Abstract
Purpose
This meta-analysis aimed to evaluate the efficacy and safety of non-vitamin K antagonist oral anticoagulants (NOACs) compared with vitamin K antagonists (VKAs) in patients with atrial fibrillation (AF) and type 2 valvular heart disease (VHD).
Methods
We searched the PubMed, LILACS, and MEDLINE databases to retrieve, randomized controlled trials (RCTs) comparing NOACs and VKAs in patients with AF and type 2 VHD, excluding mitral stenosis (moderate to severe, of rheumatic origin) or mechanical heart valves. The efficacy outcomes assessed were stroke and systemic embolism (SE), while safety outcomes included major bleeding and intracranial hemorrhage (ICH).
Results
Seven RCTs, including 16,070 patients with AF and type 2 VHD, were included. NOACs reduced the risk of stroke/SE (relative risk [RR], 0.75; 95% confidence interval [CI], 0.64–0.89; P = 0.0005), with no significant difference in major bleeding (RR, 0.88; 95% CI, 0.64–1.21; P = 0.43). The risk of ICH was reduced with NOACs (RR, 0.46; 95% CI, 0.27–0.77; P = 0.003). For patients with AF and bioprosthetic heart valve (five trials, 2805 patients), stroke/SE risks (RR, 0.65, 95% CI, 0.44–0.96) with NOACs were superior to VKAs. Major bleeding risks without ENVISAGE TAVI AF trial (RR, 0.53; 95% CI, 0.30–0.94; P = 0.03) with NOACs were superior to VKAs. The risks of ICH (RR, 0.61; 95% CI 0.34–1.09; P = 0.09) with NOACs were comparable to VKAs.
Conclusions
NOACs demonstrate efficacy and safety in patients with AF and type 2 VHD and reduce the risk of stroke/SE and ICH when compared with those with VKAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) and valvular heart disease (VHD) frequently coexist, often presenting as an enlarged left atrium and influenced by a range of risk factors including aging, hypertension, diabetes mellitus, ischemic heart disease, and heart failure [1, 2]. Both conditions independently contribute to the risk of stroke and systemic embolism [3]. VHD is associated with an increased propensity for thromboembolic events, irrespective of the cardiac rhythm [4]. The risk of thromboembolism varies according to the valve disease type and lesion severity [5]. Consequently, the implementation of anticoagulation is a critical part of the treatment approach for individuals with VHD and AF [6]. Warfarin, an anticoagulant, is commonly prescribed for these patients to mitigate the risks associated with these conditions. However, the wide variation in individual effective doses, susceptibility to food or other drugs, and the need for frequent monitoring of international normalized ratio render the clinical effectiveness of warfarin unsatisfactory [7, 8]. Patients with AF may be prescribed different anticoagulation therapies, depending on the diagnosis and stage of VHD.
A recent consensus document has introduced the evaluating heart valve, rheumatic, or artificial (EHRA) classification system to guide the selection of the preferred oral anticoagulant for patients presenting with both AF and VHD [6]. Patients with EHRA type 1 VHD are those with mitral stenosis (moderate to severe, of rheumatic origin) or a mechanical heart valve and are referred to as patients with AF who need vitamin K antagonists (VKAs) therapy [6, 9]. Research has indicated that individuals with AF and type 1 VHD face an exceedingly elevated risk of thromboembolic occurrences, with an annual incidence rate of 25% in the absence of anticoagulation and 0.8% with anticoagulation measures in place [10]. Furthermore, the RE-ALIGN, INVICTUS, and PROACT trials have shown that these two groups of patients do not benefit from non-vitamin K antagonist oral anticoagulants (NOACs) [11,12,13]. Type 2 VHD includes native VHDs, such as mitral regurgitation, aortic regurgitation, aortic stenosis, tricuspid regurgitation, and bioprosthetic valves or valve repair. Patients with AF and type 2 VHD require either VKAs or NOACs, considering the CHA2DS2-VASc score risk factor components [6].
However, there is no definitive consensus regarding the selection of oral anticoagulants for AF patients with type 2 VHD. Physicians often prefer VKAs over NOACs, possibly due to the elevated risk of thromboembolic events associated with VHD and the absence of well-defined clinical criteria for type 2 VHD [14]. To address the existing evidence gap and resolve uncertainties, we conducted a systematic review and meta-analysis to evaluate the comparative effects of NOACs and VKAs in patients with AF and type 2 VHD.
Methods
This systematic review and meta-analysis were conducted in adherence to the guidelines set forth by the preferred reporting items for systematic reviews and meta-analyses framework [15].
Data Sources and Searches
We searched the PubMed, MEDLINE, and Cochrane Library databases, and extracted all relevant trials on this subject published up to December 2023. The search strategy for each database was as follows: “atrial fibrillation” AND (“valvular heart disease” OR “heart valve prosthesis” OR “heart valve prosthesis implantation”) AND (“warfarin” OR “coumadin” OR “vitamin K antagonist” OR “direct oral anticoagulant” OR “DOAC” OR “NOAC” OR “non-vitamin K antagonist oral anticoagulant” OR “novel oral anticoagulant” OR “new oral anticoagulant”) AND (“factor Xa inhibitors” OR “dabigatran” OR “rivaroxaban” OR “edoxaban” OR “betrixaban” OR “apixaban”). During the search, the subject and free words were combined according to specific trial adjustments. In addition, we searched the references of the retrieved articles to identify trials that were identified by the retrieval strategy described above (Appendix 1 in the Supplementary Information).
Eligibility Criteria
We included randomized controlled trials (RCTs) that compared NOACs—including dabigatran, rivaroxaban, apixaban, edoxaban, and betrixaban—with VKAs in adult patients with AF and type 2 valvular heart disease (VHD) [6].
The definition of AF is a supraventricular tachyarrhythmia with uncoordinated atrial electrical activation, resulting in ineffective atrial contraction, and documented on the electrocardiogram for > 30 s [3]. Type 2 VHD, which refers to AF patients with VHD needing therapy with a VKA or a non-VKA oral anticoagulant (NOAC), also taking into consideration CHA2DS2VASc score risk factor components, includes native VHDs, such as mitral regurgitation, aortic regurgitation, aortic stenosis, tricuspid regurgitation, and bioprosthetic valves or valve repair [6].
Exclusion Criteria
Exclusion criteria were defined to exclude studies that did not focus on the use of NOACs for AF and type 2 VHD, studies that recruited patients with rheumatic mitral valves and mechanical, observational studies, non-randomized controlled trials, animal studies, reviews, and publications that are duplicates reporting identical trials.
Evaluated Outcomes
Our primary endpoint for evaluation was treatment effectiveness in preventing stroke/SE. The primary safety endpoint was the incidence of major bleeding events [16], while intracranial hemorrhage (ICH) was considered a secondary outcome. When relevant, valvular or intracardiac thrombosis was included as a primary measure of efficacy [9].
Methods for the Inclusion and Exclusion of Studies
Two evaluators independently completed the preliminary search according to the search strategy and read relevant literature and abstracts independently. After excluding studies that did not meet the inclusion criteria, the full text of studies disagreed upon by the two evaluators in this study was read to confirm their inclusion or exclusion in the retrieved studies. In cases of further disagreement between the evaluators, a decision was reached through discussions.
Risk of Bias in Individual Studies
The risk of bias in the included studies was assessed using the criteria outlined in the Cochrane Review Manager (RevMan) version 5.4.1. The criteria for bias assessment encompassed (1) random allocation method, (2) distribution scheme hiding, (3) the blinding method used for the study participants, implementers of the treatment plan, and measurement of the research results, (4) integrity of the results, (5) selective reporting of research results, and (6) other sources of bias. For each included literature, “yes” (low degree of bias), “no” (high degree of bias), and “unclear” (lack of relevant information or uncertain bias) were judged for the above six items. Disagreement between the two evaluators was resolved through discussions with a third researcher.
Statistical Methods
The quantitative synthesis of data for this meta-analysis was carried out using the RevMan 5.4.1 software. The presence of publication bias was evaluated through funnel plot analysis, contingent on the number of studies included. Both clinical and methodological heterogeneities among the studies were examined. The chi-square test was employed to assess statistical heterogeneity. P > 0.1 and I2 < 50% indicated no statistical heterogeneity and a fixed-effects model was used for the analysis. If there was statistical heterogeneity (P < 0.1, I2 ≥ 50%), the heterogeneity could not be easily explained; a random effects model then was used or a sensitivity analysis was performed; If the data provided by the included studies could not be meta-analyzed, a descriptive analysis was performed. The measurement data are presented as mean difference and 95% confidence interval (CI). Count data are presented as relative risk (RR) and 95% CI. P < 0.05 was considered statistically significant.
We used the trial sequential analysis (TSA) with version 0.9 beta, developed by the Copenhagen Trial Unit in 2011 to evaluate the main outcomes in patients with type 2 valvular heart disease (VHD). This analysis aimed to determine if the data had enough power to assess treatment effects. In TSA, we calculated the needed information size and monitoring boundaries for alpha spending, based on a 5% Type I error risk, an 80% power (20% Type II error risk), pooled risk reduction, control group event rates, and heterogeneity. If the outcomes’ power reached significance, we interpreted it through the sample size or by exceeding the monitoring boundary.
Results
Characteristics
Study Selection
The literature retrieval and screening processes are shown in Fig. 1. Using this search strategy, 513 articles from the PubMed, LILACS, and MEDLINE databases were identified and recorded. After reading their titles and authors, 101 duplicate articles were excluded; further careful review of the abstract excluded 391 articles that included reviews, systematic reviews, and conference articles and did not conform to the inclusion criteria regarding study content, intervention measures, and control measures. After careful reading of the full text to review the study design and outcomes, studies were excluded, and 14 studies were subsequently removed because their original text could not be retrieved. Finally, seven studies were included in this meta-analysis [17,18,19,20,21,22,23]. Figure 1 illustrates the flowchart of the study selection and inclusion as a flowchart. A total of 16,070 patients (9176 in the new oral anticoagulant group and 6894 in the warfarin group) were included.
Study Characteristics
Among the studies included in the analysis, four were retrospective post-hoc subgroup analyses of RCTs, and three were double-blind experimental RCTs, with a subset of three studies focusing exclusively on patients with a bioprosthetic heart valve (BHV), either aortic or mitral. As depicted in Table 1, the trials encompassed a range of VHD types. The predominant form of type 2 VHD was native valvular heart disease, with over 2800 individuals having received bioprosthetic valve replacements or valve repair. The NOACs included in the studies were dabigatran, rivaroxaban, edoxaban, and apixaban. The first three drugs were compared in patients with various types of type 2 VHD, and the last drug was used for only native type 2 VHD cases.
Patient Characteristics
Table 2 details the principal clinical features and risk factors associated with bleeding and thromboembolic events among patients with AF and VHD treated with NOACs. The lowest and highest mean (± standard deviation) ages were 48.8 ± 10.4 and 82.1 ± 5.4 years, respectively. The results showed that patients with type 2 VHD often had heart failure, coronary artery disease, diabetes, history of stroke, systemic embolism, transient ischemic attack, and hypertension. Most types of atrial fibrillation were persistent. Approximately 60% of patients were taking warfarin at baseline but were randomized to either group. The mean or median percentage of time with an INR in the therapeutic range in the VKA group is > 60%.
Outcome Assessment
Efficacy Outcomes: Stroke and Systemic Embolism
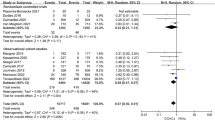
NOACs proved to be more efficacious than VKAs in patients with AF and type 2 VHD, exhibiting a reduced RR for stroke/SE (RR, 0.75; 95% CI, 0.64–0.89; P = 0.0006). The evidence from the studies was of high quality, with no heterogeneity (I2 = 0%; P = 0.68).
Safety Outcome: Major Bleeding and Intracranial Hemorrhage
There was no significant decrease in major bleeding events among patients with type 2 VHD treated with NOACs compared with those on VKAs (RR, 0.88; 95% CI, 0.64–1.21; P = 0.43). The evidence quality for this finding was low, with a high degree of heterogeneity across the studies (I2 = 85%; P < 0.0001).
Compared with VKAs, NOACs reduced the risk of ICH in patients with type 2 VHD (RR, 0.46; 95% CI, 0.27–0.77; P = 0.003). The evidence quality for this finding was low, with a high moderate heterogeneity across the studies (I2 = 60%; P = 0.03).
The forest plot for stroke/SE, major bleeding, and intracranial hemorrhage in patients with atrial fibrillation and type 2 valvular heart disease on anticoagulation is shown in Fig. 2, and the funnel plot is respectively shown in Fig. S1-3 (Appendix 2 in the supplementary information).
The forest plot illustrates the individual and pooled estimates of the risks associated with stroke/systemic embolism, major bleeding, and intracranial hemorrhage in patients with atrial fibrillation and type 2 valvular heart disease on anticoagulation. CI confidence interval, M–H Mantel–Haenszel, NOACs new oral anticoagulants, VKAs vitamin K antagonists; the asterisks indicate that the DAWA pilot study conducted by Rodrigues Duraes et al. (2016) only reported bleeding in the warfarin and dabigatran groups, and no reports of major bleeding and intracranial hemorrhage in the warfarin and dabigatran groups were reported, so they were not included in this analysis
Significant heterogeneity was observed in the safety analysis comparing NOACs to VKA in patients with type 2 VHD and AF, leading to the use of a random effects model to pool effect sizes. Given the potential differences in outcomes between bioprosthetic and native valves, a secondary analysis was performed for patients with bioprosthetic valves and AF.
Bioprosthetic Heart Valves and Secondary Analyses
For patients with bioprosthetic heart valves (BHV), five studies furnished comprehensive data: a subset from the ARISTOTLE trial [22, 24] involving BHV replacement or native valve repair (87 in the apixaban group vs. 69 in the VKAs group), a designated subgroup from the ENGAGE AF-TIMI trial [25] with 191 patients with BHV (121 in the edoxaban group vs. 70 in the VKAs group), a DAWA trial [21] pilot study including post-operative AF patients with bioprosthesis (15 in the dabigatran 110 mg twice daily group vs. 12 in the VKAs group), 1426 patients with AF from the ENVISAGE-TAVI AF trial [17] post transcatheter aortic valve replacement (713 in the edoxaban group vs. 713 in the VKAs group), and the RIVER trial’s [18] 1003 participants with bioprosthetic mitral valves (500 in the rivaroxaban group vs. 503 in the VKAs group). Aggregated data revealed that compared with VKAs, NOACs were more effective in reducing stroke and systemic embolism risks (RR, 0.65; 95% CI, 0.44–0.96), with no significant difference in major bleeding (RR, 0.76; 95% CI, 0.38–1.54) and ICH risks (RR, 0.61; 95% CI, 0.34–1.09) between NOACs and VKAs. The findings from the secondary analyses were consistent with the primary outcomes.
The sensitivity analysis of this group showed that the ENVISAGE-TAVI had a greater effect on heterogeneity. Compared with VKAs, NOACs reduced the risk of major bleeding in patients with bioprosthesis after this trial was excluded (RR, 0.53; 95% CI, 0.30–0.94; P = 0.03). The evidence quality for this finding was no heterogeneity (I2 = 0%; P = 0.64).
The forest plots for stroke/SE, major bleeding, ICH, and sensitivity analysis excluding the ENVISAGE-TAVI AF trial of major bleeding in patients with AF and BHV on anticoagulation are shown in Figs. 3 to 4 and the funnel plots are shown in Fig. S4–S7 (Appendix 2 in the Supplementary Information).
The forest plot illustrates the individual and pooled estimates of the risks associated with stroke/systemic embolism, major bleeding, and intracranial hemorrhage in patients with atrial fibrillation and bioprosthetic heart valves on anticoagulation. CI confidence interval, M–H Mantel–Haenszel, NOACs new oral anticoagulants, VKAs vitamin K antagonists
The forest plot illustrates the sensitivity analysis excluding the ENVISAGE-TAVI AF trial of the risks associated with major bleeding in patients with atrial fibrillation and bioprosthetic heart valves on anticoagulation. CI confidence interval, M–H Mantel–Haenszel, NOACs new oral anticoagulants, VKAs vitamin K antagonists
Risk of Bias in Individual Studies
In terms of bias assessment for the included studies in this meta-analysis, the Cochrane collaboration tool was employed. All seven studies utilized randomization and transparently reported the random sequence generation and allocation concealment. One study had a relatively high risk of bias and was of low quality. This was a prospective phase II pilot study with no blinding to outcome evaluation and with selective reporting. The remaining six studies were high quality, exhibiting low bias risk, complete outcome data, absence of selective reporting, and minimal biases related to follow-up and publication. The increased risk of bias was mainly due to the open-label design of three trials, and four trials conducted post-hoc analysis, which mainly explains the increase in “other bias.” The overall risk of bias was deemed mild to moderate (Appendix 3 in the supplementary information).
Discussion
The main findings of this systematic review include (i) NOACs, compared with VKAs, lessened the risk of stroke, systemic embolism, and ICH in individuals with AF and type 2 VHD; (ii) there was no significant difference in the rate of major bleeding between the anticoagulation therapies for these patients; (iii) NOACs compared with VKAs were associated with a notable decrease in stroke and systemic embolism in patients with AF post-BHV implantation compared to VKAs; and (iv) no elevated risks were observed for intracranial and major bleeding in patients with BHVs. This review is, to our knowledge, the inaugural study to distinctly assess the outcomes for the subgroup of patients with type 2 VHD—excluding those with mitral stenosis (moderate to severe, of rheumatic origin) or mechanical heart valves—who were managed with VKAs or NOACs, with risk factors evaluated using the CHA2DS2-VASc score.
The efficacy analysis demonstrated that NOACs provided a significant protective effect against stroke and systemic embolism for patients with AF and type 2 VHD. However, there was no significant reduction in the risk of major bleeding within this group. Notably, the risk of ICH was substantially reduced by half in these patients. Significant heterogeneity was observed in the safety analysis comparing NOACs to VKA in patients with type 2 VHD and AF, leading to the use of a random-effects model to pool effect sizes, mainly due to the results of the ROCKET AF and ENVISAGE-TAVI AF trials. The ROCKET AF trial suggested an increased risk of major bleeding with rivaroxaban compared to warfarin, while the risk of ICH did not reach statistical significance, which may be attributed to the type 2 VHD population’s characteristics: a mean CHA2DS2-VASc score of 3.5, a mean HAS-BLED score of 2.8, and an older age demographic (mean, 75 years), indicating a higher stroke and bleeding risk. In the ENVISAGE-TAVI AF study, edoxaban did not result in worse net endpoint events compared to VKAs, showing better adherence and efficacy but also a lower safety profile. The high risk of bleeding in the edoxaban, n group may be attributed to various factors. First, most enrolled patients were older adults, with an average age of 82 years. Second, the edoxaban group had a high incidence of gastrointestinal bleeding events, which may be related to the tendency of high bleeding risk. Moreover, the ENVISAGE-TAVI AF trial observed that VKAs had lower adherence and compliance rates than edoxaban, which could paradoxically relate to a lower observed bleeding risk. Nonetheless, the rates of net adverse clinical events and major bleeding were comparable between patients receiving VKAs and those on a daily 30 mg dose of edoxaban, particularly among those who met the criteria for dose adjustment during the trial. While acknowledging the unique characteristics of this subgroup, the collective evidence assessed via trial sequential analysis (TSA) affirms the robustness of the pooled data pertaining to stroke/SE prevention. This analysis also indicates that the reduction in major bleeding risk is consistently significant when compared to Vitamin K Antagonists (VKAs).
Approximately 20% of patients with AF have VHD, with the majority not having significant mitral stenosis or mechanical heart valves. For patients with AF and type 1 VHD, VKAs are recommended due to limited data supporting the use of NOACs in this population [26]. The choice of antithrombotic therapy for AF and type 2 VHD remains a focal point in contemporary research. Moon et al. [27] conducted a Korean population-based study to evaluate the safety and efficacy of VKAs versus NOACs in patients with AF and type 2 VHD. By employing a propensity score matching approach to mitigate confounding factors, they discovered that NOACs, compared with warfarin, significantly lowered the risk of ischemic stroke and bleeding events. Caldeira et al. and Yasmin et al. reported that certain NOACs, such as apixaban, dabigatran, and edoxaban, are particularly beneficial in reducing the risk of intracranial bleeding, regardless of the VHD status [28]. These findings are supported by a strong evidence base derived from trial sequential analysis, which underscores the correlation between stroke prevention and a decrease in ICH events. Consistent with this, our study also observed a roughly 50% protective effect of NOACs over warfarin concerning ICH, despite notable heterogeneity among the studies.
The thromboembolic risk in patients with AF and concomitant bioprosthesis valve or valve repair appears not to be markedly different from that of common native VHD [29]. Given the potential differences in our outcomes between bioprosthetic and native valves, a secondary analysis was performed for patients with bioprosthetic valves and AF. Our analysis, pooling data from five studies involving over 2,800 patients with AF and BHV or valve repair, supports the benefits of NOACs for this patient group The efficacy analysis demonstrated that NOACs provided a significant protective effect against stroke and systemic embolism for patients with AF and bioprosthesis valve. There was no significant reduction in the risk of major bleeding and ICH within this group. Moderate statistical heterogeneity was noted in major bleeding, then we conducted a sensitivity analysis. The sensitivity analysis of this group showed that the ENVISAGE-TAVI had a greater effect on heterogeneity. After removing this study, there was no heterogeneity between the studies. And the analysis results without the ENVISAGE-TAVI were changed, indicating that the stability of the results of this group was poor. and it is suggested that future researchers should conduct more studies on this aspect. Variability in concomitant antiplatelet therapy for stroke or coronary artery disease could also be a significant source of heterogeneity in bleeding risk analysis. Given the exploratory nature of the analysis, patients with AF combined with TAVI should be excluded from the interpretation of safety results, especially for the safety measure of major bleeding.
The consensus on the selection of oral anticoagulants for patients with AF or type 2 VHD is not definitive. However, it is important to recognize that NOACs are more effective than VKAs and offer additional advantages, such as convenience [30,31,32]. Physicians should be aware that VHD forms other than mitral stenosis or mechanical heart valve implantation should not preclude the use of NOACs in these patients. Although NOACs are widely prescribed, the “valvular” AF label can lead to misinterpretation, potentially excluding patients who could benefit from these medications. Given the cost-effectiveness of NOACs, the dissemination of our findings is relevant to policymakers. The European Society of Cardiology’s AF guidelines do not directly factor valvular diseases (except type 1 VHD) into stroke risk estimation or the decision on the type of anticoagulant treatment. Thus, clinical decisions for anticoagulation in this subgroup mirror those for patients without VHD.
Limitation
Our findings are constrained by methodological challenges inherent in individual studies and meta-analyses. The meta-analysis was based on study-level data rather than individual patient data. Moreover, most results were derived from post-hoc analyses of large RCTs, which, despite moderate-to-high heterogeneities, suggest the potential efficacy of NOACs. Further research is warranted to investigate the efficacy and safety of NOACs in patients with AF and type 2 VHD, with attention to disease subtype implications.
Conclusion
Compared with VKAs, NOACs significantly decrease the risk of stroke/SE risks and ICH in patients with AF and type 2 VHD who do not have mechanical heart valves or mitral stenosis. The overall risk of major bleeding did not increase, although bleeding risk results showed heterogeneity among trials. In AF patients with BHVs, NOACs showed superior efficacy in reducing stroke/SE risks, with similar safety in preventing ICH, compared to VKAs. Further research is required to evaluate the impact of NOACs compared to VKAs on the reduction of major bleeding risk in patients with AF and BHVs.
Data Availability
All authors warrant that all data, materials, software applications, or custom code support their publication and conform to site standards.
Code Availability
Not applicable.
References
Eleid MF, Nkomo VT, Pislaru SV, Gersh BJ. Valvular heart disease: new concepts in pathophysiology and therapeutic approaches. Annu Rev Med. 2023;74:155–70. https://doi.org/10.1146/annurev-med-042921-122533.
Sagris M, Vardas EP, Theofilis P, et al. Atrial fibrillation: pathogenesis, predisposing factors, and genetics. Int J Mol Sci. 2021;23(1):6. https://doi.org/10.3390/ijms23010006.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022;145(18):e876–94. https://doi.org/10.1161/cir.0000000000001062.
Doi K, Ogawa H, Ishigami K, et al. Impact of valvular heart disease on mortality, thromboembolic and cardiac events in japanese patients with atrial fibrillation - the Fushimi AF Registry. Circ J. 2020;84(5):714–22. https://doi.org/10.1253/circj.CJ-19-1158.
Melgaard L, Overvad TF, Jensen M, et al. Thromboembolic risk in nonanticoagulated patients with atrial fibrillation and valvular heart disease. JACC Clin Electrophysiol. 2020;6(13):1672–82. https://doi.org/10.1016/j.jacep.2020.07.005.
Lip GYH, Collet JP, Caterina R, et al. Antithrombotic therapy in atrial fibrillation associated with valvular heart disease: a joint consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology working group on thrombosis, endorsed by the ESC working group on valvular heart disease, Cardiac Arrhythmia Society of Southern Africa (CASSA), Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), South African Heart (SA Heart) Association and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). Europace. 2017;19(11):1757–8. https://doi.org/10.1093/europace/eux240.
Hughey AB, Gu X, Haymart B, et al. Warfarin for prevention of thromboembolism in atrial fibrillation: comparison of patient characteristics and outcomes of the “real-world” Michigan anticoagulation quality improvement initiative (MAQI(2)) registry to the RE-LY, ROCKET-AF, and ARISTOTLE trials. J Thromb Thrombolysis. 2018;46(3):316–24. https://doi.org/10.1007/s11239-018-1698-y.
Amin A, Deitelzweig S, Jing Y, et al. Estimation of the impact of warfarin’s time-in-therapeutic range on stroke and major bleeding rates and its influence on the medical cost avoidance associated with novel oral anticoagulant use-learnings from ARISTOTLE, ROCKET-AF, and RE-LY trials. J Thromb Thrombolysis. 2014;38(2):150–9. https://doi.org/10.1007/s11239-013-1048-z.
Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2024;149(1):e1–156. https://doi.org/10.1161/cir.0000000000001193.
Fleming HA, Bailey SM. Mitral valve disease, systemic embolism and anticoagulants. Postgrad Med J. 1971;47(551):599–604. https://doi.org/10.1136/pgmj.47.551.599.
Eikelboom JW, Connolly SJ, Brueckmann M, et al. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med. 2013;369(13):1206–14. https://doi.org/10.1056/NEJMoa1300615.
Connolly SJ, Karthikeyan G, Ntsekhe M, et al. Rivaroxaban in rheumatic heart disease-associated atrial fibrillation. N Engl J Med. 2022;387(11):978–88. https://doi.org/10.1056/NEJMoa2209051.
Wang TY, Svensson LG, Wen J, et al. Apixaban or warfarin in patients with an on-x mechanical aortic valve. NEJM Evid. 2023;2(7):EVIDoa2300067. https://doi.org/10.1056/EVIDoa2300067.
Vedovati MC, Reboldi G, Agnelli G, Verdecchia P. Type 2 valvular heart disease affects decision making for anticoagulation in patients with atrial fibrillation: the UMBRIA-fibrillazione atriale prospective study. TH Open. 2019;3(2):e157–64. https://doi.org/10.1055/s-0039-1692202.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84. https://doi.org/10.7326/m14-2385.
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4. https://doi.org/10.1111/j.1538-7836.2005.01204.x.
Van Mieghem NM, Unverdorben M, Hengstenberg C, et al. Edoxaban versus vitamin K antagonist for atrial fibrillation after TAVR. N Engl J Med. 2021;385(23):2150–60. https://doi.org/10.1056/NEJMoa2111016.
Duraes AR, Bitar YSL. Rivaroxaban in patients with atrial fibrillation and a bioprosthetic mitral valve. N Engl J Med. 2021;384(10):975. https://doi.org/10.1056/NEJMc2035891.
De Caterina R, Renda G, Carnicelli AP, et al. Valvular heart disease patients on edoxaban or warfarin in the ENGAGE AF-TIMI 48 Trial. J Am Coll Cardiol. 2017;69(11):1372–82. https://doi.org/10.1016/j.jacc.2016.12.031.
Ezekowitz MD, Nagarakanti R, Noack H, et al. Comparison of dabigatran and warfarin in patients with atrial fibrillation and valvular heart disease: the RE-LY trial (randomized evaluation of long-term anticoagulant therapy). Circulation. 2016;134(8):589–98. https://doi.org/10.1161/circulationaha.115.020950.
Durães AR, de Souza RP, de Almeida NB, et al. Dabigatran versus warfarin after bioprosthesis valve replacement for the management of atrial fibrillation postoperatively: DAWA pilot study. Drugs R D. 2016;16(2):149–54. https://doi.org/10.1007/s40268-016-0124-1.
Avezum A, Lopes RD, Schulte PJ, et al. Apixaban in comparison with warfarin in patients with atrial fibrillation and valvular heart disease: findings from the apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation (ARISTOTLE) trial. Circulation. 2015;132(8):624–32. https://doi.org/10.1161/circulationaha.114.014807.
Breithardt G, Baumgartner H, Berkowitz SD, et al. Clinical characteristics and outcomes with rivaroxaban vs. warfarin in patients with non-valvular atrial fibrillation but underlying native mitral and aortic valve disease participating in the ROCKET AF trial. Eur Heart J. 2014;35(47):3377–85. https://doi.org/10.1093/eurheartj/ehu305.
Guimarães PO, Pokorney SD, Lopes RD, et al. Efficacy and safety of apixaban vs warfarin in patients with atrial fibrillation and prior bioprosthetic valve replacement or valve repair: insights from the ARISTOTLE trial. Clin Cardiol. 2019;42(5):568–71. https://doi.org/10.1002/clc.23178.
Carnicelli AP, De Caterina R, Halperin JL, et al. Edoxaban for the prevention of thromboembolism in patients with atrial fibrillation and bioprosthetic valves. Circulation. 2017;135(13):1273–5. https://doi.org/10.1161/circulationaha.116.026714.
Nieuwlaat R, Capucci A, Camm AJ, et al. Atrial fibrillation management: a prospective survey in ESC member countries: the Euro heart survey on atrial fibrillation. Eur Heart J. 2005;26(22):2422–34. https://doi.org/10.1093/eurheartj/ehi505.
Moon I, Lee SR, Choi EK, et al. Non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation and valvular heart disease. J Clin Med. 2019;8(10):1624. https://doi.org/10.3390/jcm8101624.
de Souza Lima Bitar Y, Neto MG, Filho JAL et al. Comparison of the new oral anticoagulants and warfarin in patients with atrial fibrillation and valvular heart disease: systematic review and meta-analysis. Drugs R D. 2019;19(2):117–26. https://doi.org/10.1007/s40268-019-0274-z.
De Caterina R, Camm AJ. What is ‘valvular’ atrial fibrillation? A reappraisal Eur Heart J. 2014;35(47):3328–35. https://doi.org/10.1093/eurheartj/ehu352.
Urbaniak AM, Strøm BO, Krontveit R, Svanqvist KH. Prescription patterns of non-vitamin K oral anticoagulants across indications and factors associated with their increased prescribing in atrial fibrillation between 2012–2015: a study from the Norwegian prescription database. Drugs aging. 2017;34(8):635–45. https://doi.org/10.1007/s40266-017-0476-4.
Loo SY, Dell’Aniello S, Huiart L, Renoux C. Trends in the prescription of novel oral anticoagulants in UK primary care. Br J Clin Pharmacol. 2017;83(9):2096–106. https://doi.org/10.1111/bcp.13299.
Wu Y, Zhang C, Gu ZC. Cost-effectiveness analysis of direct oral anticoagulants vs vitamin K antagonists in the elderly with atrial fibrillation: insights from the evidence in a real-world setting. Front Cardiovasc Med. 2021;8:675200. https://doi.org/10.3389/fcvm.2021.675200.
Funding
This work was supported by the Natural Science Foundation of Hebei Province, the Key Science and Technology Research Program of Hebei Provincial Health Commission, the Industry University Research Cooperation Special Project, and the Hebei Province Finance Department Project (grant numbers [H2022206295], [20230991], [CXY2024020], and [LS202214]).
Author information
Authors and Affiliations
Contributions
Xiaoyun Liang and Shangyu Liu conceived and designed the study. Lishuang Ji and Fangfang Ma collected the data. Guoyuan Song and Fang Li performed the analyses. Xiaoyun Liang and Shangyu Liu wrote the paper. Gang Liu edited the entire manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study used a meta-analysis approach with data derived from previously published studies that were systematically statistically integrated and analyzed. No ethical review or informed consent was required for this study.
Consent to Participate
The data involved had been publicly released and did not involve direct intervention or collection of personal information from new participants.
Consent for Publication
All participants should appear in the manuscript.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, X., Liu, S., Ji, L. et al. Efficacy and Safety of Non-Vitamin K Antagonist Oral Anticoagulants Compared with Vitamin K Antagonists in Patients with Atrial Fibrillation and Type 2 Valvular Heart Disease: A Systematic Review and Meta-Analysis. Cardiovasc Drugs Ther (2024). https://doi.org/10.1007/s10557-024-07616-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-024-07616-7