornea during all preservation phases: a prospective study in the Eye Bank of Rome. Transpl Infect Dis 21:e13041
Ying L-Y, Qiu W-Y, Wang B-H, Zhou P, Zhang B, Yao Y-F (2022) Corneal endothelial regeneration in human eyes using endothelium-free grafts. BMC Ophthalmol 22:32
Yüksel B, Uzunel UD, Küsbeci T (2016) Endothelial cell viability of donor corneas preserved in eusol-c corneal storage medium. Exp Clin Transpl 14:441–444
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. There are no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burgos-Blasco, B., Vidal-Villegas, B., Collado-Vincueria, I. et al. Clinical outcomes of long-term corneas preserved frozen in Eusol-C used in emergency tectonic grafts. Cell Tissue Bank 24, 351–356 (2023). https://doi.org/10.1007/s10561-022-10037-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-022-10037-1