Abstract
It is known that during the active course of Coronavirus disease 2019 (COVID-19), myocardial injury has an established pathological base, while its myocardial injury post-recovery is still obscured.The aim of this study was to evaluate the longitudinal left atrial strain (LAS) using speckle tracking echocardiography (STE) in COVID-19-recovered patients who are previously healthy without confounder comorbidities to detect the potential cardiac dysfunction.200 patients were prospectively included and examined 4?12 weeks after recovery from COVID-19 infection. 137 participants with comorbidities or previous history of cardiopulmonary disease were excluded from the analysis. A total of 63 patients who fulfilled our inclusion criteria were recruited into two groups according to thepresence or absence of persistent dyspnoea and exercise intolerance. Clinical, laboratory & comprehensive echocardiographic examinations were done for all. We observed that 31.7% of the previously healthy individuals developed dyspnoea & exercise intolerance post-COVID-19 infection. There were significantly impaired LAS parameters in the symptomatic group (LA reservoir, contraction & conduit strain, 22.7%, -6.6% & -16.1% versus 40%, -12%, and ? 27% in the asymptomatic group with P < 0.000). Only LA reservoir strain and LA stiffness can independently predict the development of dyspnoea & exercise intolerance post-COVID-19 at cut-off values of 30% & 24.5% respectively with a sensitivity of 90% and a specificity of 91%, P < 0.001. These impaired LAS parameters could explain the developed symptoms post-COVID-19 recovery, even before disturbed conventional diastolic echocardiographic parameters.LAS parameters are significantly associated with the developed exertional dyspnoea & exercise intolerance post-COVID-19. LA reservoir strain & LA stiffness could provide a simple, easily available tool that points to early LV diastolic dysfunction and may direct the therapy in this subset of the population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic has an established adverse clinical impact on the cardiovascular system. However, little is known about the intermediate & longer-term sequelae of this infection, defined as “long COVID” where persistent COVID-19 symptoms last beyond 12 weeks post-infection [1].
The pathophysiologic basis for the persistent symptoms and functional limitation among patients who have long since recovered from mild acute illness remains unknown. However, Observations point out that this population does not appear to have previous cardiac or pulmonary pathology or any major pulmonary function abnormalities during the acute course of COVID-19 infection [2].
Accordingly, in the current study, we aimed to evaluate subjects who developed exertional dyspnoea, fatigue & exercise intolerance beyond weeks from complete recovery, and who did not show any overt cardiopulmonary residue proved by conventional imaging modalities.
Methods
Study population
200 patients were prospectively included and examined 4–12 weeks after recovery from COVID-19 infection. 137 Participants with comorbidities or previous history of cardiopulmonary disease were excluded from the analysis, total of 63 adults > 18 years old patients who fulfilled the inclusion criteria were included in our study and recruited into two groups; group (A) includes 20 symptomatic subjects who developed exertional dyspnoea, fatigue & exercise intolerance (NYHA class ≥ 2), compared to group (B) includes 43 patients without any residual symptoms. All participants were in sinus rhythm, patients with evidence of coronary artery disease, arterial hypertension, diabetes mellitus, left ventricular (LV) wall motion, LV cardiomyopathy, valvular heart disease, dysrhythmia especially atrial fibrillation, atrioventricular conduction abnormalities on ECG, thyroid dysfunction, pulmonary disease, respiratory failure or poor echocardiographic image quality were excluded from the study. Pulmonary embolism secondary to COVID infection was excluded by CT chest scan
Ethical considerations
This case-control study was approved by our institutional review board (IRB); ZU-IRB#9204/4-1-2022 and conducted at our University Hospital’s cardiology department between October 2021 and October 2022. All procedures were performed following the ethical standards of the national research committee. All participants gave written informed consent to participate in the study.
Transthoracic echocardiography
The echocardiographic examination was performed using a Vivid E95 (General Electric Health Care, WI, USA) ultrasound machine, and images were acquired with the patient in left lateral decubitus using a 3.5–5 MHz transducer at a depth of 16 cm. ECG was recorded, and 3 consecutive cardiac cycles of each view were recorded during quiet breathing at 50–80 frames/sec. All patients were subjected to conventional transthoracic echocardiography & Speckle tracking echocardiography (STE). All measurements were taken following the American Society of Echocardiography (ASE) recommendations [3].
Left atrium (LA) dimension, left atrial volume index (LAVI) and left ventricular (LV) end-systolic and end-diastolic diameters were measured. LV ejection fraction was estimated by modified Simpson’s rule. Trans mitral pulsed-wave Doppler velocities were recorded from the apical four-chamber view with the Doppler sample placed between the tips of mitral leaflets. Early (E) and late (A) wave peak velocities, E/A ratio, E wave deceleration time (DT), and isovolumetric relaxation time (IVRT) were measured.
Tissue Doppler imaging was recorded during quiet breathing, at a rate of at least 105 frames/ sec. The myocardial early diastolic (e`), and late diastolic (a`) velocities were obtained at lateral & septal mitral annuli. The E/e` ratios were subsequently calculated. Left ventricular diastolic function was assessed and graded according to the recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography [4].
2D speckle tracking
Left atrial longitudinal strain analysis was obtained using automated speckle tracking software. The regions of interest (ROI) were generated automatically and LA endocardial border was manually adjusted when required.
LA phases definition and LAS values were measured from the LA longitudinal strain curve according to the European Association of Cardiovascular Imaging (EACVI)/American society of echocardiography (ASE) guidelines [5].
LAS analysis was calculated with the reference point set at the onset of the QRS complex of the superimposed ECG, two longitudinal deformation parameters are identified, positive peak atrial longitudinal strain at the end of the reservoir phase and a negative peak atrial contraction strain, before atrial contraction [6]. (Fig. 1.
LA strain rate was measured during the early ventricular filling phase. LA stiffness was calculated as the ratio of E/eʹ to LA reservoir strain x100 [7].
Global LV systolic strain (GLS) was evaluated, and the software automatically traced the contour of the endocardium at apical three, four and two-chamber views. 2D GLS was analysed during aortic valve closure.
Statistical analysis
Data are expressed as mean standard deviation (SD) for continuous variables, and categorical variables, as numbers & percentages. The student-t test and Chi-square test were used to compare variables between groups. To evaluate the diagnostic performance of left atrial strain and LV diastolic function parameters for the prediction of cardiac affection, a receiver-operating characteristic curve (ROC) was constructed. Multivariate Logistic regression analysis was adjusted for age, sex, and BMI to evaluate predictors of persistent dyspnoea post-COVID-19 infection. Data are presented as odds ratios (ORs) and 95% confidence intervals (CIs). A statistical test was significant when the P value was under 0.05. All P values are the results of 2-tailed tests. Statistical analyses were performed using SPSS software version 16.
Results
Between October, 2021, and October, 2022, 200 patients who recovered from the COVID-19 infection course were followed up routinely at our outpatient clinic for clinical and transthoracic echocardiographic evaluation. 137 patients did not match our inclusion criteria & were excluded while a total of 63 participants were included in our study. According to the presence of exertional dyspnoea & exercise intolerance, two groups (symptomatic and asymptomatic) were recruited.
We observed that dyspnoea & exercise intolerance prevalence was 31.7% post-COVID-19 in our cohort, while sinus tachycardia was present in 33% of them. No differences were observed in age, sex, BMI, BSA or basal CRP level in the acute stage between groups (Table 1).
Regarding conventional echocardiographic parameters between groups, we found significantly higher values of E/e` at the septal mitral annulus and IVRT in the symptomatic group, which did not rise to meet the criteria for diastolic impairment, but this shed the light on utilizing an advanced tool for further assessment (Table 2).
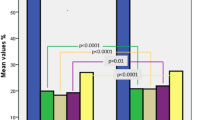
After measuring strain parameters using the available speckle tracking software, we found significantly impaired LAS parameters in the symptomatic group (LA reservoir, contraction & conduit strain, 22.7%, -6.6% & -16.1% versus 40%, -12% and, -27.5% at the asymptomatic group with P < 0.001). While the left ventricular systolic & diastolic global strain showed no significant difference between both groups as well as was the left atrial diastolic strain (p-value = 0.565, 0.187 & 0.069 respectively) (Table 3).
In the Multivariate model analysis (Table 4), after adjustment of age and sex, only LA reservoir strain and LA stiffness can independently predict the development of dyspnoea & exercise intolerance post-COVID-19 at OR of 0.72 (95% CI 0.59 to 0.896) and 1.3 (95% CI 1.034 to 1.68) respectively. These impaired parameters can point to LA myopathy and the subtle Left ventricular diastolic impairment which may explain the developed dyspnoea after recovery from COVID-19.
LA reservoir strain & LA stiffness at cut-off values of 30% & 24.5% respectively with a sensitivity of 90% and a specificity of 91% (95% CI 0.91–1), AUC of 0.959, P < 0.0001 showed the highest diagnostic performance in predicting persistent dyspnoea and exercise intolerance post-COVID-19. (Table 5; Fig. 2).
Discussion
It is known that the acute viral stressor of COVID-19 may trigger myocardial inflammation either via direct viral invasion in cardiac myocytes or indirect injuries caused by cytokine storm and inflammatory mediators which can potentially affect cardiac structure and function [8].
Vulnerable myocardium in patients with cardiometabolic risk factors can increase the likelihood of myocardial injury during the acute COVID-19 illness or post-recovery, nevertheless, studies evaluating the effect of COVID − 19 on previously healthy, non-vulnerable myocardium are scarce [9].
The background observation for our research was persistent symptoms post-COVID-19 usually start three months from the onset of COVID-19 and last several weeks after complete recovery. These symptoms cannot be explained by obvious pulmonary residual affection and their pathophysiology is not sufficiently evaluated in epidemiological studies [10].
We excluded patients with cardiometabolic risk factors & confounders affecting cardiac function, to assess the direct COVID-19 effect on the myocardium in our population.
Our results showed that 33% of post-COVID-19 patients developed unexplained exertional dyspnoea & exercise intolerance.
This was concordant with other studies that reported that persistent exertional dyspnoea one year after COVID-19 infection was present in more than a third of apparently healthy patients [11, 12]. While higher prevalence was reported by Arnold et al., where persistent breathlessness and excessive fatigue were found in (74%) of their studied patients [13].
Our results showed a statistically significant difference at septal E/e`& IVRT which were higher in the symptomatic group (8.4 & 70 ms) versus (6 & 56 ms) respectively, p < 0.000. Our results come in to agree with previously established studies reported that patients with COVID-19 infection had an increased average E/e′ ratio [14]. However, they found that the majority of patients (80%) did not have elevated LV filling pressure (E/e’≥14).
Also, Szekely et al. revealed a 16% incidence rate of LVDD despite a preserved LV systolic function in 90% of their patients [15].
A previous study used conventional DD (diastolic dysfunction) parameters, performed at 6–10 weeks after hospital discharge, in younger patients, without previous significant cardiovascular disease, they evidenced altered both LV-systolic & diastolic functions in 8.8% of subjects while 16.8% only showed diastolic dysfunction with preserved systolic performance [16].
Many studies are headed to use left ventricular speckle tracking in the detection of subclinical systolic & diastolic dysfunction in COVID-19 [17]. Our results showed normal LV systolic function evaluated by both the conventional volumetric method & global longitudinal strain, this is contrary to studies that showed reduced LV-systolic function in a third of their studied population, which may be due to the severity of COVID-19 infection or confounders affecting the myocardium in their population [18].
Based on the established role of left atrial strain analysis in the detection of LV diastolic dysfunction and its association with abnormal exercise haemodynamic in Heart failure with preserved ejection fraction (HFpEF) [19, 20], we used this tool to evaluate the possible subtle cardiac affection in our cohort. To the best of our knowledge, no African studies were done to ascertain the diastolic dysfunction burden amongst Covid-19 survivors at their intermediate-term utilizing the left atrial strain analysis.
We observed significantly impaired all LAS parameters in patients with persistent dyspnoea post COVID-19 recovery; LA Reservoir, contraction & conduit strain ( -22.7%, 6.6% & 16.1%) versus (-40%, 12% & 27%) with P < 0.000). Similar results showed that hospitalized COVID-19 patients have reduced LA function compared with COVID-19-negative controls and this dysfunction was more pronounced in COVID-19 patients who developed AF [21].
Also, left atrial stiffness (E/e` /LA reservoir strain) showed higher values among the symptomatic group (33.4% versus 16.6% at p < 0.000), which may give a clue for impaired LV lusitropy in this population. At multivariate analysis, we found that only LA reservoir strain and its derived non-invasive LA stiffness parameter were independently associated with the developed symptoms post-COVID-19 at OR of 0.72 (95% CI 0.59 to 0.896) and 1.3 (95% CI 1.034 to 1.68) respectively and are independent predictors for dyspnoea & exercise intolerance occurrence in Long COVID 19 syndrome.
Conclusion
The observations of our study suggest that LA strain and LA stiffness are early affected in patients with unexplained persistent dyspnoea and exercise intolerance post-COVID-19, and this could be attributed to impaired left ventricular diastolic function. Given the superiority of LA longitudinal strain over conventional diastolic parameters in the prediction of diastolic dysfunction, larger studies with invasive diagnostic modalities are needed to validate our results.
Limitation
Our results were not compared with an invasive hemodynamic assessment as a gold standard for elevated left ventricular filling pressure, also measurement of NTproBNP could add diagnostic role but, this was practically difficult due to the huge burden of covid-19 recovered patients.
It was a single-centre study with a relatively small sample size secondary to exclusion of numerous clinical confounders that impact the left atrial longitudinal strain.
References
Carfì A, Bernabei R, Landi F (2020) Group for the GAC-19 P-ACS. Persistent symptoms in patients after acute COVID-19. JAMA 324:603
Goërtz YMJ, Van Herck M, Delbressine JM, Vaes AW, Meys R, Machado FVC et al (2020) Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 6(4) Epub 2020 Oct 26
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39e14. https://doi.org/10.1016/j.echo.2014.10.003
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T et al (2016) Recommendations for the evaluation of left ventricular diastolic function by Echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314. doi: https://doi.org/10.1016/j.echo.2016.01.011
Badano LP, Kolias TJ, Muraru D et al (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging [published correction appears in Eur Heart J Cardiovasc Imaging 1;19(7):830–833]. Eur Heart J Cardiovasc Imaging. 2018;19(6):591–600. https://doi.org/10.1093/ehjci/jey042
Pathan F, D’Elia N, Nolan MT, Marwick TH, Negishi K (2017) Normal ranges of left atrial strain by Speckle-Tracking Echocardiography: a systematic review and Meta-analysis. J Am Soc Echocardiogr 30(1):59–70e8. https://doi.org/10.1016/j.echo.2016.09.007
Cameli M, Mandoli GE, Loiacono F et al (2016) Left atrial strain: a new parameter for assessment of left ventricular filling pressure. Heart Fail Rev 21:65–76
Tudoran M, Tudoran C, Lazureanu VE et al (2021) Alterations of left ventricular function persisting during post-acute COVID-19 in subjects without previously diagnosed cardiovascular pathology. J Pers 11:225. https://doi.org/10.3390/jpm11030225. )
Alwan NA, Johnson L (2021) Defining long COVID: going back to the start. Med (N Y) 2(5):501 Epub 2021 Mar 25
Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV (2021) WHO Clinical Case Definition Working Group on Post-COVID-19 Condition A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. doi: https://doi.org/10.1016/S1473-3099(21)00703-9
Luchian ML, Motoc A, Lochy S et al (2021) Subclinical myocardial dysfunction in patients with persistent Dyspnea One Year after COVID-19. Diagnostics (Basel) 12(1):57 Published 2021 Dec 28. https://doi.org/10.3390/diagnostics12010057
Froidure A, Mahsouli A, Liistro G, De Greef J, Belkhir L, Gerard L et al (2021) Integrative respiratory follow-up of severe COVID-19 reveals common functional and lung imaging sequelae. Respir Med 181:106383. doi: https://doi.org/10.1016/j.rmed.2021.106383
Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M et al (2021) Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax 76(4):399–401. doi: https://doi.org/10.1136/thoraxjnl-2020-216086Epub 2020 Dec 3. PMID: 33273026; PMCID: PMC7716340
Szekely Y, Lichter Y, Taieb P et al (2020) Spectrum of Cardiac Manifestations in COVID-19: a systematic echocardiographic study. Circulation 142(4):342–353. https://doi.org/10.1161/CIRCULATIONAHA.120.047971
Tudoran M, Tudoran C, Lazureanu VE, Marinescu AR, Pop GN, Pescariu AS et al (2021) Alterations of left ventricular function persisting during Post-Acute COVID-19 in subjects without previously diagnosed Cardiovascular Pathology. J Pers Med 11:225. https://doi.org/10.3390/jpm11030225
Freaney PM, Shah SJ, Khan SS (2020) COVID-19 and heart failure with preserved ejection fraction. JAMA 324:1499
Mahajan S, Kunal S, Shah B, Garg S, Palleda GM, Bansal A et al (2021) Left ventricular global longitudinal strain in COVID-19 recovered patients. Echocardiography 38(10):1722–1730
Telles F, Nanayakkara S, Evans S et al (2019) Impaired left atrial strain predicts abnormal exercise haemodynamics in heart failure with preserved ejection fraction. Eur J Heart Fail 21(4):495–505. https://doi.org/10.1002/ejhf.1399
Dal Canto E, Remmelzwaal S, van Ballegooijen AJ, Handoko ML, Heymans S, van Empel V et al (2022) Diagnostic value of echocardiographic markers for diastolic dysfunction and heart failure with preserved ejection fraction. Heart Fail Rev 27(1):207–218. doi: https://doi.org/10.1007/s10741-020-09985-1PMID: 32488580; PMCID: PMC8739319
Goerlich E, Minhas A, Gilotra N, Barth AS, Mukherjee M, Parziale A et al (2021) Left atrial function in patients with Coronavirus Disease 2019 and its Association with Incident Atrial Fibrillation/Flutter. J Am Soc Echocardiogr 34(10):1106–1109
Beyls C, Hermida A, Bohbot Y et al (2021) Automated left atrial strain analysis for predicting atrial fibrillation in severe COVID-19 pneumonia: a prospective study. Ann Intensive Care 11:168
Acknowledgements
The authors would like to thank the staff of the Academic Echocardiography Laboratory and all the patients for their participation in this study.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
ZeinElabdeen, S.G., Sherif, A., Kandil, N.T. et al. Left atrial longitudinal strain analysis in long Covid-19 syndrome. Int J Cardiovasc Imaging 39, 939–944 (2023). https://doi.org/10.1007/s10554-023-02801-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02801-5