Abstract
Purpose
Radial artery occlusion (RAO) is an unresolved complication after transradial artery (TRA) puncture. The aim of this observational study was to assess the feasibility and safety of retrograde recanalization of RAO through distal transradial access (dTRA).
Methods
From June 2021 to March 2022, 28 consecutive patients with successful puncture and intubation through the dTRA in the anatomical snuffbox and RAO confirmed by angiography were enrolled.
Results
Among the 28 patients, 27 (96.4%) patients with RAO were successfully retrogradely recanalized through the dTRA and successfully underwent coronary angiography or coronary intervention. After the procedure, only 1 (3.7%) patient developed a forearm hematoma, and there were no other bleeding complications or nerve disorders.
Conclusions
DTRA is a safe and feasible approach for retrograded recanalization of RAO, with a high procedure success rate and few complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transradial artery access (TRA) has been used for more than 90% [1] of coronary catheterizations (CC) and can reduce the complications related to the approach site and improve the comfort of early walking for patients compared with the transfemoral artery approach [2, 3]. However, TRA also has some complications, such as hematoma, arteriovenous fistula, pseudoaneurysm, osteofascial compartment syndrome, and radial artery occlusion (RAO) [4]. The PROPHET study (Prevention of Radial Artery Occlusion—Patent Hemostasis Evaluation Trial) showed that rates of RAO varied from 5 to 12% and 1.8 to 7% at the 24-h and 30-day follow-ups, respectively [5]. In addition, the failure rates of a second puncture and intubation using the same radial artery (RA) are 3.5% for males and 7.9% for females [6]. Patients with RAO may experience ischemic symptoms, and the TRA approach cannot be used in further catheterizations.
The distal transradial artery (dTRA) is an alternative site for radial artery puncture for CC, including coronary angiography (CAG) and percutaneous coronary intervention (PCI) [7]. Compared with the TRA approach, the dTRA approach has certain advantages, such as faster hemostasis and a lower risk of RAO [8]. The safety and feasibility of dTRA for CC have been demonstrated in a number of studies, but there are few data about RAO recanalization and complete CC through the dTRA approach.
Accordingly, this observational study assessed the success rate of retrograde recanalization of RAO through the dTRA approach.
Methods
Study Population
This was a single-center observational study conducted at Fuwai Hospital from June 2021 to March 2022. Patients with a history of TRA were routinely examined for RAO before repeat CC. If the RA pulse was absent, but the distal RA pulse was good, then the dTRA was used first. Finally, 28 consecutive patients who had a successful puncture and intubation of the dTRA at the anatomical snuffbox were enrolled in the study. The patients signed informed consent forms, and the study was reviewed by the Ethics Committee of Fuwai Hospital (2021-1501, Beijing, China).
Procedural Details
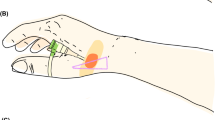
All CC procedures were performed by Dr. Lijian Gao, who was experienced in the dTRA approach. No Doppler ultrasound was performed prior to puncture. Before puncture, the patient formed a fist to fully expose the anatomical snuffbox (AS) area, which helped in feeling and choosing the site with the strongest pulse for puncture (Fig. 1). Local anesthesia with 2% lidocaine was administered in the AS area. The puncture was performed using a Terumo angiocatheter needle at an angle of approximately 30–45° (Fig. 2). After observing the blood return, angiography was performed using a 5-ml syringe to confirm RAO. Then, a percutaneous coronary intervention (PCI) guidewire was used to attempt to pass through the occluded segment of the RA. When the guidewire was successfully passed through the RA to the brachial artery or subclavian artery, the puncture needle was withdrawn, a balloon with a small diameter should be used demonstrating smooth passage to confirm that it is in the true lumen, and then, the sheath can be inserted. If the occluded segment is at proximal to the RA, the sheath can be inserted only 2–3 cm into the distal radial so that it does not reach the occluded segment, and then, balloon dilation is performed at the site of occluded RA; if the residual stenosis is still severe, progressively larger balloons were used for repeated dilation until the stenosis is relieved (Fig. 3A–D). After the resumption of RA blood flow, we injected 3000 U heparin via the sheath and then inserted a 5-Fr Terumo TIG diagnostic catheter to perform CAG (Fig. 4). For PCI, the sheath was changed to a 6-Fr or 7-Fr sheath, and unfractionated heparin (100 U/kg) was administered to the patients. After the CC procedure, angiography was repeated through the sheath to show the recanalized RA. We then removed the sheath, and the puncture site in the AS was compressed with gauze and a bandage for 4–6 h (Fig. 5).
Endpoints and Definitions
The primary endpoints of the study were the success rate of retrograde recanalization of RAO through the dTRA approach, defined as blood flow restoration by angiography. Nerve disorders are defined as finger dysfunction and numbness.
Statistical Analysis
Statistical analysis was performed using SPSS 22.0 statistical software. The measurement data are described as the mean ± standard deviation (x ± s), and the count data are expressed as a percentage (%).
Results
Baseline Patient Characteristics
The baseline characteristics of the study population are shown in Table 1. Among the 28 patients, 20 (71.4%) were male, with an average age of 59 ± 14 years. A total of 27 patients (96.4%) had previous PCI therapy, and 11 patients (39.3%) had a history of PCI ≥ 2 times through the TRA. All of them took dual antiplatelets and statins orally.
Procedural Characteristics
Twenty-seven (96.4%) patients were punctured through the right dTRA, and 1 patient was punctured through the left dTRA. The average number of attempts was 1.6 ± 0.8, and the average puncture time was 4.6 ± 3.4 min. Twenty-two (78.6%) patients required one PTCA guidewire, 5 (17.9%) patients required two PTCA guidewires, and only 1 (3.6%) patient required 3 PTCA guidewires for retrograde RAO. Among them, 27 patients’ guidewires were successfully passed through the occluded RA to the brachial artery or the subclavian artery, and only one failed. One balloon was used in 12 (42.9%) patients, two balloons in 13 (46.4%) patients, and three balloons in 2 (7.1%) patients to sufficiently restore the RAO. The successful rate of retrograde recanalization of RAO was 96.4% (27/28) (Table 2).
Only one patient failed. This patient was a 44-year-old male who underwent PCI 1 year prior via the right TRA. After successful puncture of the right dTRA, both the Pilot 50 and Fielder XTA guidewires failed to pass through the occluded segment of the RA, and the procedure was then changed to the brachial artery route.
All 27 patients who had a successful retrograded recanalization RAO underwent CAG, including 17 (63.0%) patients who underwent PCI. In fourteen (51.9%) patients, the sheath was changed to a 6-Fr sheath, and in 3 (11.1%), it changed to a 7-Fr sheath. The average duration of angiography and PCI was 13 ± 8 min and 60 ± 30 min, respectively. The average compression hemostasis time was 3.1 ± 0.4 h. Only one patient had a forearm hematoma (3.7%), and there were no other bleeding complications or nerve disorders, such as finger dysfunction or numbness (Table 3).
The baseline characteristics and procedural characteristics of each patient are shown in Table 4.
Discussion
The main finding of this observational clinical study was the high acceptable success rate of the dTRA approach for retrograde recanalization of RAO caused by previous cardiac catheterization. Thus, the dTRA approach is considered safe and feasible for this purpose.
Currently, TRA is recommended by ESC guidelines as the standard approach for CAG and PCI [9]. However, RAO is still an unwell-resolved complication of the TRA approach, and with the rapid increase in the use of TRA, the number of RAO patients is also rising [10, 11]. Factors associated with RAO include body mass index, diabetes mellitus, female sex, repeated TRA, large sheath size, anticoagulant usage, long operation, and compression time [11, 12]. Most RAO patients will not experience hand ischemia owing to the dual vascular supply of the palmar arch. Thus, the incidence of RAO may be underestimated in the real world [13]. However, for some patients, RAO still affected the physical activity of the arm or caused numbness. More importantly, RAO limits future utilization of the RA, including repeated CAG and PCI, for establishing dialysis access and for use in bypass graft in coronary artery bypass graft (CABG) surgery [8]. Therefore, finding a way to recanalize RAO has become very important.
The dTRA was first reported by Kiemeneij as an alternative access for CC in 2017 [7]. Compared with the TRA approach, the dTRA approach has advantages in terms of patient comfort, faster hemostasis, and a lower risk of RAO, which has attracted the attention of cardiologic interventionalists [14, 15]. It was found that the RAO can be opened through the dTRA. Our team reported successful angioplasty via the dTRA in recanalizing the right RAO of a 68-year-old man with a history of PCI, and a 3-month follow-up vascular ultrasound showed that the RA had smooth blood flow and no stenosis [16]. Some small-scale case series have suggested that dTRA is safe and feasible for retrograde recanalization of RAO, with a success rate of approximately 88–93% [17, 18]. In the present study, the success rate was 96.7% with very low complications, and successful patients underwent CAG and PCI. The high success rate is important to maintain radial access for future procedures.
There are some technical considerations recommended for recanalizing an RAO. First, successful dTRA puncture in the AS area is crucial. The pulsation of the distal RA in the AS area must be palpable or ultrasound-guided to improve the puncture success rate. Second, after successful puncture, a guidewire used for coronary balloon angioplasty is used to cross the RAO. The procedure was similar to PCI. The “knuckle” technique can be used to retrograde the guidewire to the brachial artery (Fig. 3B). In this study, successful retrograded RAO was achieved in 23 patients with Pilot 50, which is a hydrophilic PTCA guidewire. For the other patients, in whom Pilot 50 failed to be applied, 3 patients were changed to Fielder XTA, which is a hydrophilic guidewire, and the other patient was changed to Pilot 150, which has greater hardness. Only one patient failed with both Pilot 50 and Fielder XTA. In most patients, the occluded RA can be passed through by using a single hydrophilic guidewire. If it fails, it can be changed to another hydrophilic guidewire. Because RAO is different from coronary artery occlusion, the occlusion site is mainly thrombosis, and there is no need for a high tip-load guidewire such as Confianza Pro 12 or Gaia Third. Our experience was that the combined application of hydrophilic guidewire will improve the success rate of retrograde guidewire passage. Third, a small-diameter balloon size (1.25–1.5 mm) should be used to check if it is in the true vascular lumen; then, a balloon angioplasty is performed repeatedly at the occluded segment of RA with a larger balloon (diameter of 2.0–2.5 mm). Our principle of management is to use balloon dilation from small to large to achieve satisfactory dilation of the occluded radial artery. After it is confirmed that the sheath can be placed in the vascular lumen, subsequent CAG and PCI can be performed smoothly.
In this study, only one patient had a hematoma after the procedure. Although the experience with this technique is rather limited, there are several suggestions to improve outcomes. First, the surgeon should be experienced in dTRA, especially with a high rate of successful access. Ultrasound guidance can improve the successful puncture rate [19]. Second, when the guidewire successfully passes the RAO, a balloon with a small diameter should be used demonstrating smooth passage to confirm that it is in the true lumen, and then, the sheath can be inserted, which can avoid vascular injury and reduce the risk of bleeding. If the occluded segment is proximal to the RA, the sheath can be inserted only 2–3 cm into the distal radial so that it does not reach the occluded segment. Whether the sheath or balloon dilation is advanced depends on the location of the occluded segment of the RA. Finally, after CAG and PCI, radial arteriography should be performed to check whether there is a serious RA injury.
The long-term result of retrograde recanalization of RAO remains unclear. Small studies showed that the patency rates at 3, 6, and 12 months were 48.7%, 43.6%, and 35.9%, respectively. Balaban and Elevli showed that for 14 patients given drug-coated balloon (DCB) treatment after angioplasty, the patency rate was only 33.4% at the 1-month follow-up [16]. Such a low patency rate may be due to the different pathological mechanisms between RAO and coronary atherosclerosis [20]. No stent was used in the radial artery because the long-term patency rate was uncertain, and it interfered with future catheterizations.
Limitations
First, this is a single-center observational study with a small sample size, and not all the RAO patients were screened and had their data recorded. Therefore, we do not have data on how many patients with RAO were screened and found unacceptable. The data we are currently collecting can answer this question in the future. Second, not all patients underwent vascular ultrasound examination before and after the procedure, and the long-term patency rate of the RA is unknown. Third, intraluminal imaging was not performed in RA, which may be helpful for understanding the structure of RA for follow-up treatment. In the future, how to ensure the long-term patency rate of RA may be our research direction.
Conclusions
DTRA is a safe and feasible approach for retrograded recanalization of RAO, with a high procedure success rate and few complications.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code Availability
Statistical analysis was performed using SPSS 22.0 statistical software.
Abbreviations
- CC:
-
Cardiac catheterization
- TRA:
-
Transradial access
- RAO:
-
Radial artery occlusion
- RA:
-
Radial artery
- dTRA:
-
Distal transradial access
- CAG:
-
Coronary angiography
- PCI:
-
Percutaneous coronary intervention
- CAD:
-
Coronary artery disease
- CABG:
-
Coronary artery bypass grafting
- PTCA:
-
Percutaneous transluminal coronary angioplasty
References
Wang H, Gao Z, Yuan J, et al. Association of body mass index with mortality in Chinese patients after percutaneous coronary intervention: a large single-center data. Cardiovasc Ther. 2017;35(4):1–8.
Rao SV, Dharma S. 25 years of transradial intervention: looking back and anticipating what is ahead. JACC Cardiovasc Interv. 2017;10(22):2266–8.
Agostoni P, Biondi-Zoccai GG, de Benedictis ML, Rigattieri S, Turri M, Anselmi M, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004;44(2):349–56.
Coomes EA, Haghbayan H, Cheema AN. Distal transradial access for cardiac catheterization: a systematic scoping review. Catheter Cardiovasc Interv. 2020;96(7):1381–9.
Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion-patent hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Catheter Cardiovasc Interv. 2008;72(3):335–40.
Sakai H, Ikeda S, Harada T, Yonashiro S, Ozumi K, Ohe H, et al. Limitations of successive transradial approach in the same arm: the Japanese experience. Catheter Cardiovasc Interv. 2001;54(2):204–8.
Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and intervention (ldTRI). Eurointervention. 2017;13(7):851–7.
Corcos T. Distal radial access for coronary angiography and percutaneous coronary intervention: a state-of-the art review. Catheter Cardiovasc Interv. 2019;93(4):639–44.
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Hahalis G, Aznaouridis K, Tsigkas G, Davlouros P, Xanthopoulou I, Koutsogiannis N, et al. Radial artery and ulnar artery occlusions following coronary procedures and the impact of anticoagulation: ARTEMIS (Radial and Ulnar Artery Occlusion Meta-AnalysIS) systematic review and meta-analysis. J Am Heart Assoc. 2017;6(8):e005430.
Avdikos G, Karatasakis A, Tsoumeleas A, Lazaris E, Ziakas A, Koutouzis M. Radial artery occlusion after transradial coronary catheterization. Cardiovasc Diagn Ther. 2017;7(3):305–16.
Garg N, Madan BK, Khanna R, Sinha A, Kapoor A, Tewari S, et al. Incidence and predictors of radial artery occlusion after transradial coronary angioplasty: doppler-guided follow-up study. J Invasive Cardiol. 2015;27(2):106–12.
Ali S, Abdullah MS, Abdelrahman K, Ali A, Faisal F, Ali A. Total radial artery occlusion following transradial access: complete recanalization via the anatomical snuffbox. Methodist Debakey Cardiovasc J. 2020;16(4):314–7.
Sgueglia GA, Giorgio AD, Gaspardone A, Babunashvili A. Anatomic basis and physiological rationale of distal radial artery access for percutaneous coronary and endovascular procedures. JACC Cardiavasc Interv. 2018;11(20):2113–9.
Al-Azizi KM, Grewal V, Gobeil K, Maqsood K, Haider A, Mohani A, et al. The left distal transradial artery access for coronary angiography and intervention: a US experience. Cardiovasc Revasc Med. 2019;20(9):786–9.
Song K, Wang H, Li H, Cui Y, Gao L. A case of using the distal radial artery to open an occluded radial artery. JACC Case Rep. 2020;2(15):2432–3.
Balaban Y, Elevli MG. It is both possible and safe to perform coronary angiography through the same radial artery, after retrograde recanalization of radial artery occlusion, following a previous coronary angiography. J Interv Cardiol. 2018;31(6):957–63.
Yuan F, Zuo K, Yang Y, Gao Y, Liu L, Ding X, et al. Distal transradial access: a safe and feasible approach for coronary catheterization in cases of total radial artery occlusion. Journal of Cardiovascular Translational Research. J Cardiovasc Transl Res. 2022;15(5):1203–11.
Hadjivassiliou A, Kiemeneij F, Nathan S, et al. Ultrasound-guided access to the distal radial artery at the anatomical snuffbox for catheter-based vascular interventions: a technical guide. EuroIntervention. 2021;16(16):1342–8.
Kitrou P, Parthipun A, Diamantopoulos A, Padayachee S, Karunanithy N, Ahmed I, et al. Paclitaxel-coated balloons for failing peripheral bypass grafts: the BYPACS study. J Cardiovasc Surg (Torino). 2014;55(2):217–24.
Acknowledgements
The authors are grateful to the staff in the Department of Cardiology and Catheterization Laboratory, Fu Wai Hospital, Yunnan Fuwai Cardiovascular Hospital, and the People’s Hospital of Dehui City for their support in patient registration and data collection.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and publication of this article. This research was supported by the Yunnan Provincial Cardiovascular Disease Clinical Medical Center Project (No. FZX2019-06-01, 2022FYKY086), National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital, Chinese Academy of Medical Sciences (CAMS) (Grant No. NCRC2020013), and CAMS Innovation Fund for Medical Sciences (CIFMS) (2022-I2M-C&T-B-04).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Huanhuan Wang, Cheng Cui, Haiming Liu, Bo Zhang, Tao Tian, Shaodong Ye, Weixian Yang, Bo Xu, and Lijian Gao. The first draft of the manuscript was written by Huanhuan Wang and Cheng Cui, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Fuwai Hospital (2021-1501, Beijing, China).
Consent to Participate
Prior to enrollment, the contents of the study were explained to the patients using explanatory documents and consent documents, and written consent was obtained. If a patient withdrew consent during the observation period, all existing data collected from the patient were discarded.
Consent for Publication
The authors affirm that the human research participants provided informed consent for publication of the images in figures.
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, H., Cui, C., Liu, H. et al. Preliminary Study on Retrograde Recanalization of Radial Artery Occlusion Through Distal Radial Artery Access: a Single-Center Experience. Cardiovasc Drugs Ther (2023). https://doi.org/10.1007/s10557-023-07490-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-023-07490-9