Abstract
A 65-year-old male with chronic liver disease and refractory ascites was being evaluated for liver transplant, when constrictive pericarditis (CP) was suspected. Initial diagnostics were inconclusive due to overdiuresis. After suspension of diuretics, cardiac magnetic resonance confirmed CP, leading to successful pericardiectomy and normalization of liver function, emphasizing volume status and multimodality imaging role in CP diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Case description
A 65-year-old male with chronic liver disease and cirrhosis under evaluation for liver transplant, with a presumptive diagnosis of cirrhosis secondary to nonalcoholic steatohepatitis, had ascites refractory to increasing doses of diuretics. Liver biopsy, liver Doppler ultrasound and magnetic resonance imaging were not consistent with etiology. Transthoracic echocardiogram showed annulus reversus and marked respiratory variation of the pulsed wave Doppler of mitral and tricuspid inflow velocities suggesting constrictive pericarditis (CP), and the patient was referred to our cardiology outpatient clinic. Further work-up with right heart catheterization (RHC) showed very elevated right atrium pressure (35 mmHg), near equalisation of right and left ventricles end-diastolic pressures (36 and 41 mmHg, respectively), with square-root sign. However, it wasn’t able to show dissociation between pulmonary capillary wedge pressure and left ventricle end-diastolic pressure with respiration nor exaggerated ventricular interdependence (Fig. 1), which couldn’t confirm the diagnosis of CP. An initial cardiac magnetic resonance (CMR) demonstrated thickened pericardium, without pericardial effusion, but was also inconclusive for exaggerated ventricular interdependence. Although the RHC and CMR were carried out after fluid challenge, the patient was taking high doses of diuretics and our cardiology team believed the overdiuresis masked the constrictive physiology. Due to the rapid deterioration of liver function tests and the urgent need to decide on the patient’s eligibility for a liver transplant, it was decided to discontinue diuretics and repeat CMR. After one week of interruption of diuretics, a second CMR demonstrating pericardial thickening, exaggerated ventricular interdependence with ventricular septal shift and diastolic interventricular septal bounce (Fig. 2), gave the answers to our dilemma. The patient underwent pericardiectomy, which resolved his symptoms of fluid overload, and the liver function tests slowly returned to normal. Two years later, the patient remains asymptomatic and off the liver transplant list.
Discussion
In the setting of a chronic liver disease, with ascites and abnormal liver function tests, the diagnosis of CP can be overlooked. CP is characterized by two pathophysiological abnormalities: exaggerated ventricular interdependence and intrathoracic- intracardiac pressure dissociation.[1] These abnormalities lead to dynamic changes with respiration, which underlie the characteristic signs observed in both invasive and non-invasive diagnostic tests and contribute to the patient’s symptoms.[2] These classic signs of constriction are more pronounced in euvolemic patients.[3] If these signs are absent in individuals suspected of CP, and volume depletion is present, it is recommended to reassess after fluid replacement or, as in our case, diuretic adjustment. Although RHC remains the gold standard for confirmation of constrictive physiology, multimodality imaging, including CMR, may be useful in uncertain diagnosis. [1]
Conclusion
The diagnosis of CP can be challenging and requires a high level of suspicion. Patients with CP often receive high doses of diuretics for their symptoms, which can obscure the typical signs of the condition in both RHC and imaging studies. Clinicians often need to optimize fluid status in these patients before diagnostic testing to enhance diagnostic accuracy. Additionally, CMR may be essential for a definitive diagnosis.
Right heart catheterization (RHC) showing the simultaneous right and left heart ventricular curves. In constrictive pericarditis, exaggerated ventricular interdependence in RHC should demonstrate that the area under the right ventricular systolic pressure curve increases during inspiration, whereas the area under the left ventricular systolic pressure curve decreases. In our patient, although the area under the left ventricular pressure curves decreases slightly, there isn’t a significant change in the right ventricular ones, even after fluid challenge
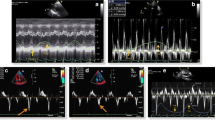
Absence of exaggerated ventricular interdependence on free-breathing protocol of cardiac magnetic resonance (CMR) (A and B) due to marked diuresis. After the interruption of diuretics for one week, a clear phenomenon of exaggerated ventricular interdependence is seen in CMR images (C and D), with ventricular septal shift with respiration cycle: rightward shift of septum during expiration (C) and leftward shift of septum during inspiration (d)
Data availability
No datasets were generated or analysed during the current study.
References
Sohal S, Mathai SV, Lipat K, et al. Multimodality Imaging of Constrictive Pericarditis: Pathophysiology and New Concepts. Curr Cardiol Rep. 2022;24(10):1439–1453.
Al-Kazaz M, Klein AL, Oh JK, et al. Pericardial Diseases and Best Practices for Pericardiectomy. Journal of the American College of Cardiology. 2024;84(6):561–580.
Rocha DFR, Oliveira ACRd, Silva VNe, et al. My Approach to Echocardiographic Assessment for Constrictive Pericarditis. 2023;36(1):-.
Funding
Open access funding provided by FCT|FCCN (b-on).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by BLT, FA, VF, SAR and BT. The first draft of the manuscript was written by BLT and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Teixeira, B.L., Albuquerque, F., Cardoso, I. et al. Overcoming diagnostic challenges in constrictive pericarditis: why volume is important?. Int J Cardiovasc Imaging (2024). https://doi.org/10.1007/s10554-024-03235-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10554-024-03235-3