Abstract
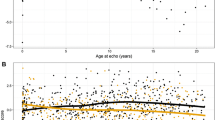
Purpose: Aortic dilation and valvar regurgitation can develop in transposition of the great arteries (TGA) after the arterial switch operation (ASO). Variation in aortic root rotational position affects flow dynamics in patients without congenital heart disease. The aim of this study was to assess neo-aortic root (neo-AoR) rotational position and its association with neo-AoR dilation, ascending aorta (AAo) dilation, and neo-aortic valvar regurgitation in TGA following ASO. Methods: Patients with TGA repaired by ASO who underwent cardiac magnetic resonance (CMR) were reviewed. Neo-AoR rotational angle, neo-AoR and AAo dimensions indexed (to height), indexed left ventricular end diastolic volume (LVEDVI), and neo-aortic valvar regurgitant fraction (RF) were obtained from CMR. Results: Among 36 patients, the median age at CMR was 17.1 years (12.3, 21.9). Neo-AoR rotational angle (range − 52 to + 78°) was clockwise ( ≥ + 15°) in 50%, counterclockwise (<-9°) in 25%, and central (-9 to + 14°) in 25% of patients. A quadratic term for neo-AoR rotational angle, indicating increasing extremes of counterclockwise and clockwise angles, was associated with neo-AoR dilation (R2 = 0.132, p = 0.03), AAo dilation (R2 = 0.160, p = 0.016), and LVEDVI (R2 = 0.20, p = 0.007). These associations remained statistically significant on multivariable analyses. Rotational angle was negatively associated with neo-aortic valvar RF on univariable (p < 0.05) and multivariable analyses (p < 0.02). Rotational angle was associated with smaller bilateral branch pulmonary arteries (p = 0.02). Conclusion: In patients with TGA after ASO, neo-AoR rotational position likely affects valvar function and hemodynamics, leading to a risk of neo-AoR and AAo dilation, aortic valvar incompetence, increasing left ventricular size, and smaller branch pulmonary arteries.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Williams WG, McCrindle BW, Ashburn DA, Jonas RA, Mavroudis C, Blackstone EH, and Congenital Heart Surgeon’s S (2003) Outcomes of 829 neonates with complete transposition of the great arteries 12–17 years after repair. Eur J Cardiothorac Surg 24(1);1–9; discussion 9–10. https://doi.org/10.1016/s1010-7940(03)00264-1
Fricke TA, d’Udekem Y, Richardson M, Thuys C, Dronavalli M, Ramsay JM, Wheaton G, Grigg LE, Brizard CP, Konstantinov IE (2012) Outcomes of the arterial switch operation for transposition of the great arteries: 25 years of experience. Ann Thorac Surg 94(1); 139–45. https://doi.org/10.1016/j.athoracsur.2012.03.019
Losay J, Touchot A, Serraf A, Litvinova A, Lambert V, Piot JD, Lacour-Gayet F, Capderou A, Planche C (2001) Late outcome after arterial switch operation for transposition of the great arteries. Circulation 104(12 Suppl 1):I121–I126
Khairy P, Clair M, Fernandes SM, Blume ED, Powell AJ, Newburger JW, Landzberg MJ, Mayer JE Jr (2013) Cardiovascular outcomes after the arterial switch operation for D-transposition of the great arteries. Circulation 127(3):331–339. https://doi.org/10.1161/CIRCULATIONAHA.112.135046
Tobler D, Williams WG, Jegatheeswaran A, Van Arsdell GS, McCrindle BW, Greutmann M, Oechslin EN, Silversides CK (2010) Cardiac outcomes in young adult survivors of the arterial switch operation for transposition of the great arteries. J Am Coll Cardiol 56(1):58–64. https://doi.org/10.1016/j.jacc.2010.03.031
Legendre A, Losay J, Touchot-Kone A, Serraf A, Belli E, Piot JD, Lambert V, Capderou A, Planche C (2003) Coronary events after arterial switch operation for transposition of the great arteries. Circulation 108(Suppl 1). https://doi.org/10.1161/01.cir.0000087902.67220.2b. ;II186-90
Co-Vu JG, Ginde S, Bartz PJ, Frommelt PC, Tweddell JS, Earing MG (2013) Long-term outcomes of the neoaorta after arterial switch operation for transposition of the great arteries. Ann Thorac Surg 95(5):1654–1659. https://doi.org/10.1016/j.athoracsur.2012.10.081
van der Palen RLF, van der Bom T, Dekker A, Tsonaka R, van Geloven N, Kuipers IM, Konings TC, Rammeloo LAJ, Ten Harkel ADJ, Jongbloed MRM, Koolbergen DR, Mulder BJM, Hazekamp MG, Blom NA (2019) Progression of aortic root dilatation and aortic valve regurgitation after the arterial switch operation. Heart 105(22):1732–1740. https://doi.org/10.1136/heartjnl-2019-315157
Shepard CW, Germanakis I, White MT, Powell AJ, Co-Vu J, Geva T (2016) Cardiovascular magnetic resonance findings late after the arterial switch operation. Circ Cardiovasc Imaging 9(9). https://doi.org/10.1161/CIRCIMAGING.116.004618
Vandekerckhove KD, Blom NA, Lalezari S, Koolbergen DR, Rijlaarsdam ME, Hazekamp MG (2009) Long-term follow-up of arterial switch operation with an emphasis on function and dimensions of left ventricle and aorta. Eur J Cardiothorac Surg 35(4);582-7; discussion 587-8. https://doi.org/10.1016/j.ejcts.2008.12.034
Schwartz ML, Gauvreau K, del Nido P, Mayer JE, Colan SD (2004) Long-term predictors of aortic root dilation and aortic regurgitation after arterial switch operation. Circulation 110(11 Suppl 1);II128-32. https://doi.org/10.1161/01.CIR.0000138392.68841.d3
McMahon CJ, Ravekes WJ, Smith EO, Denfield SW, Pignatelli RH, Altman CA, Ayres NA (2004) Risk factors for neo-aortic root enlargement and aortic regurgitation following arterial switch operation. Pediatr Cardiol 25(4); 329–35. https://doi.org/10.1007/s00246-003-0483-6
Agnoletti G, Ou P, Celermajer DS, Boudjemline Y, Marini D, Bonnet D, Aggoun Y (2008) Acute angulation of the aortic arch predisposes a patient to ascending aortic dilatation and aortic regurgitation late after the arterial switch operation for transposition of the great arteries. J Thorac Cardiovasc Surg 135(3); 568–72. https://doi.org/10.1016/j.jtcvs.2007.10.020
Martins D, Khraiche D, Legendre A, Boddaert N, Raisky O, Bonnet D, Raimondi F (2019) Aortic angle is associated with neo-aortic root dilatation and regurgitation following arterial switch operation. Int J Cardiol 280:53–56. https://doi.org/10.1016/j.ijcard.2019.01.042
Tretter JT, Mori S, Saremi F, Chikkabyrappa S, Thomas K, Bu F, Loomba RS, Alsaied T, Spicer DE, Anderson RH (2018) Variations in rotation of the aortic root and membranous septum with implications for transcatheter valve implantation. Heart 104(12):999–1005. https://doi.org/10.1136/heartjnl-2017-312390
Amofa D, Mori S, Toh H, Ta HT, Du Plessis M, Davis N, Izawa Y, Spicer DE, Anderson RH, Tretter JT (2019) The rotational position of the aortic root related to its underlying ventricular support. Clin Anat 32(8):1107–1117. https://doi.org/10.1002/ca.23462
Saremi F, Cen S, Tayari N, Alizadeh H, Emami A, Lin L, Fleischman F (2017) A correlative study of aortic valve rotation angle and thoracic aortic sizes using ECG gated CT angiography. Eur J Radiol 89:60–66. https://doi.org/10.1016/j.ejrad.2017.01.009
Powell SK, Almeneisi H, Alsaied T, Shikany A, Riley L, Miller E, Belonis A, Weaver KN, Brown N, Mori S, Tretter JT (2021) Rotational position of the aortic Root is Associated with increased aortic dimensions in Marfan and Loeys-Dietz Syndrome. https://doi.org/10.1007/s00246-021-02594-1. Pediatr Cardiol
Cohen MS, Eidem BW, Cetta F, Fogel MA, Frommelt PC, Ganame J, Han BK, Kimball TR, Johnson RK, Mertens L, Paridon SM, Powell AJ, Lopez L (2016) Multimodality Imaging Guidelines of patients with transposition of the great arteries: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular magnetic resonance and the Society of Cardiovascular computed Tomography. J Am Soc Echocardiogr 29(7):571–621. https://doi.org/10.1016/j.echo.2016.04.002
Tretter JT, Mori S (2019) Two-dimensional imaging of a Complex Three-Dimensional structure: measurements of aortic Root Dimensions. J Am Soc Echocardiogr 32(6):792–794. https://doi.org/10.1016/j.echo.2019.02.001
Zafar MA, Li Y, Rizzo JA, Charilaou P, Saeyeldin A, Velasquez CA, Mansour AM, Bin Mahmood SU, Ma WG, Brownstein AJ, Tranquilli M, Dumfarth J, Theodoropoulos P, Thombre K, Tanweer M, Erben Y, Peterss S, Ziganshin BA, Elefteriades JA (2018) Height alone, rather than body surface area, suffices for risk estimation in ascending aortic aneurysm. J Thorac Cardiovasc Surg 155(5):1938–1950. https://doi.org/10.1016/j.jtcvs.2017.10.140
van der Bom T, van der Palen RL, Bouma BJ, van Veldhuisen SL, Vliegen HW, Konings TC, Zwinderman AH, Blom NA, Koolbergen DR, Hazekamp MG, Mulder BJ (2014) Persistent neo-aortic growth during adulthood in patients after an arterial switch operation. Heart 100(17):1360–1365. https://doi.org/10.1136/heartjnl-2014-305702
Sundstrom E, Jonnagiri R, Gutmark-Little I, Gutmark E, Critser P, Taylor MD, Tretter JT (2020) Effects of normal variation in the Rotational position of the aortic Root on Hemodynamics and tissue biomechanics of the thoracic aorta. Cardiovasc Eng Technol 11(1):47–58. https://doi.org/10.1007/s13239-019-00441-2
Toh H, Mori S, Tretter JT, Izawa Y, Shimoyama S, Suzuki M, Takahashi Y, Tsuda D, Toba T, Fujiwara S, Hirata KI, Anderson RH (2020) Living anatomy of the ventricular myocardial crescents supporting the coronary aortic sinuses. Semin Thorac Cardiovasc Surg 32(2):230–241. https://doi.org/10.1053/j.semtcvs.2020.01.001
Marino BS, Wernovsky G, McElhinney DB, Jawad A, Kreb DL, Mantel SF, van der Woerd WL, Robbers-Visser D, Novello R, Gaynor JW, Spray TL, Cohen MS (2006) Neo-aortic valvar function after the arterial switch. Cardiol Young 16(5):481–489. https://doi.org/10.1017/S1047951106000953
Grotenhuis HB, Cifra B, Mertens LL, Riessenkampff E, Manlhiot C, Seed M, Yoo SJ, Grosse-Wortmann L (2019) Left ventricular remodelling in long-term survivors after the arterial switch operation for transposition of the great arteries. Eur Heart J Cardiovasc Imaging 20(1):101–107. https://doi.org/10.1093/ehjci/jey072
Kuebler JD, Chen MH, Alexander ME, Rhodes J (2016) Exercise Performance in Patients with D-Loop Transposition of the great arteries after arterial switch operation: Long-Term Outcomes and Longitudinal Assessment. Pediatr Cardiol 37(2):283–289. https://doi.org/10.1007/s00246-015-1275-5
Raju V, Burkhart HM, Durham LA 3, Eidem BW, Phillips SD, Li Z, Schaff HV, Dearani JA (2013) Reoperation after arterial switch: a 27-year experience. Ann Thorac Surg 95(6);2105-12; discussion 2112-3. https://doi.org/10.1016/j.athoracsur.2013.02.040
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by S.T, J.T, and S.L. Statistical analysis was performed by Z.G. and N.O. The first draft of the manuscript was written by S.T. Figures were prepared by S.T. and Z.G. All authors reviewed the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This research study was conducted retrospectively from data obtained from clinical purposes. This study was approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center.
Consent to participate
The requirement for informed consent was waived due to the retrospective nature of the study.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tseng, S.Y., Tretter, J.T., Gao, Z. et al. Aortic root rotational position associates with aortic valvar incompetence and aortic dilation after arterial switch operation for transposition of the great arteries. Int J Cardiovasc Imaging 39, 1013–1021 (2023). https://doi.org/10.1007/s10554-023-02794-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02794-1