Abstract
The objective of the study was to document the effect of adipocytokines on endometrial cancer progression. A search of the databases CINAHL, Medline, PubMed, Cochrane, Web of Science, Embase and Google Scholar was performed for English language articles from January 2000 to December 2020 using the keywords: (Endometrial cancer) AND (progression OR metastasis) AND (adipocytokine OR adiponectin OR leptin OR visfatin OR IL-6 OR TNF-α OR adipokine OR cytokine). Forty-nine studies on adipocytokines have been included in this review. Adiponectin has been linked with anti-proliferative and anti-metastatic effects on endometrial cancer cells and is associated with a better prognosis. Leptin, visfatin and resistin are linked to the stimulation of endometrial cancer growth, proliferation, invasion and metastasis and are associated with worse prognosis or with a higher grade/stage of endometrial cancer. IL-6, Il-11, IL-31, IL-33, TNF-α, TGF-β1, SDF-1 and CXCR are involved in endometrial cancer cell growth and metastasis or involved in epithelial mesenchymal transformation (EMT) or associated with advanced disease. Adipocytokines have been found to directly impact endometrial cancer cell proliferation, invasion and migration. These molecules and their signalling pathways may be used to determine prognosis and course of the disease and may also be exploited as potential targets for cancer treatment and prevention of progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Rising obesity rates are thought to be an important contributor to the increasing incidence of cancer in general, including cancer of the endometrium [1]. Endometrial cancer is the 4th commonest cancer in women in the United Kingdom (UK) [2] and in the United States of America (USA) [3]. In 2018, 380,000 new endometrial cancer cases were reported worldwide [4]. In the UK, 9703 new cases were diagnosed between 2016 and 2018 [2].
There is evidence that sex differences may play a role in the prevalence of obesity-related cancers [5]. In 2014, in the USA, it was estimated that 40% of all diagnosed cancer were overweight or obesity-related, with 55% of them, being diagnosed in women compared to 24% in men [5].
Histologically, endometrial cancer is divided into two subtypes [6] — type 1 or endometrioid, which is well-differentiated, usually diagnosed at an early stage and is mostly associated with a hyper-estrogenic milieu, and type 2 endometrial cancer, which is usually of non-endometrioid, papillary-serous or clear cell subtype and is usually more aggressive in nature [7]. Although type 1 endometrial cancer accounts for approximately 80% of the cases, it is women diagnosed with type 2 endometrial cancer that have been observed to have a higher mortality rate due to the early invasion and metastasis when compared with women diagnosed with type 1 endometrial cancers [7].
Obesity is associated with a state of chronic inflammation due to the deterioration of adipose tissue functions [8, 9]. Inflamed and expanded adipose tissue associated with obesity increases cancer risk more than obesity itself [9]. Emerging scientific evidence suggests that non-cancer cells in the tumour microenvironment, such as adipocytes and macrophages, interact to enhance inflammation, leading to dysregulation of various bio-active mediators called adipocytokines and lead to re-programming of cancer cell metabolism, affecting processes involved in invasion, metastasis and immune clearance, all of which can promote tumour progression [9, 10].
Adipose tissue is the largest endocrine organ and source of adipocytokines, which is a joint term [11] used to include cytokines such as interleukin-6, 10 (IL-6,10), tumour necrosis factor-α (TNF-α), chemokine (C-C motif) ligand 2 (CCL2), transforming growth factor-β (TGF-β) and peptides called adipokines, such as adiponectin, leptin and visfatin. They are mainly but not exclusively secreted from the white adipose tissue — the adipokines from the adipocytes and the cytokines from the immune cells infiltrating the adipose tissue. They are involved in cancer signalling acting via endocrine, autocrine and paracrine routes [12]. For simplicity of description, we have discussed the adipocytokines under two sub-headings adipokines and cytokines. Adiponectin and leptin are the two most abundant adipocytokines [13].
1.1 Adipokines
More than hundred different adipokines have been discovered. On review of the literature, adiponectin, leptin, resistin and visfatin are found to be most commonly studied in the context of endometrial cancer risk and progression [14, 15]. In obese women, adipose tissue secretes less adiponectin, which is an anti-inflammatory adipokine, and more inflammatory adipokines such as leptin and visfatin, creating an inflammatory micro-environment that stimulates a cascade of downstream inflammatory pathways that may have mitogenic, anti-apoptotic and angiogenic effects [16, 17]. Other commonly known adipokines include resistin, vaspin, omentin, chemerin, apelin, progranulin, monocyte chemotactic protein 1 (MCP-1), plasminogen activator inhibitor-1 (PAI-1), retinol binding protein-4 (RBP-4) and complement C1q tumour necrosis factor–related protein-4 (CTRP-4) [15].
Among adipocyte-derived factors, adiponectin is the most studied as it is the most abundant in the plasma [10, 18]. A review by Tumminia et al. reported that adiponectin exerts a critical role in the pathogenesis of obesity associated disorders including cancer [19]. Two meta-analyses have demonstrated decreased adiponectin levels in obese endometrial cancer patients compared to non-obese endometrial cancer patients [18, 20], from which we may infer that adiponectin, which has an anti-inflammatory effect, reduces the risk of endometrial cancer. Leptin is another commonly studied adipokine, high levels of which are associated with obesity. A recent meta-analysis [20] on endometrial cancer and adipocytokines has collected a host of evidence, all that point towards a positive association between leptin levels and endometrial cancer. Leptin directly interacts with peripheral tissues and indirectly interacts with various hypothalamic pathways that regulate immune function, cytokine production, angiogenesis, carcinogenesis and many such biological processes [10]. Leptin can activate transcriptional programs for several cellular processes, such as cell growth, proliferation, survival, migration and differentiation, all of which is commonly dysregulated in cancer [10, 21]. Another pro-inflammatory adipokine, visfatin, has been found to be significantly high in patients with endometrial cancer and has been implicated in endometrial cancer progression [22]. Similarly, another adipokine, resistin, has been reported to be involved in upregulation of inflammatory pathways and involved in the development and progression of type 2 endometrial cancer [15, 23]. Vaspin is an adipokine derived from serpin A12 (a visceral adipose-specific serpin), structurally a member of serine protease family. It has been reported to promote carcinogenesis [15]. Omentin-1 is an adipokine synthesized by vascular cells of visceral fat adipose tissue. Lower levels of circulating omentin have been associated with higher endometrial cancer incidence [24]. Omentin is considered a pro-apoptotic and anti-inflammatory adipokine [25], and several solid cancers such as colorectal, prostate and breast cancers are characterized by altered levels of omentin [26].
1.2 Cytokines
Cytokines are low-molecular-weight proteins that mediate autocrine or paracrine signalling effects. The tumour microenvironment (TME) [27, 28] plays a pivotal role in cancer development and spread by creating a milieu where there is crosstalk between cancer cells and stromal cells. Obese adipose tissue is infiltrated by various inflammatory cells such as fibroblasts, mast cells and lymphocytes. These inflammatory cells themselves secrete or stimulate epithelial cells and pre-cancerous cells to secrete inflammatory mediators such as interleukins 6 and 11 (IL-6, IL-11) and tumour necrosis factor-alpha (TNF-α) [27]. Depending on the signalling pathways in the tumour microenvironment, the cytokines can regulate cell proliferation, survival, differentiation, migration and death. They can mount either an anti-tumoral response, as during a state of normal homeostasis, or they can also induce cell transformation (epithelial-mesenchymal transformation) and malignancy as during a state of chronic inflammation, based upon the relative concentrations of pro- and anti-inflammatory cytokines, their receptor expressions and surrounding cell activation [28]. Raised levels of IL-6 have been associated with cancer cell proliferation, angiogenesis and metastasis [29]. IL-6 stimulates adhesion and matrix molecules such as N-cadherin, vimentin, snail, twist and E cadherin and also stimulates stem cell recruitment and self-renewal which all together contribute towards not only cancer development but also its progression and distant spread [29]. A study on endometrial cancer by Chopra et al. [30] states that cytokines such as IL-8, TNF-α and TGF-β have angiogenic properties, activating various cascades of reaction involving angiogenin and other facilitatory growth factors and interleukins (such as IL-6) stimulating the proliferation of vascular endothelial cells and inducing angiogenesis which are hallmarks of cancer development. On the other hand, anti-angiogenic cytokine such as IL-10 is found to be inversely related to the levels of angiogenic cytokines.
Chemokines are a type of cytokine that induce the movement of immune cells along a chemo-attractant gradient, i.e. cells expressing a specific chemokine receptor migrate towards a higher concentration of that chemokine [31]. Chemokines potentially influence tumour infiltration, growth, cell migration and angiogenesis by facilitating movement of inflammatory and tumour cells. Chemokines such as stromal cell–derived factor 1 (SDF-1) [31] and C-C motif chemokine ligand 2 (CCL-2) have also been included in the list of adipocytokines. SDF-1 acts via receptors such as CXC chemokine receptor type 4 (CXCR4) and CXC chemokine receptor type 7 (CXCR7). CXCR4 and its ligand SDF-1 have been found to be related to chemotaxis and tumour progression and metastasis in various cancers [31].
2 Objectives
The aim of this systematic review of literature is to describe the effect of adipocytokines on endometrial cancer progression. This will be achieved by reporting correlations between adipocytokines and cell proliferation, migration and invasion and/or by reporting the statistical association of adipocytokines with features of advanced endometrial cancer such as higher grade, higher stage, metastasis, reduced survival or recurrent disease.
3 Methods
3.1 Protocol and registration
A protocol for the review was devised and registered with PROSPERO (Registration No. CRD42021241605).
3.2 Eligibility criteria
3.2.1 Inclusion criteria
-
a)
English language studies from January 2000 to December 2020
-
b)
Studies including human subjects and endometrial cancer cell lines
-
c)
Observational/ experimental study design
-
d)
Exposure of interest: adipocytokines only, i.e. any adipokine or cytokine
-
e)
Outcome of interest: endometrial cancer progression
-
f)
Effect on endometrial cancer progression demonstrated either by direct experimentation demonstrating effect of adipocytokines on cell proliferation, migration and invasion or by demonstrating correlation between adipocytokines and markers of endometrial cancer progression such as higher tumour stage, grade, myometrial invasion, lymph node invasion or distant metastasis
3.2.2 Exclusion criteria
-
a)
Review articles on the subject
-
b)
Endometrial cancer not the primary cancer
-
c)
Studies involving effect of any other biomarkers on endometrial cancer progression except for the ones mentioned in the search criteria were not included
-
d)
No mention of effect of adipocytokines on progression of endometrial cancer
-
e)
Animal studies (however, studies with both human and animal study arms have been included in the systematic review without going into any description of the animal study arm)
3.3 Information sources
A search of the databases CINAHL, Medline, PubMed, Cochrane, Web of Science, Embase and Google Scholar was performed to identify relevant keywords contained in the title and abstract. A grey literature search was also performed to search for relevant conference abstracts, book chapters, leaflets and dissertations.
3.4 Search strategy
The search keywords were (endometrial cancer) AND (progression OR metastasis) AND (adipocytokine OR adiponectin OR leptin OR visfatin OR IL-6 OR TNF-α OR adipokine OR cytokine). Articles published in the last 20 years (January 2000 till December 2020) in English and indexed in the above databases were identified. Studies were also identified from bibliography search of the articles found in the first search based on their title.
Thereafter, duplicate studies and animal studies that were not relevant were excluded. Full texts were obtained for articles identified by the search and considered to meet the inclusion criteria, based on their title and abstract. These articles were screened for relevance and inclusion in the systematic review for data extraction and synthesis.
The eligibility of each study was checked independently by two reviewers (IR and PE). The lists of included studies selected by the 2 reviewers were then compared, and any disagreement was resolved through discussion with an independent third reviewer (LM).
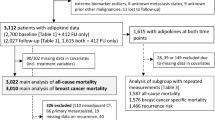
The search for articles for the study have been performed following the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta Analyses Protocols) [32] and is presented in the form of a flow-diagram (Fig. 1).
3.5 Data extraction
Data from each study included in the review were extracted by two independent reviewers (IR and PE). Extracted data elements included first author’s name, publication year, study country, sample population — human samples/cell lines, study design and laboratory assays, primary results related to study criteria and secondary findings.
3.6 Risk of bias in individual studies
These studies were assessed independently for their content and methodological validity by two reviewers (IR and PE), prior to inclusion in the review. Any disagreement was resolved through discussion with an independent third reviewer (LM). The studies included were assessed for their ethical conduct and sourcing of materials.
3.7 Synthesis of results
The studies that satisfy the inclusion criteria were divided into two groups: Experimental studies and observational studies.
-
1.
Experimental studies demonstrated the effect of adipocytokines in terms of dose-response relationships and/or time-response relationships either via cell cycle, cell invasion or cell migration studies or by demonstrating variation in the levels of various markers of cell cycle progression, cell proliferation, apoptosis, adhesion or migration in the form of dose-response and/or time-response relationships.
-
2.
Observational studies are those that correlate the levels of adipocytokines with markers of endometrial cancer progression such as higher tumour stage or grade, more aggressive type II endometrial cancer, myometrial invasion, lymph node invasion or distant metastasis or recurrence and/or poor survival.
After dividing into the two initial groups, the findings of the studies were extracted from each study’s results and discussion sections, grouped into clusters based on their modes of action and general conclusions were drawn for each cluster in the form of narrative synthesis.
The data synthesis plan has been laid out in the following flowchart (Fig. 2).
4 Results
4.1 Search results and publication characteristics
The initial database search identified 855 articles in English language that were published between January 2000 and December 2020. A total of 689 articles were excluded for duplication and lack of relevance. A full-text review was performed for the remaining 166 articles. A further 117 articles were excluded as they were either solely animal studies or review articles or not relevant as per the inclusion criteria. Finally, 49 articles have been selected for inclusion into this systematic review: 33 studies are experimental, 12 observational and 4 combined experimental and observational. The characteristics of these studies are presented in Table 1.
4.2 Experimental studies
Thirty-seven articles have been included in this group (4 overlapping with observational studies). The articles have been further subdivided into pro and anti-inflammatory sub-groups alluding broadly to their role in the inflammation process and cancer progression.
4.2.1 Anti-inflammatory adipocytokines
Among the included studies, the review noted only three adipocytokines to be anti-inflammatory, such as adiponectin, vaspin and omentin-1. These anti-inflammatory adipocytokines have been found to be correlated with slowing of cancer progression. Among the anti-inflammatory adipocytokines, the mode of action of only adiponectin has been reported so far. The various mechanisms by which adiponectin suppresses cancer progression are:
-
Cell proliferation suppression:
Adiponectin was shown to suppress cell proliferation in endometrial cancer cell lines in a concentration-dependent manner [33,34,35,36]. The study by Zhang et al. [33] reported a maximum reduction of cell proliferation (46.1%) with addition of 20 μg/ml adiponectin, and Wu et al. [36] demonstrated decreased proliferation of Ishikawa and SPEC -2 endometrial cancer cells by 47 and 49.5% at 20 μg/ml of adiponectin (dose-dependent decrease, p < 0.05).
-
Induction of apoptosis:
Adiponectin was also shown to induce apoptosis in endometrial cancer cell lines in a concentration-dependent manner [33,34,35,36]. Zhang et al. [33] demonstrated a 3.45-fold increased rate of apoptosis with addition of 20 μg/ml adiponectin, and Wu et al [36] demonstrated increased rates of apoptosis (14.4%, p < 0.05) in Ishikawa and SPEC -2 endometrial cancer cell lines.
-
Cell cycle modulation:
Wu et al. [36] also reported that adiponectin increased cells in resting cell cycle phases G1 and G0 from 48.87 to 71.14% and reduced cells in synthetic phase or S phase from 46.93 to 14.21% (both p < 0.05). A cancer cell is typically progressing, and hence, prevention of progression to synthetic phase will deter cancer progression.
-
Decreased cell invasion:
The same study by Wu et al. mentioned above [36] also demonstrated that adiponectin decreased cell invasion by 66%. Cell invasion is a hallmark of cancer progression and hence adiponectin again demonstrated another role in prevention of cancer progression.
4.2.2 Pro-inflammatory adipocytokines
The majority of the adipocytokines reported are pro-inflammatory and act by opposing mechanisms to the anti-inflammatory adipocytokines. Included in this group are leptin, visfatin, IL-6, TNF-α, IL-8, IL-11, IL-31 and 33, TGF-β, oncostatin M, plasma growth differentiation factor-15 (GDF-15) and RANKL (receptor activator of nuclear factor kB ligand). A study by So et al. [37] culture of endometrial cancer cells produced a range of adipocytokines in the culture medium — chemokine ligand 1 (CXCL1), IL-6, IL-8, migration inhibitory factor (MIF), macrophage chemo-attractant protein-1 (MCP-1 or CCL2), Serpin E1 (PAI-1), TGF-β1 and RANTES. Cancer associated fibroblasts (CAFs) secrete about tenfold higher levels of inflammatory adipocytokines such as MCP-1, IL-6, IL-8, RANTES and SDF-1 (VEGF) than normal fibroblasts [38,39,40].
Several authors have studied the adipocytokines as the primary intervention in endometrial cancer progression experiments. However, we have also included in our review the studies that have demonstrated the adipocytokines to be the ‘middle-man’, i.e. acting as the mediator for other cells (such as stem cells) in endometrial cancer progression or where the adipocytokine is the point of action of some medication to stop endometrial cancer progression (such as medicinal herbs).
The pro-inflammatory adipocytokines have been found to act by the following mechanisms:
-
Cell proliferation:
Leptin has been demonstrated to promote endometrial cancer cell proliferation in various studies [41,42,43,44]. Wu et al. demonstrated that leptin significantly increased the proliferation of Ishikawa cells and SPEC-2 cells by 96% and 92.5% at the concentration of 1 μg/ml and 109.5% and 103.5% at the concentration of 2 μg/ml, respectively (p < 0.05) [36]. Visfatin promoted cell proliferation (p < 0.05) in the study by Wang et al. [45].
Various studies demonstrated the proliferative role of IL-6 [37, 39, 46,47,48,49,50]. A study by Che et al. [47] reported that addition of IL-6 antibody to a co-culture of 17β-estradiol and endometrial cancer cells attenuates the estradiol-induced increased endometrial cancer cell growth by 60%, which leads to the conclusion that IL-6 is necessary for the estradiol-induced endometrial cancer cell growth. They also reported that estradiol promotes upregulation of IL-6 in the endometrial cancer culture medium [47]. YAP (yes-associated protein) is a transducer protein involved in the progression of various cancer types and is reported to stimulate endometrial cancer progression via IL-6 and IL-11 elevation in a study by Wang et al. [48] YAP is upregulated in endometrial cancer cell lines and tissues more than in endometrial stromal cells or benign tissue and involved in endometrial cancer progression via IL-6 and IL-11 activation. YAP induces interleukin transcription. In gene knockout experiment with small interfering-YAP (si-YAP), addition of si-YAP suppressed proliferation of endometrial cancer cells and decreased the expression of IL-6 and IL-11, which proves that YAP induces IL-6 and IL-11 which in turn promotes cell proliferation [48]. Chu et al. [49] demonstrated that IL-6 was raised in co-culture media of endometrial cancer cell and adipose-derived stem cells and that IL-6 induced endometrial cancer cell proliferation. Similarly, endometrial cancer cell lines, treated with CAF-conditioned media, lead to endometrial cancer proliferation; however, addition of increasing concentrations of IL-6 neutralizing antibody led to an inhibition of cell proliferation of almost 50% in CAF-conditioned media and only 5% in CAF-unconditioned media. This indicated that CAF stimulates endometrial cancer proliferation via IL-6 signalling [39]. Lay et al. demonstrated that IL-11 had no effect on cell proliferation [51]. A study by Winship et al. reported that IL-11 upregulated chondroitin sulphate proteoglycan (CSPG4) mRNA in endometrial cancer cell lines [52]. Silencing CSPG4 gene expression decreased endometrial cancer cell proliferation; this is an example of indirect role of IL-11 in endometrial cancer progression via CSPG4. TGF-β1 promotes endometrial cancer cell proliferation [37]. This has been indirectly demonstrated by Bokhari et al. [53] who reported that Chinese herbs Scutellaria baicalensis and Fritillaria cirrhosa are beneficial to cancer patients, and both effectively inhibit TGF-β1-induced endometrial cancer cell proliferation. SDF-1 has a role in endometrial cancer cell proliferation [40, 54]. Gu et al. [54] reported that CXCR7 and its ligand SDF-1 were highly expressed in Ishikawa, AN3CA and endometrial cancer tissue and the expression increased in response to 17β-estradiol treatment. Knockdown of CXCR7 by RNA interference (siCXCR7) inhibited the proliferation of Ishikawa and AN3CA cells. Co-culture with CAF increases SDF-1 level and promotes endometrial cancer cell proliferation [40].
-
Cell migration:
IL-6 has been reported to promote endometrial cancer cell migration in various studies [37, 46, 47, 50]. TGF-β1 induces endometrial cancer cell migration including type II endometrial cancer cells [37, 55, 56].
Estrogen-related receptor alpha (ERRα) is significantly elevated in endometrial cancer tissues, especially with nodal metastasis and can directly bind to promoter of TGF-β1 and increase its transcription. ERRα can trigger endometrial cancer cell migration via regulation of TGF-β1 [57]. IL-11 treatment resulted in a 50% increase in cell migration in AN3CA endometrial cancer cells [51]. As described above, the study by Winship et al. [52] reported that IL-11 upregulated CSPG4 mRNA in endometrial cancer cell lines. Silencing CSPG4 gene expression decreased endometrial cancer cell migration. So, again, this is an example of indirect role of IL-11 in endometrial cancer progression via CSPG4. Zhu et al. [58] studied the effect of another adipocytokine Oncostatin M. Recombinant human oncostatin M promoted cell migration in endometrial cancer cell lines such as Ishikawa and HEC-1B cells. RANK/RANKL has been noted to stimulate endometrial cancer cell migration [59, 60]. Endometrial cancer cell and CAF co-culture increases SDF-1 level which in turn promotes endometrial cancer cell migration [40]. SDF-1-induced cell migration is blocked by Kisspeptin 10 (potent angiogenesis inhibitor) in the study by Shimdt et al. [61].
-
Cell invasion:
Leptin demonstrates a stimulatory effect on endometrial cancer cell invasion [36, 41, 43, 44]. A study conducted by Wu et al. demonstrated a sixty five percent increased leptin-induced endometrial cancer cell invasion [36].
IL-6 and TGF-β1 treatments promote overexpression of matrix proteins such as MMP-2 and MMP-9, which are known markers for cell invasion [37, 50]. As previously described, Chu et al. [49] demonstrated that IL-6 induced endometrial cancer cell invasion when endometrial cancer cell is co-cultured with adipose-derived stem cells. TGF- β1 has been correlated with endometrial cancer cell invasion [37, 55]. As mentioned in endometrial cancer cell migration, ERRα can trigger endometrial cancer cell migration via regulation of TGF-β1 [57]. As reported in cell proliferation, Chinese herbs Scutellaria baicalensis and Fritillaria cirrhosa effectively inhibit TGF- β1-induced endometrial cancer cell invasion as also Siegesbeckia orientalis [53, 62] — this is an indirect way of demonstrating effect of TGF- β 1 on endometrial cancer cell invasion. Che et al. [47] reported that addition IL-6 antibody to a co-culture of estradiol and endometrial cancer cells abrogated the estradiol-induced increased endometrial cancer cell invasion marker MMP2 which leads to the conclusion that IL-6 is necessary for the estradiol-induced endometrial cancer cell invasion. Estradiol stimulates TNF-α expression from the endometrial cancer cells. In turn, IL-6 and TNF-α induce the stromal expression of hepatocyte growth factor (HGF) which in turn stimulates endometrial cancer invasion. Addition of hepatocyte GF (HGF) neutralizing antibody or HGF inhibitor NK4 inhibited estradiol-induced endometrial cancer cell invasion, which suggests that HGF treatment increases estradiol-induced invasiveness of endometrial cancer cells. The addition of neutralizing TNF-α antibody reduces the estradiol mediated endometrial cancer cell invasion in both HEC 1A and KLE cell lines (p < 0.05) which indicates that TNF-α is involved in estradiol-induced endometrial cancer cell invasion [63]. In the study by Zhu et al. above, recombinant human OSM was shown to promote invasion in endometrial cancer cell lines [58]. RANK/RANKL has been demonstrated to promote endometrial cancer cell invasion [59, 60]. A conference abstract [64] in the European journal of cancer reported that GDF15 promotes endometrial cancer metastasis by cellular invasion. SDF-1 induces endometrial cancer cell proliferation as seen in the study by Gu et al. [54], and this can be blocked by knockdown of its receptor CXCR7 by RNA interference (siCXCR7). Co-culture with CAF increases SDF-1 level and promotes endometrial cancer cell invasion [40]. This effect on invasion is also blocked by Kisspeptin 10 as in the study by Shimdt et al. [61].
-
Cell adhesion:
IL-11 was also found to increase adhesion of ANC3A endometrial cancer cells to fibronectin, an extracellular matrix protein, while having no effect on the other extracellular matrix proteins [51]. In contrast to ANC3A cell line, IL-11 was found to have no effect on adhesion properties of Ishikawa and HEC1-A cell lines [51].
-
Cell cycle modulation:
Leptin and Visfatin have been demonstrated to stimulate cell cycle progression to S-phase [36, 41,42,43, 45]. Wu et al. [36] described leptin-induced reduction of cells in G1 and G0 phase from 48.77 to 45.65% and increased cells in S-phase from 46.93 to 53.51% (both p < 0.05). Similar results of leptin on cell cycle promotion were noted by Catalano et al. [65] who noted an upregulation of cyclin D1, which is a critical modulator of G1/S transition alongside a downregulation of the major cyclin-dependent kinase inhibitor, p21WAF1/Cip1.
Che et al. [47] reported that addition IL-6 antibody to a co-culture of estradiol and endometrial cancer cells abrogated the estradiol-induced increased endometrial cancer cell cycle promoter cyclin D1 which leads to the conclusion that IL-6 is necessary for the estradiol-induced endometrial cancer cell cycle progression.
-
Apoptosis prevention:
Leptin decreased the rate of endometrial cancer cell apoptosis (3.25%, p < 0.05) in the study by Wu et al. [36] and in a dose-dependent manner up to 150 ng/ml leptin concentration (p < 0.05) in the study by Zhou et al., which also demonstrated a leptin treatment-dependent reduction of active caspase-3, which is a critical effector of apoptosis in cancer [66]. Visfatin also showed similar reduction of apoptosis (p < 0.05) [45].
Che et al. [47] reported that addition IL-6 antibody to a co-culture of estradiol and endometrial cancer cells abrogated the estradiol-induced increased endometrial cancer cell apoptosis inhibition markers Bcl-2 and Mcl-1, which lead to the conclusion that IL-6 is necessary for the estradiol-induced inhibition of endometrial cancer cell apoptosis.
-
Epithelial mesenchymal transformation (EMT):
Pro-inflammatory adipocytokines promote epithelial mesenchymal transformation, which is one of the most important steps towards cancer development and metastasis. IL-6 and TGF-β1 treatments of endometrial cancer cell lines were demonstrated to affect a decrease in epithelial marker (E cadherin) and an increase in mesenchymal markers (Twist, Snail, N-cadherin) [37, 50, 55]. Treatment with Chinese herbs Scutellaria baicalensis and Fritillaria cirrhosa in the study by Bokhari et al. [53] and Siegesbeckia orientalis in the study by Chang et al. [62] and fluorene-9-bisphenol in the study by Wang et al. [67] inhibited TGF-β1-induced expression of EMT markers Snail, Slug and Focal adhesion kinase, again demonstrating, indirectly, the effect of TGF-β1 on EMT. A conference abstract [64] in the European journal of Cancer reported that GDF15 promotes endometrial cancer metastasis by EMT. RANK level has been positively correlated with N-cadherin (p = 0.0229) and Vimentin (p = 0.0398), but negatively with E-cadherin (p = 0.0118), indicating its role in EMT. RANK overexpressed endometrial cancer cells had higher levels of CCL20 which facilitates invasion and EMT of RANK overexpressed endometrial cancer cells [68]. CCL-18 has been shown to have a mediating effect on endometrial cancer progression by EMT in a study by Jing et al. [69].
The roles of adipocytokines mentioned above have been summarized in a table format (Table 2).
4.3 Observational studies
Sixteen articles have been included in this group (4 overlapping with experimental studies).
4.3.1 Anti-inflammatory adipocytokines
As mentioned in experimental studies, adiponectin is the main anti-inflammatory adipocytokine. Lower levels of anti-inflammatory adipocytokines have been associated with progression of endometrial cancer such as higher grade, stage and lymph node involvement.
Low levels of adiponectin (<8 mg/l) were found to have significant association with higher stage II or III, grade 3 and lymph node involvement, which are clinico-pathological markers for endometrial cancer progression [33]. There was a paucity of studies on other anti-inflammatory adiponectin, but in an observational study by Cymbaluk-Płoska et al. [70], lower concentration of Vaspin was noted in presence of LN involvement (p = 0.022), lymphatic vessel invasion (p = 0.03) and deep myometrial invasion (p = 0.04) and significantly lower concentration of Omentin-1 in the presence of lymphatic vessel invasion (p = 0.002) and deep myometrial invasion (p = 0.01) [70].
4.3.2 Pro-inflammatory adipocytokines
Higher levels of pro-inflammatory adipocytokines such as leptin, visfatin, resistin, IL-6, IL-8, IL-31, IL-33, TNF-α, GDF, Oncostatin M and SDF-1 are associated with an advanced state of endometrial cancer such as high grade II/III, deeper myometrial invasion, lymph vessel invasion, lymph node metastasis, shorter survival and recurrence [40, 58, 59, 66, 68, 70,71,72,73,74,75,76,77,78,79,80].
Leptin levels have been found to be positively correlated with depth of myometrial invasion, lymph node metastasis [71], lymph vessel involvement [70], poor 3-year survival [71] and poorly differentiated endometrial cancer [66, 70] which indicate an advanced disease but was found to be inversely related with histological grade [71]. Koda et al. [72] also observed correlation between positive leptin expression and more locally advanced and moderately differentiated endometrial cancer, although the results did not reach statistical significance. Significantly higher concentrations of visfatin have been demonstrated [73] in patients with advanced endometrial cancers, for example in cases with invasion of blood vessels, lymph node metastasis, deeper infiltration of the endometrium [73] or deeper myometrial invasion [74, 75]. Mean visfatin levels were significantly different between depth of myometrial invasion (10.6 ± 7.6 ng/ml in <50% invasion and 23.5 ± 16.2 ng/ml in >50% invasion, p = 0.019) [74]. No difference was found in case of lymphatic vessel invasion [73]. Setting a cut-off level for visfatin at 20.7 ng/ml, the higher the levels of visfatin, the shorter was the overall survival of patients (p = 0.03) [73]. Similar results in the study by Tian et al [75], where overall survival rate of endometrial cancer patients was significantly higher in the group with negative visfatin expression than with positive visfatin expression (p = 0.035). Resistin was associated with increased lymph node metastasis (p = 0.046) in the observational study by Ilhan et al. [74].
IL-8 concentration was found to be 65% elevated in patients with endometrial cancer compared to control population (p < 0.0001). However, no correlation with stage or grade of endometrial cancer was noted [76]. In the study by Smith et al. [77], IL-8 levels were significantly higher than IL-6 levels, which were significantly higher than production rates for TNF-α in endometrial cancer cells. Cytokines were more abundant in cells derived from primary tumours than from metastatic sites (p < 0.001 for IL-6) or endometrial cancer cell lines (p < 0.001 for IL-6) [77]. Patients who relapsed had higher levels of IL-8 (p < 0.011) and were associated with shorter disease-free survival (p < 0.048) and overall survival. Levels of IL-8 were significantly (p < 0.002) higher in patients who died during follow-up [76]. Smith et al. [77] observed epithelial TNF-α to be more abundant in endometrial cancer tissue samples from women with advanced stages of endometrial cancer (stage III/IV) (p = 0.018) and was associated with lower survival rate (p = 0.032). Marginally lower rates of survival were also observed in patients with high epithelial cell IL-6 (p = 0.052) and IL-8 (p = 0.078) [77]. Poor overall survival was noted in tumours with high cytokine concentration such as high IL-6 and TNF-α. IL-31 and IL-33 were significantly accumulated in cancer patients (p < 0.001) and higher levels correlated with higher grade of endometrial cancer (p < 0.001) which shows that IL-31 and 33 are associated with a more severe or progressed disease [79]. Serum IL-31 was related to tumour stages (p = 0.024), and serum IL-33 was related to tumour stages (p = 0.035), depth of invasion (p = 0.008), nodal metastases (p = 0.029) and distant metastases (p = 0.036) [79]. Their receptors (IL-31R and ST2 respectively) were also highly expressed in endometrial cancer cells (p < 0.001) and higher expression correlated with advanced endometrial cancer and with shorter disease-free survival (all statistically significant) [79]. Only one study by Zhu et al. [58] has been included which reported high oncostatin M expression in endometrial cancer tissue compared to non-cancer endometrial tissue. Significant association was found between increased oncostatin M expression and the depth of myometrial invasion, lymph node metastasis, advanced disease stage (stages III or IV) and poor histological differentiation (grade 3). Engerud et al. [80] noted that high GDF levels correlated with severe disease and independently predicted recurrent disease (OR = 3.14; 95% CI 2.10–4.76) and lymph node metastases (OR = 2.64; 95% CI 1.52–4.61). Patients with high plasma level of GDF-15 had significantly larger tumour volume (p = 0.008). Preoperative plasma level of GDF-15 was significantly higher for patients who experienced recurrence than those who did not develop recurrence and the levels at the time of recurrence were greater than at baseline (p = 0.001). High GDF levels correlated with reduced disease-free survival (p = 0.001); reduced recurrence-free survival (p < 0.001); advanced FIGO stage non-endometrioid histology, high-grade tumour and deep myometrial infiltration (all p < 0.003); recurrent disease, lymph node metastasis and associated with larger tumour volume (p = 0.008); deep myometrial infiltration (p = 0.05); and cervical stromal invasion (p = 0.03) on MRI imaging. RANK/RANKL expression was significantly elevated in endometrial cancer tissue of higher stage, i.e. deeper myometrial invasion, LN and vascular involvement, and showed decreased progression-free survival and overall survival (5 fold higher risk of death) [59, 60, 68]. In a study by Walentowicz-Sadlecka et al. [78], SDF-1 was expressed in 90% of endometrial cancer tissue samples and CXCR4 and CXCR7 were found in 100% endometrial cancer tissue samples. Adjacent normal tissue showed very little expression of CXCR4 and no expression of SDF-1 or CXCR7. Statistically significant correlations were found between SDF-1 and higher clinical stage of endometrial cancer, lymph node metastases, distant metastases, deep myometrial invasion (≥50%), cervical involvement and involvement of adnexa. SDF-1 expression was significantly correlated with the risk of the recurrence (p = 0.0001). Overall survival showed stepwise impairment with increasing SDF-1 expression by Kaplan-Meier analyses. In another study by Teng et al. [40], high SDF-1α expression levels were associated with deep myometrial invasion (p = 0.018), lymph node metastasis (p = 0.038), poor survival (p = 0.039) and higher recurrence rate (p = 0.032).
4.4 Risk of bias in individual studies
Each study was evaluated for their methodological integrity, ethical sourcing of materials and conduct of study before including in the review. However, it was not possible to evaluate the quality of conference abstracts which were included in the review as a part of grey literature search to increase the coverage of the review.
4.5 Risk of bias across studies
We attempted to reduce publication bias by including grey literature search. However, our specified (2000–2020) timed search may have some introduced a time-period bias and English-language literature search may have introduced a language bias.
4.6 Strengths and limitations of our review
The strength of our review is that it presents a relatively comprehensive review of all English language studies in the last 20 years demonstrating the effect of adipocytokines on endometrial cancer progression, their association with poor clinic-pathological markers and their pathway of action. However, use of a specified time range and English language for our search criteria may have introduced a time-period bias and a language bias, respectively. We have performed a grey literature search to reduce the risk of selection bias and have included one conference abstract. PRISMA flowchart has been used to reduce publication and selection bias. All the studies included used either human tissue or endometrial cancer cell lines, mentioned the source of all ingredients and described in detail the tests involved such as proliferation, invasion assay and migration assay. The studies included are from different parts of the world, using cell lines or human tissue from varying sources across the world, but similar results have been found in majority of the studies.
The limitations include that the articles included are not uniform in their cell type/ tissue testing, various studies have used various cell lines procured from various places. Some studies have used human tissue, some fresh, some frozen, or some have used endometrial cell lines and some both. They have also used different tests and ingredients to check for cell proliferation, invasion, or migration. No statistical tests have been used.
5 Further recommendations for research
The current review shows the various ways in which adipocytokines can affect endometrial cancer progression. Further research should explore the signalling pathways by which these adipocytokines affect tumour progression. The inflammatory pathways predominantly reported in the literature on progression of endometrial cancer are the MAPK, JAK/STAT3 and PI3K/AKT /mTOR pathways [81, 82]. Studies are in progress on pI3K/Akt/m-TOR pathway being treated as a therapeutic target in endometrial carcinoma with m-TOR, PI3K, dual PI3K/m-TOR and Akt inhibitors [83, 84], and also, inhibition of the IL-6 receptor and its downstream effectors JAK1 (ruxolitinib) and STAT3 (nifuroxazide) are being investigated for its effect on tumour cell growth in vivo and in vitro studies [85]. mTORC1 inhibitors currently in clinical development stage are everolimus, temsirolimus and ridaforolimus, which have all showed antitumor activity in endometrial cancer cell lines [86]. In a study by Cantrell et al., metformin has been reported to inhibit endometrial cancer cell proliferation, which was partially mediated through AMPK activation and subsequent inhibition of the mTOR pathway [87]. Further trials should be directed towards developing adipocytokine-targeted therapy, which will involve specific inhibitors at various stages in their signalling pathways, which may block the proliferation, invasion and migration of endometrial cancer cells and therefore reduce tumour invasion and metastasis in endometrial cancer.
6 Conclusion
Various adipocytokines have been implicated in the pathogenesis of endometrial cancer by their involvement in the invasion and migration of the cancer cells. This may lead to a higher stage of disease, which ultimately culminates in a poor prognosis, poor response to anti-cancer treatment, recurrence, reduced disease-free survival or reduced overall survival. Defining the biomarkers involved can contribute to a better tailoring of endometrial cancer treatment to target specific markers and their downstream effectors which would reduce the risk of progression or recurrence of cancer. To the best of our knowledge, this study is the only systematic review on the effect of adipocytokines on endometrial cancer progression and summarises all the relevant English language articles on this subject in the last 20 years. Only a few adipocytokines have been found to be anti-inflammatory in our review such as adiponectin, vaspin and omentin-1, and they have been associated with better prognostic factors such as lower stage and grade of disease. Adiponectin has also been found to slow cancer progression by cell proliferation suppression, induction of apoptosis, cell cycle modulation and decreased cell invasion. On the other hand, there have been studies on several pro-inflammatory adipocytokines such as leptin, visfatin, resistin, IL-6, IL-8, IL-31, IL-33, TNF-α, GDF, oncostatin M and SDF-1, which are not only associated with a more advanced endometrial cancer disease state and poor prognostic factors, but they also promote endometrial cancer progression by mechanisms such as cell proliferation, invasion, migration, adhesion, cell cycle promotion and by inducing EMT. However, the studies are not extensive and need further investigation to confirm the mechanism of action of these adipocytokines and their inter-relationships. More data is needed to create a prediction model for prognostication, identifying patients at highest risk of disease progression and hence suitable for adjuvant chemotherapy and for remission monitoring. Larger prospective studies are needed to assess the effect of the various adipocytokines on endometrial cancer progression in the same cohort of patients or the same endometrial cell lines to provide a uniform basis of comparison across studies for a meta-analysis. Some of the articles in our review demonstrated that adipocytokine-specific inhibitors abrogated endometrial cancer cell proliferation, invasion and migration, so we can infer that possibly adipocytokine-targeted therapy could not only treat cancer but also prevent cancer invasion and metastasis. Targeted treatment drugs trials should probably be the next step in prevention and control of this rapidly increasing gynaecological cancer.
Change history
27 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10555-022-10020-y
References
Dimitrov, T., Gorchev, G., & Tomov, S. (2016). Modern concepts of ethiological pathogenesis and treatment of endometrial carcinoma, research literature review. International Journal of Science and Research (IJSR), 5(7), 440–445.
Uterine cancer incidence statistics. Cancer Research UK. Accessed Oct 2020, from http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/uterine-cancer/incidence#heading-One.
Cancer facts and figures 2021. American Cancer Society. Accessed May 2021 from https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2021.html
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov;68(6):394-424. doi: 10.3322/caac.21492. Erratum in: CA Cancer J Clin. 2020;70(4):313.
Argyrakopoulou, G., Dalamaga, M., Spyrou, N., & Kokkinos, A. (2021). Gender differences in obesity-related cancers. Current Obesity Reports, 10(2), 100–115. https://doi.org/10.1007/s13679-021-00426-0
Makker, A., & Goel, M. M. (2016). Tumor progression, metastasis, and modulators of epithelial-mesenchymal transition in endometrioid endometrial carcinoma: An update. Endocrine-Related Cancer, 23(2), R85–R111. https://doi.org/10.1530/ERC-15-0218
Feinberg, J., Albright, B., Black, J., Lu, L., Passarelli, R., Gysler, S., Whicker, M., Altwerger, G., Menderes, G., Hui, P., Santin, A. D., Azodi, M., Silasi, D.-A., Ratner, E. S., Litkouhi, B., & Schwartz, P. E. (2019). Ten-year comparison study of type 1 and 2 endometrial cancers: Risk factors and outcomes. Gynecologic and Obstetric Investigation, 84, 290–297. https://doi.org/10.1159/000493132
Luhn, P., Dallal, C. M., Weiss, J. M., Black, A., Huang, W. Y., Lacey Jr., J. V., Hayes, R. B., Stanczyk, F. Z., Wentzensen, N., & Brinton, L. A. (2013). Circulating adipokine levels and endometrial cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiology, Biomarkers & Prevention, 22(7), 1304–1312. https://doi.org/10.1158/1055-9965.EPI-13-0258
Himbert, C., Delphan, M., Scherer, D., Bowers, L. W., Hursting, S., & Ulrich, C. M. (2017). Signals from the adipose microenvironment and the obesity-cancer link-a systematic review. Cancer Prevention Research (Philadelphia, Pa.), 10(9), 494–506. https://doi.org/10.1158/1940-6207.CAPR-16-0322
O'Flanagan, C. H., Bowers, L. W., & Hursting, S. D. (2015). A weighty problem: Metabolic perturbations and the obesity-cancer link. Hormone Molecular Biology and Clinical Investigation, 23(2), 47–57. https://doi.org/10.1515/hmbci-2015-0022
Cao, H. (2014). Adipocytokines in obesity and metabolic disease. The Journal of Endocrinology, 220(2), T47–T59. https://doi.org/10.1530/JOE-13-0339
Conde, J., Scotece, M., Gómez, R., López, V., Gómez-Reino, J. J., Lago, F., & Gualillo, O. (2011). Adipokines: Biofactors from white adipose tissue. A complex hub among inflammation, metabolism, and immunity. Biofactors., 37(6), 413–420. https://doi.org/10.1002/biof.185
Tilg, H., & Moschen, A. (2006). Adipocytokines: Mediators linking adipose tissue, inflammation and immunity. Nature Reviews. Immunology, 6, 772–783. https://doi.org/10.1038/nri1937
Booth, A., Magnuson, A., Fouts, J., & Foster, M. (2015). Adipose tissue, obesity and adipokines: Role in cancer promotion. Hormone Molecular Biology and Clinical Investigation, 21(1), 57–74. https://doi.org/10.1515/hmbci-2014-0037
Garikapati, K. K., Ammu, V. V. V. R. K., Krishnamurthy, P. T., Chintamaneni, P. K., & Pindiprolu, S. K. S. S. (2019). Type-II endometrial cancer: Role of adipokines. Archives of Gynecology and Obstetrics, 300(2), 239–249. https://doi.org/10.1007/s00404-019-05181-1
Renehan, A. G., Zwahlen, M., & Egger, M. (2015). Adiposity and cancer risk: New mechanistic insights from epidemiology. Nature Reviews. Cancer, 15(8), 484–498. https://doi.org/10.1038/nrc3967
Dashti, S. G., English, D. R., Simpson, J. A., Karahalios, A., Moreno-Betancur, M., Biessy, C., Rinaldi, S., Ferrari, P., Tjønneland, A., Halkjær, J., Dahm, C. C., Vistisen, H. T., Menegaux, F., Perduca, V., Severi, G., Aleksandrova, K., Schulze, M. B., Masala, G., Sieri, S., et al. (2021). Adiposity and endometrial cancer risk in postmenopausal women: A sequential causal mediation analysis. Cancer Epidemiology, Biomarkers & Prevention, 30(1), 104–113. https://doi.org/10.1158/1055-9965.EPI-20-0965
Zeng, F., Shi, J., Long, Y., tian, H., Li, X., Zhao, A. Z., Li, R. F., & Chen, T. (2015). Adiponectin and endometrial cancer: A systematic review and meta-analysis. Cellular Physiology and Biochemistry, 36(4), 1670–1678. https://doi.org/10.1159/000430327
Tumminia, A., Vinciguerra, F., Parisi, M., Graziano, M., Sciacca, L., Baratta, R., & Frittitta, L. (2019). Adipose tissue, obesity and adiponectin: Role in endocrine cancer risk. International Journal of Molecular Sciences, 20(12), 2863. https://doi.org/10.3390/ijms20122863
Ellis, P. E., Barron, G. A., & Bermano, G. (2020). Adipocytokines and their relationship to endometrial cancer risk: A systematic review and meta-analysis. Gynecologic Oncology, 158(2), 507–516. https://doi.org/10.1016/j.ygyno.2020.05.033
Sharma, D., Saxena, N. K., Vertino, P. M., & Anania, F. A. (2006). Leptin promotes the proliferative response and invasiveness in human EC cells by activating multiple signal-transduction pathways. Endocrine-Related Cancer, 13(2), 629–640. https://doi.org/10.1677/erc.1.01169
Nergiz Avcioglu, S., Altinkaya, S. O., Küçük, M., Yüksel, H., Ömürlü, I. K., & Yanik, S. (2015). Visfatin concentrations in patients with EC. Gynecological Endocrinology, 31(3), 202–207. https://doi.org/10.3109/09513590.2014.975687
Hlavna, M., Kohut, L., Lipkova, J., Bienertova-Vasku, J., Dostalova, Z., Chovanec, J., & Vasku, A. (2011). Relationship of resistin levels with endometrial cancer risk. Neoplasma., 58(2), 124–128. https://doi.org/10.4149/neo_2011_02_124
Holman, L. L., Onstad, M., Zhang, Q., Schmandt, R., Neal, S., Munsell, M., Urbauer, D., Mok, S., & Lu, K. (2014). Serum omentin concentration is a potential biomarker for complex atypical hyperplasia and endometrioid endometrial cancer. Gynecologic Oncology, 133(1), 119. https://doi.org/10.1016/j.ygyno.2014.03.313
Christodoulatos, G. S., Antonakos, G., Karampela, I., Psallida, S., Stratigou, T., Vallianou, N., Lekka, A., Marinou, I., Vogiatzakis, E., Kokoris, S., Papavassiliou, A. G., & Dalamaga, M. (2021). Circulating omentin-1 as a biomarker at the intersection of postmenopausal breast cancer occurrence and cardiometabolic risk: An observational cross-sectional study. Biomolecules., 11(11), 1609. https://doi.org/10.3390/biom11111609
Arjmand M, Moradi A, Akbari A, Mehrad-Majd H. Clinical significance of circulating omentin levels in various malignant tumors: Evidence from a systematic review and meta-analysis. Cytokine. 2020;125. 10.1016/j.cyto.2019.154869.
De Nola, R., Menga, A., Castegna, A., Loizzi, V., Ranieri, G., Cicinelli, E., & Cormio, G. (2019). The crowded crosstalk between cancer cells and stromal microenvironment in gynecological malignancies: Biological pathways and therapeutic implication. International Journal of Molecular Sciences, 20(10), 2401. https://doi.org/10.3390/ijms20102401
Landskron, G., De la Fuente, M., Thuwajit, P., Thuwajit, C., & Hermoso, M. A. (2014). Chronic inflammation and cytokines in the tumor microenvironment. Journal of Immunology Research, 2014, 149185. https://doi.org/10.1155/2014/149185
Bharti, R., Dey, G., & Mandal, M. (2016). Cancer development, chemoresistance, epithelial to mesenchymal transition and stem cells: A snapshot of IL-6 mediated involvement. Cancer Letters, 375(1), 51–61. https://doi.org/10.1016/j.canlet.2016.02.048
Chopra, V., Dinh, T. V., & Hannigan, E. V. (1997). Serum levels of interleukins, growth factors and angiogenin in patients with endometrial cancer. Journal of Cancer Research and Clinical Oncology, 123(3), 167–172. https://doi.org/10.1007/BF01214669
Felix, A. S., Edwards, R., Bowser, R., & Linkov, F. (2010). Chemokines and cancer progression: A qualitative review on the role of stromal cell-derived factor 1-alpha and CXCR4 in EC. Cancer Microenvironment, 3(1), 49–56. https://doi.org/10.1007/s12307-010-0042-7
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed1000097
Zhang, L., Wen, K., Han, X., Liu, R., & Qu, Q. (2015). Adiponectin mediates antiproliferative and apoptotic responses in endometrial carcinoma by the AdipoRs/AMPK pathway. Gynecologic Oncology, 137(2), 311–320. https://doi.org/10.1016/j.ygyno.2015.02.012
Moon, H. S., Chamberland, J. P., Aronis, K., Tseleni-Balafouta, S., & Mantzoros, C. S. (2011). Direct role of adiponectin and adiponectin receptors in endometrial cancer: In vitro and ex vivo studies in humans. Molecular Cancer Therapeutics, 10(12), 2234–2243. https://doi.org/10.1158/1535-7163.MCT-11-0545
Cong L, Gasser J, Zhao J, Yang B, Li F, Zhao AZ. Human adiponectin inhibits cell growth and induces apoptosis in human endometrial carcinoma cells, HEC-1-A and RL95 2. Endocr Relat Cancer. 2007;14(3):713-20. doi: 10.1677/ERC-07-0065. Erratum in: Endocr Relat Cancer. 2007 Dec;14(4):1127.
Wu, X., Yan, Q., Zhang, Z., Du, G., & Wan, X. (2012). Acrp30 inhibits leptin-induced metastasis by downregulating the JAK/STAT3 pathway via AMPK activation in aggressive SPEC-2 endometrial cancer cells. Oncology Reports, 27(5), 1488–1496. https://doi.org/10.3892/or.2012.1670
So, K. A., Min, K. J., Hong, J. H., & Lee, J. K. (2015). Interleukin-6 expression by interactions between gynecologic cancer cells and human mesenchymal stem cells promotes epithelial-mesenchymal transition. International Journal of Oncology, 47(4), 1451–1459. https://doi.org/10.3892/ijo.2015.3122
Subramaniam, K. S., Tham, S. T., Mohamed, Z., Woo, Y. L., Mat Adenan, N. A., & Chung, I. (2013). Cancer-associated fibroblasts promote proliferation of endometrial cancer cells. PLoS One, 8(7), e68923. https://doi.org/10.1371/journal.pone.0068923
Subramaniam, K. S., Omar, I. S., Kwong, S. C., Mohamed, Z., Woo, Y. L., Mat Adenan, N. A., & Chung, I. (2016). Cancer-associated fibroblasts promote endometrial cancer growth via activation of interleukin-6/STAT-3/c-Myc pathway. American Journal of Cancer Research, 6(2), 200–213.
Teng, F., Tian, W. Y., Wang, Y. M., Zhang, Y. F., Guo, F., Zhao, J., Gao, C., & Xue, F. X. (2016). Cancer-associated fibroblasts promote the progression of endometrial cancer via the SDF-1/CXCR4 axis. Journal of Hematology & Oncology, 9, 8. https://doi.org/10.1186/s13045-015-0231-4
Daley-Brown, D., Harbuzariu, A., Kurian, A. A., Oprea-Ilies, G., & Gonzalez-Perez, R. R. (2019). Leptin-induced Notch and IL-1 signaling crosstalk in endometrial adenocarcinoma is associated with invasiveness and chemoresistance. World J Clin Oncol., 10(6), 222–233. https://doi.org/10.5306/wjco.v10.i6.222
Liu, Y., Lv, L., Xiao, W., Gong, C., Yin, J., Wang, D., & Sheng, H. (2011). Leptin activates STAT3 and ERK1/2 pathways and induces endometrial cancer cell proliferation. Journal of Huazhong University of Science and Technology. Medical Sciences, 31(3), 365. https://doi.org/10.1007/s11596-011-0382-7
Gao, J., Tian, J., Lv, Y., Shi, F., Kong, F., Shi, H., & Zhao, L. (2009). Leptin induces functional activation of cyclooxygenase-2 through JAK2/STAT3, MAPK/ERK, and PI3K/AKT pathways in human endometrial cancer cells. Cancer Science, 100(3), 389–395. https://doi.org/10.1111/j.1349-7006.2008.01053.x
Sharma, D., Saxena, N. K., Vertino, P. M., & Anania, F. A. (2006). Leptin promotes the proliferative response and invasiveness in human endometrial cancer cells by activating multiple signal-transduction pathways. Endocrine-Related Cancer, 13(2), 629–640. https://doi.org/10.1677/erc.1.01169
Wang, Y., Gao, C., Zhang, Y., Gao, J., Teng, F., Tian, W., Yang, W., Yan, Y., & Xue, F. (2016). Visfatin stimulates endometrial cancer cell proliferation via activation of PI3K/Akt and MAPK/ERK1/2 signalling pathways. Gynecologic Oncology, 143(1), 168–178. https://doi.org/10.1016/j.ygyno.2016.07.109
Che, Q., Liu, B. Y., Wang, F. Y., He, Y. Y., Lu, W., Liao, Y., Gu, W., & Wan, X. P. (2014). Interleukin 6 promotes endometrial cancer growth through an autocrine feedback loop involving ERK-NF-κB signaling pathway. Biochemical and Biophysical Research Communications, 446(1), 167–172. https://doi.org/10.1016/j.bbrc.2014.02.080
Che, Q., Xiao, X., Xu, J., Liu, M., Lu, Y., Liu, S., & Dong, X. (2019). 17β-Estradiol promotes EC proliferation and invasion through IL-6 pathway. Endocrine Connections, 8(7), 961–968. https://doi.org/10.1530/EC-19-0258
Wang, J., Song, T., Zhou, S., & Kong, X. (2019). YAP promotes the malignancy of endometrial cancer cells via regulation of IL-6 and IL-11. Molecular Medicine, 25(1), 32. https://doi.org/10.1186/s10020-019-0103-4
Chu, Y., Wang, Y., Peng, W., Xu, L., Liu, M., Li, J., Hu, X., Li, Y., Zuo, J., & Ye, Y. (2018). STAT3 activation by IL-6 from adipose-derived stem cells promotes endometrial carcinoma proliferation and metastasis. Biochemical and Biophysical Research Communications, 500(3), 626–631. https://doi.org/10.1016/j.bbrc.2018.04.121
Che, Q., Xiao, X., Liu, M., Lu, Y., Dong, X., & Liu, S. (2019). IL-6 promotes endometrial cancer cells invasion and migration through signal transducers and activators of transcription 3 signaling pathway. Pathology, Research and Practice, 215(6), 152392. https://doi.org/10.1016/j.prp.2019.03.020
Lay, V., Yap, J., Sonderegger, S., & Dimitriadis, E. (2012). Interleukin 11 regulates endometrial cancer cell adhesion and migration via STAT3. International Journal of Oncology, 41(2), 759–764. https://doi.org/10.3892/ijo.2012.1486
Winship, A., Van Sinderen, M., Heffernan-Marks, A., & Dimitriadis, E. (2017). Chondroitin sulfate proteoglycan protein is stimulated by interleukin 11 and promotes endometrial epithelial cancer cell proliferation and migration. International Journal of Oncology, 50(3), 798–804. https://doi.org/10.3892/ijo.2017.3848
Bokhari, A. A., & Syed, V. (2015). Inhibition of transforming growth factor-β (TGF-β) signaling by Scutellaria baicalensis and Fritillaria cirrhosa extracts in endometrial cancer. Journal of Cellular Biochemistry, 116(8), 1797–1805. https://doi.org/10.1002/jcb.25138
Gu, H. Q., Zhang, Z. B., Zhang, J. W., Wang, Q. Q., Xi, X. W., & He, Y. Y. (2017). The role of the SDF-1/ CXCR7 axis on the growth and invasion ability of endometrial cancer cells. Archives of Gynecology and Obstetrics, 295(4), 987–995. https://doi.org/10.1007/s00404-017-4308-x
Wang, X., Zhang, W., Sun, X., Lin, Y., & Chen, W. (2018). Cancer-associated fibroblasts induce epithelial-mesenchymal transition through secreted cytokines in endometrial cancer cells. Oncology Letters, 15(4), 5694–5702. https://doi.org/10.3892/ol.2018.8000
Xiong, S., Cheng, J. C., Klausen, C., Zhao, J., & Leung, P. C. (2016). TGF-β1 stimulates migration of type II endometrial cancer cells by down-regulating PTEN via activation of SMAD and ERK1/2 signaling pathways. Oncotarget., 7(38), 61262–61272. https://doi.org/10.18632/oncotarget.11311
Huang, X., Wang, X., Shang, J., Zhaang, Z., Cui, B., Lin, Y., Yang, Y., Song, Y., Yu, S., & Xia, J. (2018). Estrogen related receptor alpha triggers the migration and invasion of endometrial cancer cells via up regulation of TGFB1. Cell Adhesion & Migration, 12(6), 538–547. https://doi.org/10.1080/19336918.2018.1477901
Zhu, M., Che, Q., Liao, Y., Wang, H., Wang, J., Chen, Z., Wang, F., Dai, C., & Wan, X. (2015). Oncostatin M activates STAT3 to promote EC invasion and angiogenesis. Oncology Reports, 34(1), 129–138. https://doi.org/10.3892/or.2015.3951
Liu, Y., Wang, J., Ni, T., Wang, L., Wang, Y., & Sun, X. (2016). CCL20 mediates RANK/RANKL-induced epithelial-mesenchymal transition in endometrial cancer cells. Oncotarget., 7(18), 25328–25339. https://doi.org/10.18632/oncotarget.8291
Wang, J., Sun, X., Zhang, H., Wang, Y., & Li, Y. (2015). MPA influences tumor cell proliferation, migration, and invasion induced by RANKL through PRB involving the MAPK pathway in endometrial cancer. Oncology Reports, 33(2), 799–809. https://doi.org/10.3892/or.2014.3651
Schmidt, E., Haase, M., Ziegler, E., Emons, G., & Gründker, C. (2014). Kisspeptin-10 inhibits stromal-derived factor 1-induced invasion of human endometrial cancer cells. International Journal of Gynecological Cancer, 24(2), 210–217. https://doi.org/10.1097/IGC.0000000000000050
Chang, C. C., Ling, X. H., Hsu, H. F., Wu, J. M., Wang, C. P., Yang, J. F., Fang, L. W., & Houng, J. Y. (2016). Siegesbeckia orientalis extract inhibits TGF-β1-induced migration and invasion of endometrial cancer cells. Molecules., 21(8), 1021. https://doi.org/10.3390/molecules21081021
Choi, D. S., Kim, H. J., Yoon, J. H., Yoo, S. C., Jo, H., Lee, S. Y., Min, C. K., & Ryu, H. S. (2009). EC invasion depends on cancer-derived tumor necrosis factor-alpha and stromal derived hepatocyte growth factor. International Journal of Cancer, 124(11), 2528–2538. https://doi.org/10.1002/ijc.24238
Billaud J.N.; Dubus E.; Tugendreich S.; Toburen D. Identification of potential immune targets in controlling endometrioid endometrial carcinoma metastatic progression. Conference Abstract. European Journal of Cancer; 2016; vol. 55
Catalano, S., Giordano, C., Rizza, P., Gu, G., Barone, I., Bonofiglio, D., Giordano, F., Malivindi, R., Gaccione, D., Lanzino, M., De Amicis, F., & Andò, S. (2009). Evidence that leptin through STAT and CREB signaling enhances cyclin D1 expression and promotes human endometrial cancer proliferation. Journal of Cellular Physiology, 218(3), 490–500. https://doi.org/10.1002/jcp.21622
Zhou, X., Li, H., Chai, Y., & Liu, Z. (2015). Leptin inhibits the apoptosis of endometrial carcinoma cells through activation of the nuclear factor κB-inducing kinase/IκB kinase pathway. International Journal of Gynecological Cancer, 25(5), 770–778. https://doi.org/10.1097/IGC.0000000000000440
Wang, L., Zhuang, T., Li, F., & Wei, W. (2019). Fluorene-9-bisphenol inhibits epithelial-mesenchymal transition of human endometrial cancer Ishikawa cells by repressing TGF-β signaling pathway. Environmental Science and Pollution Research International, 26(26), 27407–27413. https://doi.org/10.1007/s11356-019-05184-0
Wang, J., Liu, Y., Wang, L., Sun, X., & Wang, Y. (2016). Clinical prognostic significance and pro-metastatic activity of RANK/RANKL via the AKT pathway in endometrial cancer. Oncotarget., 7(5), 5564–5575. https://doi.org/10.18632/oncotarget.6795
Jing, X., Peng, J., Dou, Y., Sun, J., Ma, C., Wang, Q., Zhang, L., Luo, X., Kong, B., Zhang, Y., Wang, L., & Qu, X. (2019). Macrophage ERα promoted invasion of endometrial cancer cell by mTOR/KIF5B-mediated epithelial to mesenchymal transition. Immunology and Cell Biology, 97(6), 563–576. https://doi.org/10.1111/imcb.12245
Cymbaluk-Płoska, A., Chudecka-Głaz, A., Jagodzińska, A., Pius-Sadowska, E., Sompolska-Rzechuła, A., Machaliński, B., & Menkiszak, J. (2018). Evaluation of biologically active substances promoting the development of or protecting against endometrial cancer. Oncotargets and Therapy, 11, 1363–1372. https://doi.org/10.2147/OTT.S155942
Zhang, Y., Liu, L., Li, C., & Ai, H. (2014). Correlation analysis between the expressions of leptin and its receptor (ObR) and clinicopathology in endometrial cancer. Cancer Biomarkers, 14(5), 353–359. https://doi.org/10.3233/CBM-140415
Koda, M., Sulkowska, M., Wincewicz, A., Kanczuga-Koda, L., Musiatowicz, B., Szymanska, M., & Sulkowski, S. (2007). Expression of leptin, leptin receptor, and hypoxia-inducible factor 1 alpha in human endometrial cancer. Annals of the New York Academy of Sciences, 1095, 90–98. https://doi.org/10.1196/annals.1397.013
Cymbaluk-Płoska, A., Chudecka-Głaz, A., Pius-Sadowska, E., Sompolska-Rzechuła, A., Machaliński, B., & Menkiszak, J. (2018). Circulating serum level of visfatin in patients with endometrial cancer. BioMed Research International, 2018, 8576179. https://doi.org/10.1155/2018/8576179
Ilhan, T. T., Kebapcilar, A., Yilmaz, S. A., Ilhan, T., Kerimoglu, O. S., Pekin, A. T., Akyurek, F., Unlu, A., & Celik, C. (2015). Relations of serum visfatin and resistin levels with EC and factors associated with its prognosis. Asian Pacific Journal of Cancer Prevention, 16(11), 4503–4508. https://doi.org/10.7314/apjcp.2015.16.11.4503
Tian, W., Zhu, Y., Wang, Y., Teng, F., Zhang, H., Liu, G., Ma, X., Sun, D., Rohan, T., & Xue, F. (2013). Visfatin, a potential biomarker and prognostic factor for endometrial cancer. Gynecologic Oncology, 129(3), 505–512. https://doi.org/10.1016/j.ygyno.2013.02.022
Kotowicz, B., Fuksiewicz, M., Jonska-Gmyrek, J., Berezowska, A., Radziszewski, J., Bidzinski, M., & Kowalska, M. (2017). Clinical significance of pretreatment serum levels of VEGF and its receptors, IL-8, and their prognostic value in type I and II endometrial cancer patients. PLoS One, 12(10), e0184576. https://doi.org/10.1371/journal.pone.0184576
Smith, H. O., Stephens, N. D., Qualls, C. R., Fligelman, T., Wang, T., Lin, C. Y., Burton, E., Griffith, J. K., & Pollard, J. W. (2013). The clinical significance of inflammatory cytokines in primary cell culture in endometrial carcinoma. Molecular Oncology, 7(1), 41–54. https://doi.org/10.1016/j.molonc.2012.07.002
Walentowicz-Sadlecka, M., Sadlecki, P., Bodnar, M., Marszalek, A., Walentowicz, P., Sokup, A., Wilińska-Jankowska, A., & Grabiec, M. (2014). Stromal derived factor-1 (SDF-1) and its receptors CXCR4 and CXCR7 in EC patients. PLoS One, 9(1), e84629. https://doi.org/10.1371/journal.pone.0084629
Zeng, X., Zhang, Z., Gao, Q. Q., Wang, Y. Y., Yu, X. Z., Zhou, B., & Xi, M. R. (2016). Clinical significance of serum interleukin-31 and interleukin-33 levels in patients of endometrial cancer: A case control study. Disease Markers, 2016, 9262919. https://doi.org/10.1155/2016/9262919
Engerud, H., Hope, K., Berg, H. F., Fasmer, K. E., Tangen, I. L., Haldorsen, I. S., Trovik, J., & Krakstad, C. (2019). Plasma growth differentiation factor-15 is an independent marker for aggressive disease in endometrial cancer. PLoS One, 14(1), e0210585. https://doi.org/10.1371/journal.pone.0210585
Kourea, H. P., Nikolaou, M., Tzelepi, V., Adonakis, G., Kardamakis, D., Tsapanos, V., Scopa, C. D., Kalofonos, C., & Decavalas, G. (2015). Expression of phosphorylated Akt, mTOR and MAPK in type I endometrial carcinoma: Clinical significance. Anticancer Research, 35(4), 2321–2331.
Chen, C. L., Hsieh, F. C., Lieblein, J. C., Brown, J., Chan, C., Wallace, J. A., Cheng, G., Hall, B. M., & Lin, J. (2007). Stat3 activation in human endometrial and cervical cancers. British Journal of Cancer, 96(4), 591–599. https://doi.org/10.1038/sj.bjc.6603597
Slomovitz, B. M., & Coleman, R. L. (2012). The PI3K/AKT/mTOR pathway as a therapeutic target in endometrial cancer. Clinical Cancer Research, 18(21), 5856–5864. https://doi.org/10.1158/1078-0432.CCR-12-0662
Pavlidou, A., & Vlahos, N. F. (2014). Molecular alterations of PI3K/Akt/mTOR pathway: A therapeutic target in endometrial cancer. ScientificWorldJournal., 2014, 709736. https://doi.org/10.1155/2014/709736
Van der Zee, M., Sacchetti, A., Cansoy, M., Joosten, R., Teeuwssen, M., Heijmans-Antonissen, C., Ewing-Graham, P. C., Burger, C. W., Blok, L. J., & Fodde, R. (2015). IL6/JAK1/STAT3 signaling blockade in endometrial cancer affects the ALDHhi/CD126+ stem-like component and reduces tumor burden. Cancer Research, 75(17), 3608–3622. https://doi.org/10.1158/0008-5472.CAN-14-2498
Roncolato, F., Lindemann, K., Willson, M. L., Martyn, J., & Mileshkin, L. (2019). PI3K/AKT/mTOR inhibitors for advanced or recurrent endometrial cancer. Cochrane Database of Systematic Reviews, 10(10), CD012160. https://doi.org/10.1002/14651858.CD012160.pub2
Cantrell, L. A., Zhou, C., Mendivil, A., Malloy, K. M., Gehrig, P. A., & Bae-Jump, V. L. (2010). Metformin is a potent inhibitor of endometrial cancer cell proliferation--implications for a novel treatment strategy. Gynecologic Oncology, 116(1), 92–98. https://doi.org/10.1016/j.ygyno.2009.09.024
Zeng, X., Li, J., Kang, L. N., Xi, M. R., & Liao, G. D. (2020). Potential clinical value of interleukin-31 and interleukin-33 with their receptors expression as diagnostic and predictive factors in endometrial cancer: A case-control study. International Journal of Clinical and Experimental Pathology, 13(6), 1324–1332.
Acknowledgements
1. Alison Paul, librarian, Ashford and St Peters NHS Foundation Trust, UK — for helping us set up the literature search criteria.
2. GRACE charity and Womb Cancer Support UK (WCSUK)
Availability of data and material
Not applicable, as review article, data derived from other studies which have been mentioned using references.
Code availability
No special software or code has been used. Search criteria for articles have been mentioned in the review.
Author information
Authors and Affiliations
Contributions
IR and PE conceptualized this review, developed the protocol, selected the articles for full-text review, performed data extraction and synthesis and wrote the manuscript. LM and AM reviewed the manuscript and provided valuable input.
Corresponding author
Ethics declarations
Ethical considerations
In this systematic review, we used only previously published data. As no unpublished data were used, we did not seek ethics committee approval. The study is according to the PRISMA guidelines for systematic reviews.
Consent to participate
Not applicable
Consent for publication
I, Irene Ray, give my consent for the publication of the systematic review.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The reference citations inside the Table 1 are out of order as the reference citations in the article have been moved around. The original article has been corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ray, I., Meira, L.B., Michael, A. et al. Adipocytokines and disease progression in endometrial cancer: a systematic review. Cancer Metastasis Rev 41, 211–242 (2022). https://doi.org/10.1007/s10555-021-10002-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-021-10002-6