Abstract
Bone banks are necessary for providing biological allografts for a series of orthopedic procedures. As nations cope with new realities driven by the 2019 coronavirus disease (COVID-19) pandemic, health-care providers, institutions, and patients share a particular concern about the effect of COVID-19 on organ donation and transplantation. Here, we describe the management of the Kitasato University Bone Bank during the state of emergency declared in response to COVID-19. Living donors received pre-operative screening by PCR, and allograft bone from COVID-19-negative donors was cryopreserved as transplantable tissues. The weekly rate of infection gradually increased from February 2–9 to April 5–11 in the dead donor-derived allograft bone-harvesting region covered by the Bank. It is becoming clear that the virus can be transmitted by asymptomatic patients, and that this route may have facilitated the spread of COVID-19. Therefore, the Bank stopped dead donor donation to consider the safety of medical staff. Three recipients received bone allografts following pre-operative COVID-19 screening by PCR. All patients were asymptomatic after bone allograft. Our experience may provide helpful information for the management of tissue banks.
Similar content being viewed by others
Introduction
The number of bone allografts conducted in the Japanese orthopaedic field continues to increasing (Iwamoto et al. 1997; Komiya et al. 2003; Urabe et al. 2007). Bone banks play a necessary role in providing biological allografts for a series of orthopedic procedures. Kitasato University Bone Bank (KUBB) is a regional bone bank which harvests, processes, preserves, and provides allograft bone harvested from living and dead donors for bone allografting in Japan. KUBB is one of only three regional bone banks in Japan and plays an important role in providing allograft bone tissue across Japan.
The first case of coronavirus disease 2019 (COVID-19) was described in December 2019 in Wuhan, China. On January 16, 2020, the first reports of COVID-19 were officially announced by the Ministry of Health Labour and Welfare in Japan. The COVID-19 pandemic is the most important health care crisis of this century. Prime Minister Shinzo Abe declared a state of emergency in seven urban areas in Japan on April 7 and extended it until May 25. Previous studies reported a strong temporal association between the increase in COVID-19 infections and a marked overall decrease in solid-organ transplantation procedures and procurement in Europe, USA, and the Middle East (Loupy et al. 2020; Dominguez-Gil et al. 2020; Zidan et al. 2020). A recent study reported methods for donor selection for solid organ transplantation during the pandemic (Galvan et al. 2020). However, a standardized and comprehensive approach to the evaluation of donors with possible COVID-19 infection in tissue banks has not been fully established.
KUBB is located in Kanagawa Prefecture, Japan. Kanagawa Prefecture has the third-highest number of infected patients in Japan. The number of COVID-19-infected patients in Japan has been relatively small compared to other countries such as the USA and those in Europe. However, management of bone banks differs from each country. For example, allograft bone is sterilized using gamma irradiation in the USA, but by heat treatment at 60 °C for 10 h in Japan. Therefore, our experience may aid the maintenance of tissue banks during and after this pandemic. Here, we describe the management of KUBB during the state of emergency declared for COVID-19.
KUBB: bone banking procedures and importance in the region
Role of KUBB
KUBB participates in harvesting from living and dead donors, virus and microbial testing, cold preservation, processing, and shipping to hospitals across Japan (Fig. 1). KUBB harvests femoral heads from living donors who undergoing surgery for hip osteoarthritis and femoral neck fracture in Kitasato University hospital. KUBB harvests bones, including femur, tibia, and iliac bon; and tendons, including Achilles tendon and patellar ligament from dead donors, including those with cardiac and brain death. After microbial and virus testing, harvested bone from both living and dead donors is preserved deep frozen at − 80 °C before processing. During processing, soft tissue around the bone is removed, and the bone tissue is then generally heated at 60 °C for 10 h during processing. After screening using swab tests, processed bone is preserved deep frozen at − 80 °C until allografting. KUBB harvests bone tissue from an annual average 117 living donors and 4 dead donors during 2015–2019 and provided annual average 135 bone products to 13 hospitals.
Number of harvested femoral heads from living donors
We counted the number of harvested allograft bone during the state of emergency (April 7 2020 to May 24 2020) in 2020. All living donors without symptoms of fever, shortness of breath, and desaturation underwent PCR screening one day before orthopedic surgery.
Estimation of the number of COVID-19 patients in the KUBB allograft bone-harvesting region
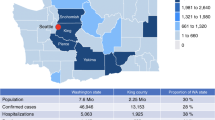
We estimated the number of COVID-19 patients in the KUBB allograft bone-harvesting region, which includes Tokyo, Kanagawa, Saitama, and western Shizuoka (Fig. 2) from February 12 to May 24 2020 using information from the Tokyo, Kanagawa, Chiba, and Shizuoka governments’ official home pages (Tokyo, https://stopcovid19.metro.tokyo.lg.jp/; Kanagawa, https://www.pref.kanagawa.jp/docs/ga4/bukanshi/occurrence_03.html (in Japanese); Chiba, http://www.pref.chiba.lg.jp/shippei/press/2019/ncov-index.html (in Japanese); and Shizuoka, https://www.pref.shizuoka.jp/kinkyu/covid-19-tyuumokujouhou.html (in Japanese)).
Allograft
Three recipients—namely one each with lumbar spinal stenosis, loosening of total hip arthroplasty and kyphosis—received a bone allograft during the state of emergency at Kitasato University Hospital. Recipients without symptoms of fever, shorter of breath, and desaturation underwent PCR screening three day before orthopedic surgery. Allograft bone harvested from donors no earlier than 6 months before April were used for grafts.
Management of the KUBB during COVID times
Number of bone allografts harvested from living donors
During the state of emergency, 12 allografts were harvested from living donors with osteoarthritis (11 hips) and femoral neck fracture (1 hip) following PCR screening of living donors. All living donors were negative for COVID-19. In contrast, 24 allografts were harvested from living donors with osteoarthritis (24 hips) during the same period in 2019, indicating a 50% decrease in the number of living donors during the state of emergency.
Harvesting from dead donors
The weekly rate of infection gradually increased from February 2–9 to April 5–11 in Tokyo, Kanagawa, Chiba, and Western Shizuoka (Fig. 3). Various lines of evidence suggest that the virus is transmitted by asymptomatic patients, and that this route may have facilitated the spread of COVID-19 (Bai et al. 2020; Li et al. 2020). KUBB harvested from an average of 4 dead donors/year during 2015–2019, but stopped dead donor donation during the state of emergency in consideration of the safety of medical staff.
Bone allografts
Three patients remained asymptomatic after orthopedic surgery during 4 weeks of follow up. No physicians or medical staff developed symptoms of COVID-19. In contrast, 12 allografts were transplanted into patients during the same period in 2019, indicating a 75% decrease in the number of living donors during the state of emergency.
The aftermath of a pandemic in tissue banking
Many health care workers around the world have succumbed to this virus, and many orthopedic departments of hospitals have stopped or markedly reduced elective surgery. The widespread recommendation in the US to delay elective operations during the pandemic has produced a large population of patients with hip and knee osteoarthritis who are unable to receive their recommended surgical treatment (Brown et al. 2020). In KUBB, this decrease in elective surgery has resulted in a decrease in the number of allograft bone harvests from living donors. However, as all patients were COVID-19-negative on pre-operative screening, allograft bone was cryopreserved at − 80 °C as transplantable tissue. A WHO laboratory network reported that only a minimal reduction in SARS coronavirus concentration was observed after 21 days at − 80 °C (WHO Laboratory Network 2020), but that SARS coronavirus was quickly killed by heat at 56 °C for 15 min (WHO Laboratory Network 2020). In Japan, allograft bone undergoes heat treatment at 60 °C for 10 h before bone grafting. Given that PCR testing produces some false negative results (Ai et al. 2020; Kucirka et al. 2020), heat treatment may be effective in preventing COVID-19 infection via allograft materials.
Cryopreserved allograft bone tissue remains transplantable for a long time. Almost all tissue banks keep allografts at 70 °C to 80 °C, which allows storage for 3 to 5 years (Shelton 2003; Vangsness Jr. et al. 2006). As KUBB had preserved 458 bone allograft at this time, donation was stopped due to the increase in COVID-19-infected patients in the allograft bone-harvesting region following consideration of the urgency of bone harvesting and the risk and benefits.
Organ donor screening for COVID-19 by approach to donation differs slightly among countries (Kumar et al. 2020). Nucleic acid testing using PCR has been recommended in several countries. The Japan Society for Transplantation issued a formal statement on March 6, 2020 (http://www.asas.or.jp/jst/pdf/info_20200306.pdf; in Japanese) which recommended that donor screening should include nucleic acid testing, fever, respiratory symptoms, exposure to COVID-19, and history of travel to high-risk countries. Therefore, PCR analysis during hospitalization before brain death may be necessary for harvesting of allograft bone from brain-death donor. In contrast, previous studies reported that COVID-19 infection was observed in trauma patients (Mahdavi et al. 2020; Khazaei et al. 2020). Donor assessment when considering harvesting from cardiac-death donors will need to be performed rapidly, and will require rapid and exact detection tools in order to prevent infection of coordinators and medical staff.
Recipients of organ translation should undergo clinical and/or laboratory screening for COVID-19. We performed clinical and laboratory screening in three recipients before bone allograft, and confirmed that they were asymptomatic after allograft. Some centers for organ transplantation are not currently PCR screening asymptomatic recipients who are admitted for transplantation (Kumar et al. 2020). We Strengthening of recipient screening methods may be warranted given the increasing numbers of COVID-infected patients. Further investigation with large sample size is needed.
KUBB provides allograft bone from dead donors across Japan, as it is one of only three regional bone banks in this country. The decrease in donors during the state of emergency concerning COVID-19 has affected bone allografting, and the rate of surgery may be expected to increase again in the future. In addition, a continuous reduction in KUBB activity due to second- and third-wave infections may lead to the depletion of bone allografts obtained from dead donors and affect bone allograft activity in Japan. To guarantee allograft bone transplantation, establishment of screening and biological inactivation methods during bone processing will be needed.
Two major limitation of this study warrant mention. First, the number of cases was small. Further investigation with larger sample sizes is needed. Second, the follow-up period in patients received allografts was short. Longer term follow-up is needed.
We describe the management of a regional bone bank during a state of emergency declared for the COVID-19 in Japan. Our experience may provide helpful information for the management of tissue bank risk.
References
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L (2020) Correlation of chest CT and RT-PCR testing in Coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 296:E32–E40
Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, Wang M (2020) Presumed asymptomatic carrier transmission of COVID-19. JAMA 323:1406–1407
Brown TS, Bedard NA, Rojas EO, Anthony CA, Schwarzkopf R, Barnes CL, Stambough JB, Mears SC, Edwards PK, Nandi S, Prieto HA, Parvizi J (2020) The effect of the COVID-19 pandemic on electively scheduled hip and knee arthroplasty patients in the United States. J Arthroplasty 35:S45–S48
Dominguez-Gil B, Coll E, Fernandez-Ruiz M, Corral E, Del RF, Zaragoza R, Rubio JJ, Hernandez D (2020) COVID-19 in Spain: transplantation in the midst of the pandemic. Am J Transplant. https://doi.org/10.1111/ajt.16369
Galvan NTN, Moreno NF, Garza JE, Bourgeois S, Hemmersbach-Miller M, Murthy B, Timmins K, O’Mahony CA, Anton J, Civitello A, Garcha P, Loor G, Liao K, Shaffi A, Vierling J, Stribling R, Rana A, Goss JA (2020) Donor and transplant candidate selection for solid organ transplantation during the COVID-19 pandemic. Am J Transplant 20(11):3113–3122
Iwamoto Y, Sugioka Y, Chuman H, Masuda S, Hotokebuchi T, Kawai S, Yamamoto M (1997) Nationwide survey of bone grafting performed from 1980 through 1989 in Japan. Clin Orthop Relat Res 335:292–297
Khazaei M, Asgari R, Zarei E, Moharramzad Y, Haghighatkhah H, Sanei TM (2020) Incidentally diagnosed COVID-19 infection in trauma patients; a clinical experience. Arch Acad Emerg Med 8:e31
Komiya K, Nasuno S, Uchiyama K, Takahira N, Kobayashi N, Minehara H, Watanabe S, Itoman M (2003) Status of bone allografting in Japan - Nation-Wide Survey of bone grafting performed from 1995 through 1999. Cell Tissue Bank 4:217–220
Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J (2020) Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann Intern Med 173:1294–1303
Kumar D, Manuel O, Natori Y, Egawa H, Grossi P, Han SH, Fernandez-Ruiz M, Humar A (2020) COVID-19: a global transplant perspective on successfully navigating a pandemic. Am J Transplant 20:1773–1779
Li C, Ji F, Wang L, Wang L, Hao J, Dai M, Liu Y, Pan X, Fu J, Li L, Yang G, Yang J, Yan X, Gu B (2020) Asymptomatic and human-to-human transmission of SARS-CoV-2 in a 2-family cluster, Xuzhou, China. Emerg Infect Dis 26:1626–1628
Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, Jacquelinet C (2020) Organ procurement and transplantation during the COVID-19 pandemic. Lancet 395:e95–e96
Mahdavi A, Haseli S, Mahdavi A, Bakhshayeshkaram M, Foroumandi M, Nekooghadam SM, Raoufi M, Taheri MS (2020) The role of repeat chest CT scan in the COVID-19 pandemic. Acad Radiol 27:1049–1050
Shelton WR (2003) Arthroscopic allograft surgery of the knee and shoulder: indications, techniques, and risks. Arthroscopy 19(Suppl 1):67–69
Urabe K, Itoman M, Toyama Y, Yanase Y, Iwamoto Y, Ohgushi H, Ochi M, Takakura Y, Hachiya Y, Matsuzaki H, Matsusue Y, Mori S (2007) Current trends in bone grafting and the issue of banked bone allografts based on the fourth nationwide survey of bone grafting status from 2000 to 2004. J Orthop Sci 12:520–525
Vangsness CT Jr, Wagner PP, Moore TM, Roberts MR (2006) Overview of safety issues concerning the preparation and processing of soft-tissue allografts. Arthroscopy 22:1351–1358
WHO Laboratory Network (2020) First data on stability and resistance of SARS coronavirus compiled by members of WHO laboratory network
Zidan A, Alabbad S, Ali T, Nizami I, Haberal M, Tokat Y, Kamel R, Said H, Abdelaal A, Elsharkawy M, El FA, Sayed H, Al-Mousawi M, AlGhonaim M, Broering D (2020) Position statement of transplant activity in the middle east in era of COVID-19 pandemic. Transplantation 104:2205–2207
Acknowledgements
We thank DMC Corp for editing drafts of this manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Kentaro Uchida, Manabu Mukai, Masayuki Miyagi, Kensuke Fukushima, Katsufumi Uchiyama, Naonobu Takahira, Akiko Nakayama, Mai Matsumoto, Ken Urabe, Masashi Takaso, and Gen Inoue contributed to material preparation, data collection and analysis. Kentaro Uchida wrote the first draft of the manuscript. All authors commented on drafts of the manuscript prior to finalization. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study received ethical approval by the Ethics Review Board of Kitasato University (approval number: B20-132) for the use of an opt-out methodology.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uchida, K., Mukai, M., Miyagi, M. et al. Management of regional bone bank during declaration of a state of emergency concerning the COVID-19 in Japan. Cell Tissue Bank 22, 703–709 (2021). https://doi.org/10.1007/s10561-021-09908-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-021-09908-w