Abstract
Aims
In-stent chronic total occlusion (IS-CTO) represents a unique challenge for percutaneous coronary intervention. Whether the optimal treatment for IS-CTO is angioplasty with paclitaxel-coated balloons (PCBs) or repeat stenting with drug-eluting stents (DESs) is unclear. We aimed to evaluate the long-term clinical outcome of PCB angioplasty and DES repeat stenting for DES IS-CTO.
Methods
We retrospectively included patients with DES IS-CTO who underwent successful PCB angioplasty or DES repeat stenting from January 2016 to December 2019. The primary endpoints were major adverse cardiac events (MACEs), including cardiac death, myocardial infarction, and target lesion revascularization (TLR). Cox proportional hazards model was performed to compare the risk of MACEs between PCB angioplasty and DES repeat stenting, and to further explore the prognostic factors of patients with DES IS-CTO.
Results
A total of 214 patients with DES IS-CTO were enrolled: 78 patients (36.4%) treated with PCB and 136 patients (63.6%) treated with DES respectively. The median follow-up was 1160 days, and MACEs were observed in 28.2% of patients with PCB angioplasty versus 26.5% of patients with DES repeat stenting (P = 0.784), mainly driven by TLR (21.8% vs. 19.9%, P = 0.735). There was no significant difference in the risk of MACEs between the PCB group and the DES group (hazard ratio [HR] 1.25, 95% confidence interval [CI] 0.64–2.46, P = 0.512). Multivariate Cox analysis revealed that chronic kidney disease and ≥ 3 stent layers in the lesion were independent predictors of MACEs, while switching to another antiproliferative drug was an independent protective factor (all P < 0.05).
Conclusions
PCB angioplasty was an effective alternative treatment strategy for DES IS-CTO, which had similar long-term outcomes to DES repeat stenting in contemporary practice, but both were accompanied by a high rate of long-term MACEs. Improving the poor prognosis of patients with DES IS-CTO remains a challenge.
Similar content being viewed by others
Introduction
The application of drug-eluting stents (DESs) is predominant in routine coronary intervention. Antiproliferative drugs bound to the surface of the DES can inhibit active neointimal hyperplasia after stent implantation. The new generation of DESs are especially effective and can further reduce the risk of restenosis and need for target lesion revascularization (TLR) [1, 2]. However, within 5 years of stenting with DESs, approximately 7 to 10% of patients undergo re-revascularization of the target lesion due to in-stent restenosis (ISR) [3,4,5]. In the field of percutaneous coronary intervention (PCI), ISR and chronic total occlusion (CTO) are two major challenges. In-stent chronic total occlusion (IS-CTO) is a kind of coronary artery disease that occurs after stenting and has characteristics of both ISR and CTO. The number of IS-CTO cases accounts for approximately 10 to 25% of all PCI performed for CTO [6,7,8]. Although the incidence of IS-CTO is not extremely high, due to the popularity of percutaneous coronary stenting, especially in the contemporary era, patients who have received DES implantation constitute a very large base, and the public health burden caused by DES IS-CTO cannot be underestimated.
Currently, the two main treatments for ISR are angioplasty with paclitaxel-coated balloons (PCBs) and repeat stenting with DESs [9,10,11,12]. However, current data are insufficient for comparisons of effectiveness between the two strategies. In this study, we compared the long-term clinical outcomes of patients who underwent angioplasty with PCB or repeat stenting with DES in the treatment of DES IS-CTO and identified the clinical predictors of MACEs, hoping to provide medical evidence for optimizing the treatment of DES IS-CTO in clinical practice.
Methods
Study Population
From January 2016 to December 2019, we retrospectively enrolled patients who underwent successful PCI with PCB or DES for DES IS-CTO in Beijing Anzhen Hospital. Patients treated with both PCBs and DESs at the lesion site and patients lost to follow-up were excluded in the final analysis. For patients with multiple interventions or multivessel disease, only the first successful PCI for DES IS-CTO was recorded. In each procedure, lesions were fully predilated with noncompliant balloons, scoring balloons, or cutting balloons. The choices of devices and implants were decided by the operators or interventional cardiologist teams. According to the different intervention treatments used at the occlusion site, the patients were divided into two groups: the PCB angioplasty group and the DES repeat stenting group. After patients were discharged from the hospital, professionally trained and experienced investigators obtained patients’ clinical endpoints through review of medical records or telephone interviews. Variable data were assessed independently by at least two cardiologists, and controversial data were submitted to a panel of independent experts (three certified cardiologists) for adjudication. Clinical, procedural, and outcome data were recorded by independent investigators in a dedicated database. The study protocol was performed according to the principles of the Declaration of Helsinki and approved by the hospital ethics committee.
Definitions and Endpoints
CTO was defined as a coronary obstruction with a thrombolysis in myocardial infarction (TIMI) flow grade 0 for at least 3 months [13]. The occlusion duration was estimated by typical symptoms, angiogram, history of myocardial infarction in the target vessel territory, and new ischemic or infarct changes on electrocardiogram after the previous stent implantation. The CTO was considered in-stent if the occlusion was located within a previously deployed stent or within the 5-mm margins proximal or distal to the stent [14]. Procedural success was defined as successful CTO revascularization, achievement of < 30% residual diameter stenosis within the target lesions, and restoration of TIMI grade 3 flow, with no in-hospital serious adverse events, including death, myocardial infarction (MI), urgent target vessel revascularization with PCI or bypass surgery, cardiac tamponade requiring intervention or surgery, and stroke. The baseline demographic, angiographic, and procedure data were obtained through the Hospital Information System. The definition of high bleeding risk was based on the standards developed by the Academic Research Consortium for High Bleeding Risk [15]. The J-CTO score was calculated from 5 dimensions of blunt stump, calcification, bending > 45°, CTO lesion length ≥ 20 mm, and reattempt [16]. The PROGRESS CTO score was calculated from the 4 dimensions of proximal cap ambiguity, absence of interventional collaterals, moderate or severe tortuosity, and circumflex CTO [17]. The J-CTO score and PROGRESS CTO score were used to quantify the complexity of CTO lesions. The collateral circulation of CTO was graded with Rentrop classification [18]. The primary endpoints were major adverse cardiac events (MACEs), defined as a composite of cardiac death, MI, and TLR on follow-up [19]. Cardiac death was defined as any death of cardiac cause, unwitnessed death, or death without another known cause [20]. MI was defined according to the fourth universal definition of MI [21]. TLR was defined as any repeat percutaneous intervention or target vessel bypass surgery performed for restenosis or other complications of CTO target lesion [20].
Statistical Analysis
Continuous variables are presented as the mean ± standard deviation (SD) or the median with first quartile (Q1) and third quartile (Q3). Student’s t test or the Wilcoxon rank-sum test were used to compare differences in continuous variables between groups. Categorical variables are presented as numerical values and percentages, and data were compared using the chi-square or Fisher’s exact test. To determine whether the application of PCB angioplasty or DES repeat stenting was associated with adverse long-term outcomes, survival curves were plotted to estimate the cumulative incidence of clinical events using the Kaplan–Meier method, and intergroup comparisons were performed using the log-rank test. The propensity score–based inverse probability of treatment weighting (IPTW) method was also performed to reduce possible selection bias and then evaluate the association between different intervention treatments and clinical outcome. Covariate include male, age, current smoker, diabetes, chronic kidney disease (CKD), high bleeding risk, calcification, CTO lesion length ≥ 20 mm, moderate or severe tortuosity, ostial lesion, proximal cap side-branch, diseased distal landing zone, time since last stents implantation in target lesion, and number of stent layers in lesions [11, 12, 15, 22,23,24]. After IPTW, weighted standardized mean differences of each covariate with values < 0.10 indicated a reasonable balance. The hazard ratios (HRs) of MACE were calculated using the Cox proportional hazards model. Univariable models were constructed for the treatments and other variables, including those with P values < 0.10 between participants with and without MACEs and between participants who underwent different treatments, other variables that incorporated into the propensity score model were also included. Further, a multivariable Cox model was constructed to adjust for variables with a P value < 0.10 in the univariable model. A P value < 0.05 on the two-sided test was considered statistically significant. All statistical analyses were performed using SPSS software, Version 22.0 (IBM Corporation, Armonk, NY, USA) and R statistical package version 4.0.3 (R Project for Statistical Computing, Vienna, Austria).
Results
Patient Characteristics
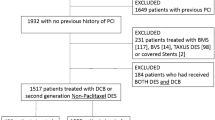
A total of 214 eligible patients were enrolled in our study, and the study flow chart is presented in Fig. 1. Seventy-eight patients (36.4%) were treated with PCB angioplasty, and 136 patients (63.6%) were treated with DES repeat stenting. The baseline demographic and clinical characteristics of the PCB angioplasty group and the DES repeat stenting group are presented in Table 1. A total of 83.6% of the patients were male, with a mean age of 59.1 ± 8.9 years. Baseline cardiovascular risk factors did not differ significantly between participants who underwent different treatments except for a higher ejection fraction in patients who underwent PCB angioplasty (62 (58–66)% vs. 59 (53–65)%, P = 0.016).
Angiographic Characteristics
The angiographic features of the two groups are shown in Table 2. The distribution of CTO target vessels was observed to be different between the two groups. PCB angioplasty was more frequently performed in the left anterior descending artery, while DES repeat stenting was more often performed in the right coronary artery IS-CTO. The J-CTO score (2 (1, 3) vs. 2 (1, 3), P = 0.855) and PROGRESS CTO score (1 (0, 1) vs. 1 (0, 2), P = 0.336) representing CTO complexity in the PCB group were comparable to those in the DES group. In our study, the time since last stent implantation in target lesion was 72 (interquartile range 37 to 109) months, and sirolimus-eluting stents were implanted in 150 (70.1%) patients during the previous PCI.
Procedural Characteristics
In terms of procedure characteristics, although the final implants were different, other data between the two groups were basically balanced, as shown in Table 3. In our study, antegrade wire escalation was the main initial strategy. In the final successful strategy, although the proportion of antegrade wire escalation decreased, retrograde wire escalation or antegrade dissection re-entry accounted only for a small part. Furthermore, no significant differences were observed between the PCB group and the DES group in procedure time, fluoroscopy time, or contrast volume, which reflected the difficulty of the operation. When the effects of different antiproliferative drugs were considered, a significant difference was observed between the two groups in switching to another antiproliferative drug. The majority of the PCB group adopted a switch strategy, while the proportion was almost double that of the DES group (94.9% vs. 50.0%, P < 0.001).
The number of patients who underwent successful IS-CTO PCI during the study period and the trend in the use of PCB angioplasty are presented in Fig. 2. Over time, the application of PCB angioplasty was observed to increase gradually, from 27.6% in the early period to 40.0% recently but no statistically significant difference (Pfor trend = 0.172).
Furthermore, when we grouped the patients according to the number of previous stent layers at the lesions, an increase in the proportion of PCB angioplasty was observed with the increase in the number of stent layers (Pfor trend = 0.007), as shown in Fig. 3.
Clinical Outcomes
Over the median follow-up of 1160 (interquartile range 937 to 1536) days and a minimum follow-up time of 383 days, 58 (27.1%) patients had MACEs, mainly driven by TLR (20.6%) (Table 4). There was no significant difference in the incidence of MACEs and their components between the PCB angioplasty group and the DES repeat stenting group during the follow-up (P = 0.784). Patients with MACEs were more likely to have CKD (P = 0.009), more stent layers in lesions (P = 0.001), less time since last stent implantation in target lesion (P = 0.048), and a lower proportion of different antiproliferative drugs (P = 0.006) (Online Resource 1).
Kaplan–Meier curves are shown in Fig. 4. The log-rank test for equality of survivor function showed no significant difference between the PCB angioplasty group and DES repeat stenting group in MACEs (P = 0.711) or in cardiac death (P = 0.500), MI (P = 0.603), and TLR (P = 0.700). In the Cox proportional hazards model, different treatments were not associated with the risk of MACEs (HR 1.11, 95% CI 0.65–1.88, P = 0.711), even after multifactorial adjustment (HR 1.25, 95% CI 0.64–2.46, P = 0.512) (Table 5). Finally, after the adjustment of propensity score–based IPTW (Online Resource 2), there was no significant difference in clinical outcome among different treatment modalities (Online Resource 3). CKD (HR 2.82, 95% CI 1.37–5.83, P = 0.005) and ≥ 3 stent layers in lesions (HR 4.50, 95% CI 2.04–9.91, P < 0.001) were found to be related to a higher risk of MACEs. Patients treated with different antiproliferative drugs decreased the risk of MACEs by 55% (HR 0.45, 95% CI 0.24–0.85, P = 0.014), and the results remained significant for another limus-DES repeat stenting subgroup (HR 0.35, 95% CI 0.15–0.79, P = 0.012) (Online Resource 4).
Kaplan–Meier survival curves of incident major adverse cardiac events (A), cardiac death (B), myocardial infarction (C), and target lesion revascularization (D) for patients with paclitaxel-coated balloon angioplasty or drug-eluting stent implantation. DES, drug-eluting stent; MACE, major adverse cardiac event; MI, myocardial infarction; PCB, paclitaxel-coated balloon; TLR, target lesion revascularization
Discussion
The main findings of our study are as follows:
-
1)
With the increase in the number of previous stent layers in DES IS-CTO lesions, the proportion of PCB gradually increased.
-
2)
After successful revascularization with PCB or DES in patients with DES IS-CTO, MACEs occurred in approximately one-fourth of patients during the median follow-up of 3 years and were mainly driven by TLR.
-
3)
No significant difference in long-term clinical outcomes was observed between patients who underwent PCB angioplasty and those who underwent DES repeat stenting in the treatment of DES IS-CTO.
-
4)
CKD and ≥ 3 stent layers in the lesion were independent predictors of adverse prognosis, while switching to another antiproliferative drug was an independent protective factor.
For a long time, ISR has been a problem for operators despite the evolution of stents [25]. In the era of DES, CTO occurring within stents has become a unique type of coronary artery disease. Unlike bare-metal stent (BMS) IS-CTO, the main cause of DES IS-CTO is acute thrombotic occlusion followed by neointimal hyperplasia-related restenosis, hypersensitivity, neointimal erosion, neoatherosclerotic rupture, and edge-related disease [26].
In our study, patients with DES IS-CTO were observed to have a high incidence of long-term adverse events. Previous studies have shown that regardless of the therapeutic modality, the clinical outcomes of DES-ISR were worse than those of BMS-ISR [27]. A study of 11,961 CTO PCI cases at 107 centers worldwide reported that interventions for IS-CTOs and de novo CTOs had similar rates of technical success, procedural success, and in-hospital adverse events, but poorer prognosis [28]. Other contemporary studies also confirmed that compared to de novo CTO, IS-CTO was associated with poorer long-term outcomes despite similar procedural success rates [29,30,31]. The objective of our study was the intersection of the two adverse lesions, DES-ISR, and IS-CTO. Especially in the era of widespread application of DES, DES IS-CTO has become a troublesome type of lesion that operators have to face. However, the poor prognosis, which was not parallel to the high success rate, was an unacceptable fact for operators. Vasodilation is severely impaired after IS-CTO PCI, which leads to hemodynamic changes and promotes the progression of thrombosis or atherosclerosis [32]. The phenomenon of multilayered stents at lesions was observed in nearly half of the cases in our study. Previous studies have found that multilayer stent implantation may be associated with an increased risk of abnormal vascular response and stent recoiling leading to underexpansion, which in turn leads to a worse long-term prognosis [30, 33].
In the published literature, few studies have specifically explored the long-term outcomes of PCB or DES treatment with IS-CTO. Basavarajaiah et al. [34] compared the long-term outcome of 403 IS-CTO patients treated with balloon angioplasty (BA), drug-coated balloon (DCB), or DES. During the 4-year median follow-up period, MACEs occurred in about half of the patients, of which the BA group had the worst outcome. Compared with the other two treatment modalities, the DCB group had a lower rate of revascularization, but the difference was not statistically significant. In our study, no significant difference in long-term clinical events was observed between PCB angioplasty group and DES repeat stenting group for DES IS-CTO. As the two most effective treatments for ISR, the question about PCB angioplasty and DES repeat stenting which one is better has always been the focus of academic attention. In the 2018 European Society of Cardiology/European Association for Cardiothoracic Surgery Guidelines on Myocardial Revascularization, both DESs and DCBs were recommended for the treatment of ISR, whether BMS-ISR or DES-ISR (Class I, Level of Evidence: A) [10]. A large meta-analysis of 10 randomized clinical trials showed that angioplasty with PCB was less effective than repeat stenting with DES in reducing TLR in the treatment of DES-ISR [11].
As an alternative implant, DCBs are coated with antiproliferative drugs based on a lipophilic matrix, such as paclitaxel, which homogeneously transfers the drug to the coronary artery wall during balloon dilatation. The obvious advantage of DCBs is that they do not require additional metal layers, and they prevent the risks associated with permanent implants and reduce the incidence of inflammation and thrombosis. However, the disadvantages of intervention without implantation are the reduction in acute gain and occurrence of acute recoil [12]. As the other choice of the two main treatment options, DES stenting seems to be the more common and widely accepted treatment for CTO. However, repeated stenting in IS-CTO may again trigger previous stent restenosis factors, such as local abnormal inflammation, adverse reactions to the stent polymer, resistance to antiplatelet agents, stent malapposition or underexpansion, and even immune diseases [29, 35]. Therefore, in the intervention of DES IS-CTO, especially in the treatment of complex lesions with multiple stent layers, there is a dilemma that every operator must face. Although the placement of PCBs can prevent the need for additional stent placement, it does not bring satisfactory long-term outcomes. Similarly, although DES can bring good acute and midterm outcomes, it constitutes a part of the vicious circle of ISR in the long run [36].
A phenomenon of routine intervention for DES IS-CTO has been observed: as the number of stent layers increased in the lesions, operators preferred PCB angioplasty as an emerging alternative option to additional stent implantation. The current theory holds that stent overlap increases the risk of restenosis and recurrent ISR, and additional stenting at ISR lesion can further impair muscle reactivity and endothelial function [37]. In a number of large multicenter registries published in recent years, stenting has been found to be less used in the interventions of IS-CTOs than in de novo CTOs [28]. This may represent the operator’s concern that repeated stenting may be associated with poor prognosis. Our study confirmed the operator’s concern that the long-term outcomes of IS-CTO with multilayer metal stents were worse than those with single-layer metal stents. Yabushita et al. [33] presented data from the New Tokyo Registry that evaluated the clinical outcome of DCBs for the treatment of ISR based on the number of previous metallic layers. MACEs and TLR at 1 year after DCB treatment were significantly higher in patients with ≥ 3 stent layers than in those in the 1 and 2 stent layer groups, and ≥ 3 metallic layers were independent predictors of MACEs. For multimetal layer ISR, previous stent underexpansion or stent fracture may be more difficult to correct, which may be a possible reason for the poor prognosis of multimetal layer ISR. Since multilayer metal stents are associated with poor prognosis, operators should avoid placing stents with more than 2 layers. For patients with symptomatic recurrent restenosis, other alternative treatments may be considered, such as DCB, brachytherapy, or bypass grafting [38].
In this study, CKD was independently associated with poor prognosis, which was expected, as a higher incidence of MACEs was also observed in a subset of patients with CKD complicated with ISR in previous studies [39]. In the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches-Chronic Kidney Disease trial, revascularization did not reduce the risk of death and nonfatal MI in patients with stable coronary heart disease and advanced CKD [40]. Since each intervention causes additional damage to renal function, current guidelines recommend that the contrast load greater than 4 times estimated glomerular filtration rate should be used as an indication for terminating CTO-PCI attempts [41], leaving very limited room for physicians to operate in patients with CKD. Therefore, operators should carefully weigh the risks and benefits and be cautious when considering interventions for such patients. It must be emphasized that the effective treatment cannot be achieved without comprehensive and integrated management of individuals. Therefore, for patients with DES IS-CTO complicated with CKD, in addition to the necessary interventional therapy and antiplatelet therapy, active control of clinical complications and guideline-directed medical therapy may be helpful for improving prognosis [38].
We observed that switching to another antiproliferative drug was associated with better clinical outcomes. In our study, almost all PCB angioplasties adopted a switching strategy, which may be because fewer patients were previously implanted with paclitaxel-eluting stents in our study. Therefore, we analyzed limus-DES as a subgroup and confirmed that the switching to another antiproliferative drug was still significantly associated with a better prognosis in the DES repeat stenting group. In the Restenosis Intra-Stent: Balloon Angioplasty Versus Drug-Eluting Stent trial, a prospective multicenter study evaluated the angiographic and clinical outcomes of DES with different drug or alternative interventional modalities in the treatment of DES-ISR [42]. The main finding was that treatment of DES-ISR with different DESs (switch strategy) was associated with better angiographic and clinical long-term results. When compared in the cohort that underwent repeat stenting, the angiographic results of different DES approaches were superior to those of the same DES approach, which also showed a better trend in clinical results. The theoretical basis of DESs with different antiproliferative drugs in the treatment of DES-ISR is based on the different mechanisms of action of their active pharmacologic agents. Tissues respond differently to different DESs, so the factors involved in previous stent failure may be corrected by switching to DESs with different antiproliferative drugs [43]. Although there are many different mechanisms involved in ISR, when the previous DES fails, operators should be cautious in developing new intervention strategies, in which case switching to another antiproliferative drug may be an attractive treatment strategy.
The classification of ISR has been updated in recent years. In the past, Mehran et al. [44] developed a classification of ISR based on BMS according to the characteristics of angiography. With the promotion of DES and an in-depth understanding of the restenosis mechanism, Waksman et al. [45] based on the mechanism of restenosis proposed a new classification for DES-ISR. Sekiguchi et al. [46] proposed four occlusion patterns of IS-CTO and found differences in the technical success rate, guidewire crossing times, and crossing strategy among different patterns. In the DES era, both the correct classification and individualized treatment of DES IS-CTO based on the mechanism and occlusion patterns of restenosis are crucial to improve clinical efficacy. It is challenging to infer the mechanism of stent failure by angiography alone, and intracoronary imaging can effectively identify the mechanical and biological mechanisms of ISR [22]. Intravascular ultrasound (IVUS)-guided IS-CTO PCI can assist in the selection of appropriate stents, optimize the final result, and provide acceptable long-term clinical outcomes [8]. In addition, optical coherence tomography (OCT) has been recommended by the European Association of Percutaneous Cardiovascular Interventions, as the preferred imaging technique for studying ISR [47]. OCT can provide higher resolution images for the evaluation of morphological features, thus helping to correct factors related to past failures and optimize the intervention [48]. Although previous stents can serve as a roadmap for intervention, tracking through the stented segment theoretically reduces the risk of dissection or injury during the procedure, further improving the procedure success rate [30]. In routine recanalization practice, however, conditions such as stent underexpansion or stent rupture often make wiring more difficult, and the complexity of the IS-CTO means presence of subintimal or extra-stent wire passage, difficulty in device delivery, and even crushing the occluded stent, which increases the risk of adverse events [28, 49, 50]. Recently, the IS-CTO score system was established to predict the technical success of IS-CTO PCI via antegrade approach, which reflects the academic circle’s attention to this special type of coronary artery disease [50]. We are pleased to see that with the improvement of technology, the innovation of CTO PCI devices, and the accumulation of experience, the success rate of contemporary IS-CTO PCI is increasing [28]. Of course, the best way to solve DES IS-CTO is to prevent it. Once the DES IS-CTO happens, trying to identify the cause behind it, correct the undesirable factors, and avoid repeating the same mistakes is the direction we should strive for.
Limitations
This study has several limitations. First, this was a single-center, retrospective study of a small cohort with inevitable shortcomings. Second, because the choices of implants were determined by the operators or interventional cardiologist teams, there was selection bias in this real-world study. Although we performed propensity score to minimize possible bias, larger multicenter randomized controlled trials are still needed to clarify the clinical outcome of DES IS-CTO. Third, the proportion of intracoronary imaging used in our study was much lower than in other large IS-CTO studies conducted at the same period [28], so it was not possible to carefully evaluate the pathological features and potential mechanism of DES IS-CTO, and the lack of an IVUS- or OCT-optimized intervention may be associated with poor clinical outcomes; therefore, the results of this study should be interpreted carefully. Fourth, this study only recorded the medication of patients at discharge, but the medication of patients after discharge, including dose, frequency, and duration, has not been well evaluated. Therefore, it was not clear whether drug factors affect the long-term prognosis of patients. Last, this study excluded patients with unknown data on previous interventional procedures, so the conclusions of this study may not be extended to all patients with DES IS-CTO.
Conclusions
PCB angioplasty for the treatment of DES IS-CTO is effective and has similar long-term outcomes to DES repeat stenting in contemporary practice. Successful DES IS-CTO interventions were accompanied with a higher rate of long-term adverse events, especially for patients with CKD and multilayered stents. Switching to another antiproliferative drug may provide better long-term clinical outcomes, especially for patients with limus-DES repeat stenting.
Data Availability
The raw data supporting the conclusion of this article will be provided by the communication author under reasonable requirements.
References
Bangalore S, Kumar S, Fusaro M, et al. Short- and long-term outcomes with drug-eluting and bare-metal coronary stents: a mixed-treatment comparison analysis of 117 762 patient-years of follow-up from randomized trials. Circulation. 2012;125(23):2873–91.
Stefanini GG, Holmes DR Jr. Drug-eluting coronary-artery stents. N Engl J Med. 2013;368(3):254–65.
Zocca P, Kok MM, Tandjung K, et al. 5-year outcome following randomized treatment of all-comers with zotarolimus-eluting resolute integrity and everolimus-eluting PROMUS element coronary stents: final report of the DUTCH PEERS (TWENTE II) Trial. JACC Cardiovasc Interv. 2018;11(5):462–9.
Vlachojannis GJ, Smits PC, Hofma SH, et al. Biodegradable polymer biolimus-eluting stents versus durable polymer everolimus-eluting stents in patients with coronary artery disease: final 5-year report from the COMPARE II Trial (abluminal biodegradable polymer biolimus-eluting stent versus durable polymer everolimus-eluting stent). JACC Cardiovasc Interv. 2017;10(12):1215–21.
Iqbal J, Serruys PW, Silber S, et al. Comparison of zotarolimus- and everolimus-eluting coronary stents: final 5-year report of the RESOLUTE all-comers trial. Circ Cardiovasc Interv. 2015;8(6):e002230.
Abbas AE, Brewington SD, Dixon SR, et al. Success, safety, and mechanisms of failure of percutaneous coronary intervention for occlusive non-drug-eluting in-stent restenosis versus native artery total occlusion. Am J Cardiol. 2005;95(12):1462–6.
Vemmou E, Alaswad K, Karmpaliotis D, et al. Outcomes of percutaneous coronary intervention for in-stent chronic total occlusions: insights from the PROGRESS-CTO Registry. JACC Cardiovasc Interv. 2020;13(16):1969–71.
Yoon YH, Lee PH, Lee SW, et al. Clinical outcomes after percutaneous coronary intervention for in-stent chronic total occlusion. EuroIntervention. 2020;16(6):e472–9.
Giacoppo D, Gargiulo G, Aruta P, et al. Treatment strategies for coronary in-stent restenosis: systematic review and hierarchical Bayesian network meta-analysis of 24 randomised trials and 4880 patients. BMJ. 2015;351:h5392.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Giacoppo D, Alfonso F, Xu B, et al. Paclitaxel-coated balloon angioplasty vs. drug-eluting stenting for the treatment of coronary in-stent restenosis: a comprehensive, collaborative, individual patient data meta-analysis of 10 randomized clinical trials (DAEDALUS study). Eur Heart J. 2020;41(38):3715–28.
Lansky A, Grubman D, Scheller B. Paclitaxel-coated balloons: a safe alternative to drug-eluting stents for coronary in-stent restenosis. Eur Heart J. 2020;41(38):3729–31.
Christopoulos G, Karmpaliotis D, Alaswad K, et al. The efficacy of “hybrid” percutaneous coronary intervention in chronic total occlusions caused by in-stent restenosis: insights from a US multicenter registry. Catheter Cardiovasc Interv. 2014;84(4):646–51.
de la Torre Hernandez JM, Rumoroso JR, Subinas A, et al. Percutaneous intervention in chronic total coronary occlusions caused by in-stent restenosis: procedural results and long-term clinical outcomes in the TORO (Spanish registry of chronic TOtal occlusion secondary to an occlusive in-stent RestenOsis) multicentre registry. EuroIntervention. 2017;13(2):e219–26.
Urban P, Mehran R, Colleran R, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the Academic Research Consortium for High Bleeding Risk. Eur Heart J. 2019;40(31):2632–53.
Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–21.
Christopoulos G, Kandzari DE, Yeh RW, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: the PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) Score. JACC Cardiovasc Interv. 2016;9(1):1–9.
Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985;5(3):587–92.
Garcia-Garcia HM, McFadden EP, Farb A, et al. Standardized end point definitions for coronary intervention trials: the Academic Research Consortium-2 Consensus Document. Circulation. 2018;137(24):2635–50.
Ybarra LF, Rinfret S, Brilakis ES, et al. Definitions and clinical trial design principles for coronary artery chronic total occlusion therapies: CTO-ARC Consensus Recommendations. Circulation. 2021;143(5):479–500.
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618–51.
Ullrich H, Olschewski M, Munzel T, Gori T. Coronary in-stent restenosis: predictors and treatment. Dtsch Arztebl Int. 2021;118(38):637–44.
Jeger RV, Eccleshall S, Wan Ahmad WA, et al. Drug-coated balloons for coronary artery disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020;13(12):1391–402.
Lee JM, Rhee TM, Hahn JY, et al. Comparison of outcomes after treatment of in-stent restenosis using newer generation drug-eluting stents versus drug-eluting balloon: Patient-level pooled analysis of Korean Multicenter in-Stent Restenosis Registry. Int J Cardiol. 2017;230:181–90.
Kufner S, Joner M, Thannheimer A, et al. Ten-year clinical outcomes from a trial of three limus-eluting stents with different polymer coatings in patients with coronary artery disease. Circulation. 2019;139(3):325–33.
Mori H, Lutter C, Yahagi K, et al. Pathology of chronic total occlusion in bare-metal versus drug-eluting stents: implications for revascularization. JACC Cardiovasc Interv. 2017;10(4):367–78.
Byrne RA, Cassese S, Windisch T, et al. Differential relative efficacy between drug-eluting stents in patients with bare metal and drug-eluting stent restenosis; evidence in support of drug resistance: insights from the ISAR-DESIRE and ISAR-DESIRE 2 trials. EuroIntervention. 2013;9(7):797–802.
Vemmou E, Quadros AS, Dens JA, et al. In-stent CTO percutaneous coronary intervention: individual patient data pooled analysis of 4 multicenter registries. JACC Cardiovasc Interv. 2021;14(12):1308–19.
Azzalini L, Dautov R, Ojeda S, et al. Procedural and long-term outcomes of percutaneous coronary intervention for in-stent chronic total occlusion. JACC Cardiovasc Interv. 2017;10(9):892–902.
Lee SH, Cho JY, Kim JS, et al. A comparison of procedural success rate and long-term clinical outcomes between in-stent restenosis chronic total occlusion and de novo chronic total occlusion using multicenter registry data. Clin Res Cardiol. 2020;109(5):628–37.
Mir T, Ullah W, Sattar Y, et al. Outcomes of percutaneous intervention in in-stent versus de-novo chronic total occlusion: a meta-analysis. Expert Rev Cardiovasc Ther. 2020;18(11):827–33.
Galassi AR, Tomasello SD, Crea F, et al. Transient impairment of vasomotion function after successful chronic total occlusion recanalization. J Am Coll Cardiol. 2012;59(8):711–8.
Yabushita H, Kawamoto H, Fujino Y, et al. Clinical outcomes of drug-eluting balloon for in-stent restenosis based on the number of metallic layers. Circ Cardiovasc Interv. 2018;11(8):e005935.
Basavarajaiah S, Mitomo S, Nakamura S, et al. Long-term outcome following percutaneous intervention of intra-stent coronary occlusion and evaluating the different treatment modalities. Int J Cardiol Heart Vasc. 2021;34:100803.
Gong ML, Mao Y, Liu JH. Long-term outcomes of percutaneous coronary intervention for in-stent chronic total occlusion. Chin Med J (Engl). 2020;134(3):302–8.
Alfonso F, Cuesta J. The therapeutic dilemma of recurrent in-stent restenosis. Circ Cardiovasc Interv. 2018;11(8):e007109.
Singh AD, Singal AK, Mian A, et al. Recurrent drug-eluting stent in-stent restenosis: a state-of-the-art review of pathophysiology, diagnosis, and management. Cardiovasc Revasc Med. 2020;21(9):1157–63.
Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(3):e18–114.
Jonas M, Kagan M, Sella G, Haberman D, Chernin G. Cardiovascular outcomes following percutaneous coronary intervention with drug-eluting balloons in chronic kidney disease: a retrospective analysis. BMC Nephrol. 2020;21(1):445.
Bangalore S, Maron DJ, O’Brien SM, et al. Management of Coronary Disease in Patients with Advanced Kidney Disease. N Engl J Med. 2020;382(17):1608–18.
Galassi AR, Werner GS, Boukhris M, et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention. 2019;15(2):198–208.
Alfonso F, Perez-Vizcayno MJ, Dutary J, et al. Implantation of a drug-eluting stent with a different drug (switch strategy) in patients with drug-eluting stent restenosis. Results from a prospective multicenter study (RIBS III [Restenosis Intra-Stent: Balloon Angioplasty Versus Drug-Eluting Stent]). JACC Cardiovasc Interv. 2012;5(7):728–37.
Yabe T, Toda M, Nakanishi R, et al. Same or different drug-eluting stent re-implantation for drug-eluting stent restenosis: an assessment including second-generation drug-eluting stents. J Interv Cardiol. 2016;29(3):311–8.
Mehran R, Dangas G, Abizaid AS, et al. Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation. 1999;100(18):1872–8.
Shlofmitz E, Iantorno M, Waksman R. Restenosis of drug-eluting stents: a new classification system based on disease mechanism to guide treatment and state-of-the-art review. Circ Cardiovasc Interv. 2019;12(8):e007023.
Sekiguchi M, Muramatsu T, Kishi K, et al. Occlusion patterns, strategies and procedural outcomes of percutaneous coronary intervention for in-stent chronic total occlusion. EuroIntervention. 2021;17(8):e631–8.
Raber L, Mintz GS, Koskinas KC, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2018;39(35):3281–300.
Yin D, Mintz GS, Song L, et al. In-stent restenosis characteristics and repeat stenting underexpansion: insights from optical coherence tomography. EuroIntervention. 2020;16(4):e335–43.
Gao K, Li BL, Zhang M, et al. Long-term outcomes of percutaneous coronary intervention for patients with in-stent chronic total occlusion versus de novo chronic total occlusion. Angiology. 2021;72(8):740–8.
Gong M, Peng H, Wu Z, et al. Angiographic scoring system for predicting successful percutaneous coronary intervention of in-stent chronic total occlusion. J Cardiovasc Transl Res. 2021;14(4):598–609.
Funding
The study was supported by the National Natural Science Foundation of China (81970291 and 82170344).
Author information
Authors and Affiliations
Contributions
JL and SW conceived the concept of the study and supervision. YZ contributed to the design of the research and wrote the original draft. ZW and TL participated in data analysis and results interpretation. All authors were involved in data collection and analysis, and edited and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was reviewed and approved by Ethics Committee of Beijing Anzhen Hospital. The study was conducted according to the Declaration of Helsinki in its most current form. Approval was granted by Ethics Committee of Beijing Anzhen Hospital (2021–04-15/No.2021035X).
Consent to Participate
Not applicable.
Consent to Publish
Not applicable.
Competing Interests
The authors no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

10557_2022_7363_Fig5_ESM.png
Supplementary file2. Online Resource 2. The SMD of characteristic among IPTW unweighted and weighted sample. CKD: chronic kidney disease; CTO: chronic total occlusion; IPTW: inverse probability of treatment weighting; SMD: standardized mean differences (PNG 133 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Y., Wu, Z., Wang, S. et al. Clinical Outcome of Paclitaxel-Coated Balloon Angioplasty Versus Drug-Eluting Stent Implantation for the Treatment of Coronary Drug-Eluting Stent In-Stent Chronic Total Occlusion. Cardiovasc Drugs Ther 37, 1155–1166 (2023). https://doi.org/10.1007/s10557-022-07363-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-022-07363-7