Abstract
Purpose
This systematic review was performed to summarize published experience using low density lipoprotein particle number (LDL-P) to monitor the efficacy of lipid-lowering pharmacotherapies.
Methods
Studies were identified from a literature search of MEDLINE (January 1, 2000 – June 30, 2012); and abstract searches of select conferences. All accepted studies reported mean (or median) nuclear magnetic resonance (NMR)-based LDL-P values for at least 10 subjects receiving lipid lowering pharmacotherapy.
Results
Searches revealed 36 studies (with 61 treatment arms) in which LDL-P measurements were reported pre- and post-treatment. Most studies also reported changes in low-density lipoprotein cholesterol (LDL-C), but fewer studies reported changes in apolipoprotein B (apoB)(n = 20) and non-HDL-C (n = 28). Treatments included statins (22 arms/15 studies), fibrates (7 arms/7studies), niacin (7 arms/6 studies), bile acid sequestrants (5 arms/2 studies), an anti-apoB oligonucleotide (2 arms/2 studies), combination therapies (8 arms/6 studies), anti-diabetics (5 arms/4 studies), and, other treatments (5 arms/2 studies). Lipid-lowering pharmacotherapy resulted in reductions in mean LDL-P in all but two studies. In several statin studies, the percent reductions in LDL-P were smaller than reductions in LDL-C, comparable changes were reported when LDL-P and apoB, were reported.
Conclusions
Study-level data from this systemic review establish that different lipid lowering agents can lead to discordance between LDL-P and LDL-C, therefore, basing LDL-lowering therapy only on the achievement of cholesterol goals may result in a treatment gap. Therefore, the use of LDL-P for monitoring lipid-lowering therapy, particularly for statins, can provide a more accurate assessment of residual cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association between low-density lipoprotein (LDL) particles and cardiovascular disease (CVD) is well established [1, 2]. Evidence from lipid lowering clinical trials demonstrates that LDL lowering therapy reduces cardiovascular events [3]. Currently, there are number of methods available commercially to measure LDL. LDL cholesterol (LDL-C) and non-high-density lipoprotein cholesterol (non-HDL-C) rely on the cholesterol content of the lipoprotein to measure the efficacy of LDL-lowering therapy whereas LDL particle (LDL-P) number and apolipoprotein B (apoB) levels are used to measure the actual quantity of LDL [3].
LDL particles contain a core of lipid, predominantly cholesterol esters and a minor amount of triglycerides, surrounded by a shell of phospholipid on which the major surface protein is apoB [3]. LDL-C measures the amount of cholesterol packaged in the LDL particle and has served as the basis for the assessment and management of CVD risk for many years; however, a number of recent studies have shown that CVD risk may be better predicted by measuring the concentration of LDL-P [1, 2, 4, 5]. The cholesterol and triglyceride content of LDL particles vary widely among individuals and can change over time as a result of lifestyle changes, metabolic disease, and lipid-lowering therapy. It has been reported that statins, estrogen replacement therapy, and a low fat/high carbohydrate diet lower the LDL-C content in LDL particles more than they lower the LDL-P concentration, while fibrates, nicotinic acid, exercise and a low carbohydrate diet lower LDL-P concentration more than they lower LDL-C content [3]. Thus, reliance on LDL-C rather than LDL-P as a measure of CVD risk may result in suboptimal management of LDL-related risk in certain individuals.
In 2011, the National Lipid Association (NLA) held a consensus conference focused on the use of inflammatory markers and advanced lipoprotein testing to improve CVD risk assessment and management of lipid-lowering therapy. Their consensus statement concluded that measurement of LDL-P would be a “reasonable measure” to incorporate into treatment decisions for many patients at intermediate and high risk treated to LDL-C and non-HDL-C goals in order to evaluate the adequacy of LDL lowering therapy [6]. However, the panel noted: “additional research is needed to more clearly define settings in which a policy of treating to LDL-P goals might produce more favorable outcomes than the alternative of treating to LDL-C and non-HDL-C goals”.
To assess the utilization of LDL-P measurements for the management of lipid-lowering therapy, a systematic review of published studies was conducted which focused on study level comparisons of treatment-related changes in LDL-P versus other lipid parameters, including LDL-C, non-HDL-C, and apoB. We report here study-level correlations between treatment-related changes in lipid and lipoprotein parameters and CVD progression.
Materials and Methods
Literature Search and Selection
An electronic search of PubMed was performed using the following search strategy, where “MeSH” indicates Medical Subject Headings:
-
1.
Lipoproteins, LDL [MeSH] OR low-density lipoprotein particle OR LDL OR particle test OR LDL-C OR LDL-P
-
2.
Magnetic Resonance Spectroscopy [MeSH] OR NMR OR nuclear magnetic resonance
-
3.
#1 AND #2; Limits: English, Human, January 1, 2000 –July 30, 2012, NOT case reports, letters, editorials, reviews, new articles
Note that articles available as Epub ahead of print before the search cut-off date were considered eligible for inclusion; even if the eventual print publication date was after July 30, 2012. The electronic search was supplemented by manual searches of 2010 – 2012 abstracts for the annual meetings of the American College of Cardiology, and American Diabetes Association, National Lipid Association and American Heart Association (2010 and 2011 conferences only), (screened first by title and then by review of the complete abstract) and a limited manual search of reference lists from accepted studies and recent reviews.
Studies of any design (prospective or retrospective, randomized or non-randomized) were selected for review if they reported mean (or median) magnetic resonance-based LDL-P values for at least 10 patients prior to and after receiving lipid-lowering pharmacotherapy; studies reporting LDL-P changes only after nutritional supplements or lifestyle changes (exercise, diet, smoking cessation) were not included. Screening was performed by a single reviewer. Multiple publications of the same or overlapping series of patients were identified and grouped together as a “kinned” citation; the parent study was most often the most recent publication. Data from kinned studies were counted only once to avoid the double-counting of patients.
Extraction of Study-Level Variables
Data were extracted by two independent reviewers and discrepancies resolved by consensus conference. The following data elements were sought from each accepted study: study characteristics, including PMID number, first author, geographic location by country, publication year, study type [case series, cohort, Randomized Control Trial (RCT)], and lipid lowering treatment [generic drug name, dose, and treatment duration; population characteristics, including underlying condition(s) requiring lipid-lowering therapy, number of subjects enrolled, mean/median age, gender distribution, racial distribution, and number of subjects with CVD, present family history of CVD, diabetes, metabolic syndrome, smoking, hypertension (blood pressure >140/90 mm Hg or on medication), obesity (body mass index ≥ 35 kg/m3); and LDL-P, and if available, LDL-C, HDL-C, non-HDL-C, and apoB prior to and after lipid-lowering treatment; and if reported, CVD outcomes and changes in atherosclerotic plaque burden (carotid intima media thickness (CIMT), coronary artery calcium (CAC) score) and/or correlations of changes in LDL-P and CVD outcome and changes in atherosclerotic plaque burden.
On-treatment results for LDL-C, apoB and non–HDL-C are expressed in milligrams per deciliter and LDL-P in nanomoles per liter. In addition, each parameter is expressed in terms of population percentiles based on data from the Framingham Offspring Study [7].
Study, patient, and test-level data were summarized using general descriptive statistics (means, standard deviations, ranges, counts) and subgroup analyses were performed by type of lipid-lowering therapy.
Results
Search Yields
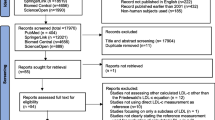
From the PubMed search, a total of 653 citations were screened and 320 full publications were retrieved for further review (Fig. 1). Manual searches of bibliographies and recent reviews yielded 51 additional studies, and manual searches of annual meeting abstracts yielded 4 additional studies (reported only as abstracts) for further review. From these, a total of 36 primary studies reported treatment-induced changes in mean (or median) NMR-derived LDL-P values following lipid-lowering pharmacotherapy. These studies served as the basis for this analysis. In addition to LDL-P, most accepted studies also reported changes in mean (or median) LDL-C (31 studies), non-HDL-C (28 studies) and/or apoB (20 studies). Baseline concentrations of LDL-P have been reported for the Medical Research Council/British Heart Foundation Heart Protection Study, one of the largest randomized control trials of statin therapy to date, however LDL-P was not measured following treatment so this study was not included.
Study and treatment characteristics are summarized in Table 1. Mean (or median) nuclear magnetic resonance (NMR)-based LDL-P values were reported pre- and post-treatments with statins (1876 subjects in 22 treatment arms), fibrates (788 subjects in 7 arms), niacin (580 subjects in 7 arms), bile acid sequestrants (139 subjects in 5 arms), combination therapies (1342 subjects in 8 treatment arms), anti-apoB oligonucleotide therapy (104 subjects in 2 treatment arms), anti-diabetic therapies (848 subjects in 5 treatment arms) and other treatments (717 subjects in 5 treatment arms). Most studies were short-term (median of 3 months per treatment arm), randomized controlled trials (28), and designed to demonstrate lipid lowering for primary prevention (27/36). Only four studies reported CVD outcomes.
Treatment-Induced Changes in Lipid Parameters
Results from 36 studies are summarized in Tables 2, 3, 4, 5, 6, 7, 8, and 9. Reductions in LDL-P were observed with all treatments except for two (one fibrate, one anti-diabetic). Similarly, LDL-C was reduced with all treatments except for the fibrates, anti-diabetic therapy and the cholesteryl ester transfer protein (CETP) inhibitor dalcetrapib. Of the marketed lipid-lowering monotherapies studied, statins produced the greatest reductions in LDL-P and LDL-C, followed by niacin, fibrates and bile acid sequestrants. In addition, the combination of statins with other agents yielded an even greater effect on LDL-P and LDL-C. The effects of each type of lipid-lowering or anti-diabetic therapy on LDL-P and LDL-C are discussed below in terms of average results across all studies within each drug class, not accounting for differences in the agent, dose, time period, size of the treatment group or characteristics of the population at baseline.
Statins
A total of 1,876 subjects were treated with statins for a mean of 4 months (range 1–12 months). Most subjects had hypercholesterolemia or mixed dyslipidemia with or without known CVD; two studies featured subjects with metabolic syndrome or diabetes. The types of statins studied included: atorvastatin (A) in 8 treatment arms [8–14], pravastatin (P) in 6 arms [13, 15–19], simvastatin (S) in 8 arms [9, 13, 20–22], rosuvastatin (R) in 3 arms [9, 12], and pitavastatin (Pit) in 1 arms [17]. The mean LDL-P and LDL-C concentrations at baseline were 1942 ± 380 nmol/L and 162 ± 32 mg/dL respectively (Table 2). The mean treatment-induced decrease in LDL-P across studies was 30 % producing an on-treatment level of 1346 ± 226 nmol/L which is equivalent to the 42nd percentile of the Framingham Offspring reference population. This was slightly less than the mean decrease in LDL-C (−34 %), which yielded an on-treatment level of 106 ± 27 mg/dL (29th percentile), and the mean decrease in non-HDL-C (−34 %, 35th percentile). The mean on-treatment apoB level was 103 ± 21 mg/dL (54th percentile) which represented a 27 % decrease from baseline. These results suggest that statins reduce LDL-C to a lower population percentile however, both LDL-P and apoB levels remained at elevated population percentiles signifying potentially higher residual cardiovascular (CV) risk.
Fibrates
Results from 7 studies of fibrate treatments involving 788 subjects with hypertriglyceridemia or known CVD are presented in Table 3. These included 4 studies with fenofibrate (F) [9, 21, 23, 24], 2 with bezafibrate (Bz) [25, 26] and one with gemfibrozil (G) [4]. Unlike statins, fibrates were found to increase LDL-C in most studies (mean +6 %) whereas LDL-P, non-HDL-C and apoB were reduced in most fibrate studies (mean decreases of 10 %, 14 % and 6 % respectively). The average population percentiles achieved for LDL-C, non-HDL-C and apoB were 44 %, 54 %, and 56 %, respectively. In contrast, the average on-treatment percentile achieved for LDL-P was 57 %. This highlights distinct differences in these biomarkers representing LDL-related risk for CVD.
Niacin
Niacin was evaluated in a total of 580 subjects enrolled across 6 studies (Table 4) [10, 27–33]. Baseline LDL-P and LDL-C levels were quite variable ranging from 1033 to 2561 nmol/L for LDL-P and 76 to 211 mg/dL for LDL-C. Small decreases (≤ 20 %) were observed in all LDL-related parameters with treatment. The mean population percentiles achieved on-treatment for LDL-P and LDL-C were 51 % and 53 % however in 2 studies, population percentiles for LDL-P of below 20 % were achieved [28, 31].
Bile acid Sequestrants
The bile acid Sequestrants colesevelam (Colv) and colestimide (Cole) were evaluated in 2 studies involving a total of 139 hypercholesterolemic subjects (Table 5) [34, 35]. Baseline LDL-P and LDL-C mean levels were significantly elevated (2206 ± 164 nmol/L and 178 ± 13 mg/dL, respectively). Both levels were decreased 9 % on treatment.
Anti-ApoB Oligonucleotides
Two studies reported results of treatment with the experimental injectable anti-apoB oligonucleotide mipomersin (Table 6) [36, 37]. One study was conducted in patients with familial hypercholesterolemia [36]; the other in statin-intolerant patients with high CVD risk [37]. Significant decreases in all LDL-related parameters were reported (mean −41 to −48 %). The average population percentiles achieved for LDL-C, non-HDL-C and apoB were 47 %, 45 %, and 53 %, respectively. In contrast, the average on-treatment percentile achieved for LDL-P was 28 %. Thus, LDL-P goals were closer to being achieved with treatment than LDL-C, non-HDL-C and apoB goals.
Combination Therapies
Therapies involving combinations of statins with one or more lipid lowering agent including niacin [20, 29], fenofibrate [9], ezetimibe [29] or prescription omega-3-fatty acid [11], pioglitazone [38], were evaluated in 1342 subjects across 6 studies (Table 7). On treatment, LDL-P and LDL-C were reduced 34 % and 35 %, to levels equivalent to the 27th and 13th percentiles of the reference population, respectively. Similar reductions in non-HDL-C (21 %) and apoB (35 %) were also observed. The most effective therapy was the combination of simvastatin with ezetimibe and niacin which decreased LDL-P and LDL-C by 48 % and 60 %, levels equivalent to the 10th and 2nd population percentiles, respectively [29].
Anti-diabetic agents
Results from 4 studies evaluating anti-diabetic therapies in subjects with metabolic syndrome or type 2 diabetes mellitus (T2D) are presented in Table 8. These included pioglitazone (3 treatment arms) [39–41], rosiglitazone (1 arm) [39] and metformin (1 arm) [42]. Overall, mean reductions in LDL-P and LDL-C were small (4–5 %).
Other lipid-lowering therapies
Two studies reported results from lipid-lowering therapies that could not be classified in the aforementioned treatment groups (Table 9). These included the Stop Atherosclerosis in Native Diabetics Study (SANDS) [43] and a study evaluating the CETP inhibitor dalcetrapib [44]. SANDS compared the effects of aggressive treatment to LDL-C and non-HDL-C targets vs. standard treatment. The aggressive treatment, consisting of statins, alone or in combination with other agents, decreased LDL-C and LDL-P to desired population percentile goals (<2 % and 7 %, respectively) whereas the standard treatment had little effect. In the dalcetrapib study in which subjects had LDL-C < 100 mg/dL but elevated LDL-P levels at baseline, treatment at the highest dose decreased LDL-P 10 % to a level equivalent to the 26th population percentile.
Medication, LDL-C and LDL-P Goals
Each study was evaluated to determine whether the following treatment goals recommended for high risk patients were met [45]: LDL-P ≤ 1000 nmol/L and LDL-C < 100 mg/dL. In the statin monotherapy studies, LDL-P goals were met in 4 % (1/22) of study arms and LDL-C goals met in 53 % (9/17) of study arms in which patients were above goal at initiation of treatment. In the niacin treatment group, LDL-P and LDL-C goals were met in 29 % (2/7) and 33 % (2/6) of study arms, respectively. In the statin combination therapy treatment group, LDL-P goals were met in 28 % (2/8) of study arms and LDL-C goals were met in 67 % (4/6) of treatment arms in which patients were above goal at initiation of treatment. In addition, LDL-C and LDL-P goals were met with aggressive, but not standard treatment, in SANDS. None of the other lipid-lowering therapies resulted in the attainment of LDL-P and LDL-C goals.
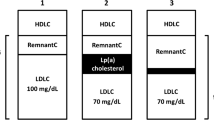
Furthermore, as illustrated in Fig. 2, these responses are expressed in terms of percentile of the population achieved for each lipid lowering therapy. Various treatment options (except niacin) reduced LDL-C to a lower population percentile versus LDL-P suggesting possible residual CV risk with elevated LDL-P levels.
Correlation of Lipid Parameters and CVD Progression
Three studies examined correlations between treatment-induced changes in lipid parameters and atherosclerosis progression [25, 43, 46] and one study examined correlations between changes in lipid parameters and new coronary events [4].
In the Pravastatin Limitation of Atherosclerosis in the Coronary Arteries (PLAC-I) Trial, 241 patients with angiographically defined coronary artery disease were randomized to treatment with 40 mg/day pravastatin or placebo [46]. Statin-treated subjects showed a 25 % decrease in LDL-P and 26 % decrease in LDL-C over 6 months and a significantly slower rate of lumen narrowing over 3 years compared to placebo controls (−0.018 vs. −0.053 mm/year, p < 0.01). Correlation of 6-month lipid levels and atherosclerosis progression showed that lumen narrowing was associated with higher on-study LDL-P (r = −0.13), independent of on-study LDL-C, HDL-C, and triglycerides.
In SANDS, 418 Native Americans with diabetes and no previous cardiovascular events were randomized to 1) aggressive statin treatment to targets of LDL-C ≤70 mg/dL, non-HDL-C ≤100 mg/dL, and systolic blood pressure (SBP) ≤115 mm Hg or 2) standard statin treatment to targets of LDL-C ≤100 mg/dL, non-HDL-C ≤130 mg/dL, and SBP ≤130 mm Hg [43]. CIMT was assessed as a measure of the severity of atherosclerosis. Most patients had been treated previously and had achieved standard targets at baseline (mean LDL-C of 103 and 102 mg/dL, mean non-HDL-C of 136 and 137 mg/dL, and mean SBP of 128 and 132 mm Hg for the aggressive and standard groups, respectively). After 36 months of treatment, the aggressive group had achieved significantly greater reductions in LDL-P (−30 % vs. −8 %), LDL-C (−31 % vs. +2 %), non-HDL-C (−26 % vs. +1 %), apoB (−26 % vs. −6 %) and a significant reduction in lumen narrowing (−0.020 vs. +0.038 mm) compared to the standard group. A comparison of changes in CIMT between the two groups, stratified by baseline lipid levels, showed no significant interactions between treatment and initial levels of LDL-P, LDL-C, non-HDL-C, HDL-C, triglycerides, or apoB indicating that the treatment effect did not differ by baseline levels of the measured lipid parameters. Further analysis found that changes in LDL-C and non-HDL-C were both independently correlated with CIMT regression, while changes in LDL-P and apoB showed borderline significance to CIMT regression at 36 months.
In the Veterans Affairs High-Density Lipoprotein Intervention Trial (VA-HIT), 1061 men with a diagnosis of established coronary heart disease (CHD) were randomized to 1200 mg/day gemfibrozil or placebo and treated for a median of 5.1 years. On-study lipid levels, obtained at the 7-month visit, showed significant increases in HDL-C (+6 % vs. 0 %) and HDL-P (+10 % vs. +6 %) and significant decreases in triglycerides (−30 % vs. +6 %), non-HDL-C (−5 % vs. +1 %), apoB (−6 % vs. −3 %), and LDL-P (−5 % vs. +7 %) for the gemfibrozil group compared to the placebo group [4]. Among those patients who had a coronary event, baseline and treatment levels of LDL-P were strong independent predictors of a new coronary event, while neither baseline nor on-study levels of LDL-C, HDL-C, or triglycerides were significant predictors of CHD risk.
Discussion
The objective of this analysis was to determine the effect of different LDL-lowering therapies on various LDL markers. Study-level correlations between treatment-related changes in lipid parameters and CVD progression were reported, as well as the population percentile achieved based on data from the Framingham Offspring Study. Among the lipid-lowering monotherapies studied, the anti-apoB therapy (mipomersen) and the statins produced the greatest reductions in LDL-P and LDL-C, followed by niacin, fibrates and bile acid sequestrants. Furthermore, the combination of statins with other agents led to greater reductions in LDL-P and LDL-C than the statins alone. Although the combination of fibrates with statins generally decrease LDL-C and LDL-P levels (Table 7), the effect can vary and increases in these parameters have been observed in certain populations [47]. Studies evaluating omega-3-fatty acids as monotherapy were beyond the focus of this review however, a study was published reporting the effects of a pure form of icosapenty ethyl eicosapentaenoic acid (IPE) on lipoprotein particles in hypertiglyceridemic patients. This study showed that in subjects treated with 4 g/day IPE for 12 weeks, changes in LDL-P (−0.1 %) and LDL-C (−6.5 %) from baseline were negligible [48].
Therapies targeting LDL-C are easily evaluated in routine clinical practice because of the widespread availability of LDL-C measurements; LDL-C is most commonly estimated from measurements of total cholesterol using the Friedewald formula. However, as illustrated in this analysis, various treatment options demonstrated variable effects on LDL-C relative to LDL-P. Study-level data from this systematic review showed that statins generally lower LDL-C more than they lower LDL-P, whereas fibrates lower LDL-P more than they lower LDL-C. Therefore, reliance on only LDL-C as a biomarker of LDL-related risk of CVD may not fully appreciate the benefit of these therapies due to the fact that LDL-C and LDL-P may not agree at times and are considered discordant measures.
Why is there discordance between LDL-C and LDL-P?The cholesterol content of LDL particles varies between individuals owing to differences in the relative content of cholesteryl ester and triglycerides within the core of LDL particles [3, 49]. The majority of atherogenic lipoproteins in individuals with insulin resistance, metabolic syndrome or T2D are smaller, cholesterol-depleted LDL particles. These compositional changes in LDL particles may lead to a disagreement between measures of LDL-C and LDL-P resulting in “discordance” [2]. As demonstrated in this analysis, statins tend to lower LDL-C more than LDL-P, hence creating discordance whereby LDL-C targets may be achieved while LDL-P levels remain elevated. This indicates the potential for residual CVD risk.
The clinical consequences of discordant measures of LDL-P and LDL-C have been investigated in MESA [2] and the Framingham Offspring Study [1]. In both studies, in individuals with discordant LDL-P and LDL-C levels, it was LDL-P and not LDL-C that tracked well with CVD risk.
This systematic review also identified 2 randomized controlled trials that reported correlations between lipid and lipoprotein parameters and CVD progression. A strong correlation between on-study LDL-P and CVD progression was observed in the PLAC-1 trial which found that lumen narrowing was associated with higher on-study LDL-P, independent of LDL-C, HDL-C, and triglycerides [46]. In addition, the VA-HIT study found that on-study LDL-P was a strong, independent predictor of new coronary events, while on-study LDL-C, HDL-C, and triglycerides were not significant predictors of CVD risk [4]. Overall, these results are consistent with study-level analyses from several large epidemiologic studies, including the EPIC-Norfolk [50, 51], Framingham Offspring [1], MESA [2], and Women’s Health studies [5, 15], which found that LDL-P was a better discriminator of cardiovascular risk than LDL-C.
Lipoprotein Management
Measurement of LDL-P levels is recommended for high-risk patients whose LDL-C levels are optimal, near optimal or borderline-high, but who also have additional CHD risk equivalents. These include patients with CVD, metabolic syndrome or T2D that are near or at a LDL-C goal of >70 mg/dL and <100 mg/dL; or patients with metabolic syndrome, low HDL-C levels or T2D near or at a goal of LDL-C <100 mg/dL. What therapeutic targets should be established for apoB, LDL-C, non-HDL-C, and LDL-P in these patients? The American Association of Clinical Chemistry (AACC) suggest the following goals: apoB <80 mg/dL, LDL-C <100 mg/dL, non-HDL-C <120 mg/dL and LDL-P <1100 nmol/L [6, 52]. When a patient is at or near their LDL-C goal with discordantly high LDL-P, then one can conclude that the patient has residual LDL-related risk and more intense LDL lowering therapy is needed. Conversely, when LDL-P levels are within the target range, then current therapy is adequate [3]. Therefore, the information gleaned from the LDL-P concentration should be utilized to aid clinical decision-making regarding drug choice and dosing. This can be especially helpful with regard to combination therapies which differentially affect LDL-C and LDL-P [44].
Perspectives and Future Directions
In this study, we conducted a systematic review that reports the effects of multiple classes of lipid modifying agents on LDL-C and LDL-P. In the future, new classes of LDL-C lowering therapies will further challenge the use of the Friedewald formula to calculate LDL-C levels. Certain medications that inhibit CETP [53] and proprotein convertase subtilisin/kexin type 9 (PCSK9) [54] have reported limitations of the LDL-C estimation by the Friedewald formula, which overestimates the LDL-C lowering effect of these agents when compared to standardized ultracentrifugation methods (beta quantification). These obstacles may be overcome by measuring LDL-P and/or apoB.
LDL-P measurements provide more accurate information concerning risk stratification in most studies, and a potential target to guide adjustment for LDL-C lowering therapy. Among subjects with LDL-C at their minimal acceptable goal, an elevated LDL-P would confer risk that may be reduced by adjustment of the statin dosage, change in statin from a less efficacious to more efficacious agent, or the addition of a further LDL-P lowering agent. Contemporary lipid lowering management practices tend to overtreat with statins, particularly for intermediate and high risk patients, to LDL-C values that are pushing beyond 70 mg/dL. The use of LDL-P as a management target in the presence of discordantly high LDL-P values can individualize aggressive lipid-lowering therapy and in the process potentially reduce statin intolerance and be more cost-efficient. In addition, patients with LDL-C above their minimal acceptable target who have low LDL-P may not need intensification of their cholesterol lowering therapies.
References
Cromwell WC, Otvos JD, Keyes MJ, et al. LDL particle number and risk of future cardiovascular disease in the framingham offspring study - implications for LDL management. J Clin Lipidol. 2007;1:583–92.
Otvos JD, Mora S, Shalaurova I, Greenland P, Mackey RH, Goff Jr DC. Clinical implications of discordance between low-density lipoprotein cholesterol and particle number. J Clin Lipidol. 2011;5:105–13.
Rosenson RS, Davidson MH, Pourfarzib R. Underappreciated opportunities for low-density lipoprotein management in patients with cardiometabolic residual risk. Atherosclerosis. 2010;213:1–7.
Otvos JD, Collins D, Freedman DS, et al. Low-density lipoprotein and high-density lipoprotein particle subclasses predict coronary events and are favorably changed by gemfibrozil therapy in the veterans affairs high-density lipoprotein intervention trial. Circulation. 2006;113:1556–63.
Mora S, Otvos JD, Rifai N, Rosenson RS, Buring JE, Ridker PM. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation. 2009;119:931–9.
Davidson MH, Ballantyne CM, Jacobson TA, et al. Clinical utility of inflammatory markers and advanced lipoprotein testing: advice from an expert panel of lipid specialists. J Clin Lipidol. 2011;5:338–67.
Contois JH, McNamara JR, Lammi-Keefe CJ, Wilson PW, Massov T, Schaefer EJ. Reference intervals for plasma apolipoprotein B determined with a standardized commercial immunoturbidimetric assay: results from the Framingham Offspring Study. Clin Chem. [Comparative Study Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, Non-P.H.S. Research Support, U.S. Gov’t, P.H.S.]. 1996 Apr;42:515–23.
Ikewaki K, Terao Y, Ozasa H, et al. Effects of atorvastatin on nuclear magnetic resonance-defined lipoprotein subclasses and inflammatory markers in patients with hypercholesterolemia. J Atheroscler Thromb. 2009;16:51–6.
Jones PH, Dayspring T, Setze C, Lele A, Kelly M, Thakker K. Effects of fenofibric acid in combination with statin therapy on LDL and HDL particle number in patients with mixed dyslipidemia. J Clin Lipidol. 2011;5:202.
McKenney JM, McCormick LS, Schaefer EJ, Black DM, Watkins ML. Effect of niacin and atorvastatin on lipoprotein subclasses in patients with atherogenic dyslipidemia. Am J Cardiol. 2001;88:270–4.
Maki KC, Lawless AL, Kelley KM, et al. Effects of prescription omega-3-acid ethyl esters on fasting lipid profile in subjects with primary hypercholesterolemia. J Cardiovasc Pharmacol. 2011;57:489–94.
Rosenson RS, Otvos JD, Hsia J. Effects of rosuvastatin and atorvastatin on LDL and HDL particle concentrations in patients with metabolic syndrome: a randomized, double-blind, controlled study. Diabetes Care. 2009;32:1087–91.
Schaefer EJ, McNamara JR, Tayler T, et al. Comparisons of effects of statins (atorvastatin, fluvastatin, lovastatin, pravastatin, and simvastatin) on fasting and postprandial lipoproteins in patients with coronary heart disease versus control subjects. Am J Cardiol. 2004;93:31–9.
Soedamah-Muthu SS, Colhoun HM, Thomason MJ, et al. The effect of atorvastatin on serum lipids, lipoproteins and NMR spectroscopy defined lipoprotein subclasses in type 2 diabetic patients with ischaemic heart disease. Atherosclerosis. 2003;167:243–55.
Blake GJ, Otvos JD, Rifai N, Ridker PM. Low-density lipoprotein particle concentration and size as determined by nuclear magnetic resonance spectroscopy as predictors of cardiovascular disease in women. Circulation. 2002;106:1930–7.
Otvos JD, Shalaurova I, Freedman DS, Rosenson RS. Effects of pravastatin treatment on lipoprotein subclass profiles and particle size in the PLAC-I trial. Atherosclerosis. 2002;160:41–8.
Sponseller CA, Morgan RE, Campbell SE, Yu CY, Davidson MH. Pitavastatin 4 mg significantly reduces LDL-P and increases HDL size compared with Pravastatin 40 mg: results from PREVAIL US. J Clin Lipidol. 2012;6:288.
Stein JH, Merwood MA, Bellehumeur JL, et al. Effects of pravastatin on lipoproteins and endothelial function in patients receiving human immunodeficiency virus protease inhibitors. Am Heart J. 2004;147:E18.
van der Graaf A, Rodenburg J, Vissers MN, et al. Atherogenic lipoprotein particle size and concentrations and the effect of pravastatin in children with familial hypercholesterolemia. J Pediatr. 2008;152:873–8.
Airan-Javia SL, Wolf RL, Wolfe ML, Tadesse M, Mohler E, Reilly MP. Atheroprotective lipoprotein effects of a niacin-simvastatin combination compared to low- and high-dose simvastatin monotherapy. Am Heart J. 2009;157:687–e1-8.
Chan SY, Mancini GB, Ignaszewski A, Frohlich J. Statins but not fibrates improve the atherogenic to anti-atherogenic lipoprotein particle ratio: a randomized crossover study. BMC Clin Pharmacol. 2008;8:10.
Miller M, Dolinar C, Cromwell W, Otvos JD. Effectiveness of high doses of simvastatin as monotherapy in mixed hyperlipidemia. Am J Cardiol. 2001;87:232–4. A9.
Ikewaki K, Tohyama J, Nakata Y, Wakikawa T, Kido T, Mochizuki S. Fenofibrate effectively reduces remnants, and small dense LDL, and increases HDL particle number in hypertriglyceridemic men - a nuclear magnetic resonance study. J Atheroscler Thromb. 2004;11:278–85.
Rosenson RS. Fenofibrate reduces lipoprotein associated phospholipase A2 mass and oxidative lipids in hypertriglyceridemic subjects with the metabolic syndrome. Am Heart J. 2008;155:499 e9–16.
Ayaori M, Momiyama Y, Fayad ZA, et al. Effect of bezafibrate therapy on atherosclerotic aortic plaques detected by MRI in dyslipidemic patients with hypertriglyceridemia. Atherosclerosis. 2008;196:425–33.
Ikewaki K, Noma K, Tohyama J, Kido T, Mochizuki S. Effects of bezafibrate on lipoprotein subclasses and inflammatory markers in patients with hypertriglyceridemia–a nuclear magnetic resonance study. Int J Cardiol. 2005;101:441–7.
Dube MP, Wu JW, Aberg JA, et al. Safety and efficacy of extended-release niacin for the treatment of dyslipidaemia in patients with HIV infection: AIDS Clinical Trials Group Study A5148. Antivir Ther. 2006;11:1081–9.
Jafri H, Alsheikh-Ali AA, Mooney P, Kimmelstiel CD, Karas RH, Kuvin JT. Extended-release niacin reduces LDL particle number without changing total LDL cholesterol in patients with stable CAD. J Clin Lipidol. 2009;3:45–50.
Le NA, Jin R, Tershakovec AM, et al. Changes in lipoprotein particle number with ezetimibe/simvastatin coadministered with extended-release niacin in patients with type II hyperlipidemia. J Clin Lipidol. 2012;6:254.
Morgan JM, Capuzzi DM, Baksh RI, et al. Effects of extended-release niacin on lipoprotein subclass distribution. Am J Cardiol. 2003;91:1432–6.
Bays H, Giezek H, McKenney JM, O’Neill EA, Tershakovec AM. Extended-release niacin/laropiprant effects on lipoprotein subfractions in patients with type 2 diabetes mellitus. Metab Syndr Relat Disord. 2012 Mar 8.
McKenney JM, McCormick LS, Weiss S, Koren M, Kafonek S, Black DM. A randomized trial of the effects of atorvastatin and niacin in patients with combined hyperlipidemia or isolated hypertriglyceridemia. Collaborative Atorvastatin Study Group. Am J Med. 1998;104:137–43.
MacLean A, McKenney JM, Scott R, et al. Efficacy and safety of extended-release niacin/laropiprant in patients with type 2 diabetes mellitus. Br J Cardiol. 2011;18:37–45.
Kishimoto N, Fujii S, Chiba H, Sakuma I, Tsutsui H. Colestimide, an anion exchange resin agent, can decrease the number of LDL particles without affecting their size in patients with hyperlipidemia. J Cardiol. 2010;55:65–8.
Rosenson RS. Colesevelam HCl reduces LDL particle number and increases LDL size in hypercholesterolemia. Atherosclerosis. 2006;185:327–30.
Cromwell W, Dufour R, Gagne C, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces small LDL particle number and increases LDL particle size in patients with heterozygous familial Hypercholestrolemia and Coronary Artery Disease AHA Committee on Scientific Sessions 2010. Circulation. 2010
Visser ME, Wagener G, Baker BF, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, lowers low-density lipoprotein cholesterol in high-risk statin-intolerant patients: a randomized, double-blind, placebo-controlled trial. Eur Heart J. 2012;33:1142–9.
Berhanu P, Kipnes MS, Khan MA, et al. Effects of pioglitazone on lipid and lipoprotein profiles in patients with type 2 diabetes and dyslipidaemia after treatment conversion from rosiglitazone while continuing stable statin therapy. Diab Vasc Dis Res. 2006;3:39–44.
Deeg MA, Buse JB, Goldberg RB, et al. Pioglitazone and rosiglitazone have different effects on serum lipoprotein particle concentrations and sizes in patients with type 2 diabetes and dyslipidemia. Diabetes Care. 2007;30:2458–64.
Shadid S, LaForge R, Otvos JD, Jensen MD. Treatment of obesity with diet/exercise versus pioglitazone has distinct effects on lipoprotein particle size. Atherosclerosis. 2006;188:370–6.
Szapary PO, Bloedon LT, Samaha FF, et al. Effects of pioglitazone on lipoproteins, inflammatory markers, and adipokines in nondiabetic patients with metabolic syndrome. Arterioscler Thromb Vasc Biol. 2006;26:182–8.
Goldberg RB, Rosenson RS, Hernandez-Triana E, Misir S, Jones MR. Initial combination therapy with metformin plus colesevelam improves lipoprotein particles in patients with early type 2 diabetes mellitus. J Clin Lipidol. 2012;6:318–24.
Howard WJ, Russell M, Fleg JL, et al. Prevention of atherosclerosis with Ldl-C lowering - lipoprotein changes and interactions: the sands study. J Clin Lipidol. 2009;3:322–31.
Ballantyne CM, Miller M, Niesor EJ, Burgess T, Kallend D, Stein EA. Effect of dalcetrapib plus pravastatin on lipoprotein metabolism and high-density lipoprotein composition and function in dyslipidemic patients: results of a phase IIb dose-ranging study. Am Heart J. 2012;163:515–21. 21 e1-3.
Cromwell WC, Barringer TA. Low-density lipoprotein and apolipoprotein B: clinical use in patients with coronary heart disease. Curr Cardiol Rep. 2009;11:468–75.
Rosenson RS, Otvos JD, Freedman DS. Relations of lipoprotein subclass levels and low-density lipoprotein size to progression of coronary artery disease in the Pravastatin Limitation of Atherosclerosis in the Coronary Arteries (PLAC-I) trial. Am J Cardiol. 2002;90:89–94.
Davidson MH, Rosenson RS, Maki KC, et al. Results from the fenofibric acid on carotid intima-media thickness in subjects with type IIb dyslipidemia with residual risk in addition to atorvastatin therapy (FIRST) trial. J Am Coll Cardiol. 2013;61:E1434.
Bays HE, Braeckman RA, Ballantyne CM, et al. Icosapent ethyl, a pure EPA omega-3 fatty acid: effects on lipoprotein particle concentration and size in patients with very high triglyceride levels (the MARINE study). J Clin Lipidol. 2012;6:565–72.
Jeyarajah EJ, Cromwell WC, Otvos JD. Lipoprotein particle analysis by nuclear magnetic resonance spectroscopy. Clin Lab Med. 2006;26:847–70.
Arsenault BJ, Despres JP, Stroes ES, et al. Lipid assessment, metabolic syndrome and coronary heart disease risk. Eur J Clin Invest. 2010;40:1081–93.
El Harchaoui K, van der Steeg WA, Stroes ES, et al. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007;49:547–53.
Contois JH, McConnell JP, Sethi AA, et al. Apolipoprotein B and cardiovascular disease risk: position statement from the AACC lipoproteins and Vascular Diseases Division Working Group on Best Practices. Clin Chem. 2009;55:407–19 [Practice Guideline Research Support, N.I.H., Intramural].
Davidson M, Liu SX, Barter P, et al. Measurement of LDL-C after treatment with the CETP inhibitor anacetrapib. J Lipid Res. 2013;54:467–72.
Koren MJ, Scott R, Kim JB, et al. Efficacy, safety, and tolerability of a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 as monotherapy in patients with hypercholesterolaemia (MENDEL): a randomised, double-blind, placebo-controlled, phase 2 study. Lancet. 2012;380:1995–2006.
Rosenson RS, Wolff DA, Huskin AL, Helenowski IB, Rademaker AW. Fenofibrate therapy ameliorates fasting and postprandial lipoproteinemia, oxidative stress, and the inflammatory response in subjects with hypertriglyceridemia and the metabolic syndrome. Diabetes Care. 2007;30:1945–51.
Rosenstock J, Fonseca VA, Garvey WT, et al. Initial combination therapy with metformin and colesevelam for achievement of glycemic and lipid goals in early type 2 diabetes. Endocr Pract. 2010;16:629–40.
Acknowledgments
The authors would like to thank Erin R Baker, PhD of S2 Statistical Solutions, Inc. for assistance in the development of the manuscript. S2 Statistical Solutions, Inc. is a paid consultant to LipoScience, Inc.
The study was funded by LipoScience, Inc. NMR lipoprotein measurements are provided by LipoScience, Inc. (Raleigh, NC).
Disclosures
Dr. Robert Rosenson has received grant support from Amgen, F Hoffman LaRoche and Sanofi Aventis; honoraria from Abbott Labs, Amgen, Kowa, LipoScience, Inc., Regeneron, Sanofi Aventis, ShandongLuye, and Sticares InterACT; and has stock or stock options in LipoScience, Inc.
Dr. James Underberg has received consulting fees from LipoScience, Genzyme, Aegerion, Amarin, and Sanofi; has been on the speaker bureau for Abbott, Amarin, GlaxoSmithKline, AstraZeneca, Merck, Kowa, Eli Lilly, Forest, and Daiichi Sankyo; and received research grants from LipoScience, and Kowa Research Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Rosenson, R.S., Underberg, J.A. Systematic Review: Evaluating the Effect of Lipid-Lowering Therapy on Lipoprotein and Lipid Values. Cardiovasc Drugs Ther 27, 465–479 (2013). https://doi.org/10.1007/s10557-013-6477-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-013-6477-6