Abstract
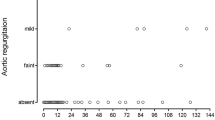
Proximal aortic enlargement is associated with an increased risk of heart failure and all-cause mortality. Recently, aortic root dilatation (ARD) was reported in postoperative patients with ventricular septal defects (VSDs). However, the impact of ARD on left ventricular (LV) function in postoperative VSD patients remains unclear. Thus, the aim of this study was to investigate the effect of ARD on LV function in patients with postoperative VSD. One hundred and thirty-five patients (> 15 years of age) with surgically repaired isolated ventricular defects and who underwent transthoracic echocardiography in our institution between 2009 and 2013 were identified. ARD was defined as an observed aortic root diameter/body surface area > 2.1 cm/m2. The propensity score estimating the probability of having ARD adjusted for anatomical and clinical characteristics was calculated. Forty-four patients (32.6%) had ARD. In unadjusted analyses, right ventricular systolic pressure, Tei index, and E/e’ were significantly (p < 0.05) higher in patients with ARD than in those without ARD (31.3 ± 7.5 vs. 35.4 ± 13.7 mmHg, 0.32 ± 0.10 vs. 0.44 ± 0.15, and 7.1 ± 1.7 vs. 9.5 ± 2.9, respectively). In the propensity score-adjusted analysis, significant differences in the Tei index and E/e’ were confirmed between the two groups (Tei index difference: 0.11, 95% confidence interval 0.05–0.17; E/e’ difference: 2.4, 95% confidence interval 1.3–3.5). However, there were no differences in the other echocardiographic measurements. The presence of ARD in patients with postoperative VSD was significantly associated with LV diastolic dysfunction. Thus, surgically repaired VSD patients require careful screening for aortic enlargement and LV function.

Similar content being viewed by others
References
Menting ME, Cuypers JA, Opic P, Utens EM, Witsenburg M, van den Bosch AE, van Domburg RT, Meijboom FJ, Boersma E, Bogers AJ, Roos-Hesselink JW (2015) The unnatural history of the ventricular septal defect: outcome up to 40 years after surgical closure. J Am Coll Cardiol 65:1941–1951
Nederend I, de Geus EJC, Blom NA, Ten Harkel ADJ (2018) Long-term follow-up after ventricular septal defect repair in children: cardiac autonomic control, cardiac function and exercise capacity. Eur J Cardiothorac Surg 53:1082–1088
Karonis T, Scognamiglio G, Babu-Narayan SV, Montanaro C, Uebing A, Diller GP, Alonso-Gonzalez R, Swan L, Dimopoulos K, Gatzoulis MA, Li W (2016) Clinical course and potential complications of small ventricular septal defects in adulthood: late development of left ventricular dysfunction justifies lifelong care. Int J Cardiol 208:102–106
Roos-Hesselink JW, Meijboom FJ, Spitaels SE, Van Domburg R, Van Rijen EH, Utens EM, Bogers AJ, Simoons ML (2004) Outcome of patients after surgical closure of ventricular septal defect at young age: longitudinal follow-up of 22–34 years. Eur Heart J 25:1057–1062
Lam CS, Gona P, Larson MG, Aragam J, Lee DS, Mitchell GF, Levy D, Cheng S, Benjamin EJ, Vasan RS (2013) Aortic root remodeling and risk of heart failure in the Framingham Heart study. JACC Heart failure 1:79–83
Kamimura D, Suzuki T, Musani SK, Hall ME, Samdarshi TE, Correa A, Fox ER (2017) Increased proximal aortic diameter is associated with risk of cardiovascular events and all-cause mortality in blacks The Jackson Heart Study. J Am Heart Assoc. https://doi.org/10.1161/jaha.116.005005
Cuspidi C, Facchetti R, Bombelli M, Re A, Cairoa M, Sala C, Tadic M, Grassi G, Mancia G (2014) Aortic root diameter and risk of cardiovascular events in a general population: data from the PAMELA study. J Hypertens 32:1879–1887
Yetman AT, Graham T (2009) The dilated aorta in patients with congenital cardiac defects. J Am Coll Cardiol 53:461–467
Francois K (2015) Aortopathy associated with congenital heart disease: a current literature review. Ann Pediatr Cardiol 8:25–36
Zanjani KS, Niwa K (2013) Aortic dilatation and aortopathy in congenital heart diseases. J Cardiol 61:16–21
Saito C, Fukushima N, Fukushima K, Matsumura G, Ashihara K, Hagiwara N (2017) Factors associated with aortic root dilatation after surgically repaired ventricular septal defect. Echocardiography 34:1203–1209
Gabriels C, Van De Bruaene A, Helsen F, Moons P, Van Deyk K, Troost E, Meyns B, Gewillig M, Budts W (2016) Recall of patients discharged from follow-up after repair of isolated congenital shunt lesions. Int J Cardiol 221:314–320
Fukushima K, Fukushima N, Ejima K, Kato K, Sato Y, Uematsu S, Arai K, Manaka T, Takagi A, Ashihara K, Shoda M, Hagiwara N (2015) Left atrial appendage flow velocity and time from P-wave onset to tissue Doppler-derived A’ predict atrial fibrillation recurrence after radiofrequency catheter ablation. Echocardiography 32:1101–1108
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39.e14
Evangelista A, Flachskampf FA, Erbel R, Antonini-Canterin F, Vlachopoulos C, Rocchi G, Sicari R, Nihoyannopoulos P, Zamorano J, Pepi M, Breithardt OA, Plonska-Gosciniak E, European Association of Echocardiography, Document Reviewers (2010) Echocardiography in aortic diseases: EAE recommendations for clinical practice. Eur J Echocardiogr 11:645–658
Fukushima K, Fukushima N, Kato K, Ejima K, Sato H, Fukushima K, Saito C, Hayashi K, Arai K, Manaka T, Ashihara K, Shoda M, Hagiwara N (2016) Correlation between left atrial appendage morphology and flow velocity in patients with paroxysmal atrial fibrillation. Eur Heart J Cardiovasc Imaging 17:59–66
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 26:357–366
Tissera G, Piskorz D, Citta L, Citta N, Citta P, Keller L, Bongarzoni L, Mata L, Tommasi A (2016) Morphologic and functional heart abnormalities associated to high modified Tei index in hypertensive patients. High Blood Press Cardiovasc Prev 23:373–380
Chobanian AV (2017) Guidelines for the management of hypertension. Med Clin North Am 101:219–227
Seino Y, Nanjo K, Tajima N, Kadowaki T, Kashiwagi A, Araki E, Ito C, Inagaki N, Iwamoto Y, Kasuga M, Hanafusa T, Haneda M, Ueki K (2010) Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig 1:212–228
Kinoshita M, Yokote K, Arai H, Iida M, Ishigaki Y, Ishibashi S, Umemoto S, Egusa G, Ohmura H, Okamura T, Kihara S, Koba S, Saito I, Shoji T, Daida H, Tsukamoto K, Deguchi J, Dohi S, Dobashi K, Hamaguchi H, Hara M, Hiro T, Biro S, Fujioka Y, Maruyama C, Miyamoto Y, Murakami Y, Yokode M, Yoshida H, Rakugi H, Wakatsuki A, Yamashita S (2017) Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases. J Atheroscler Thromb 25:846–984
Covella M, Milan A, Totaro S, Cuspidi C, Re A, Rabbia F, Veglio F (2014) Echocardiographic aortic root dilatation in hypertensive patients: a systematic review and meta-analysis. J Hypertens 32:1928–1935
Nwabuo CC, Moreira HT, Vasconcellos HD, Ambale-Venkatesh B, Yoneyama K, Ohyama Y, Sharma RK, Armstrong AC, Ostovaneh MR, Lewis CE, Liu K, Schreiner PJ, Ogunyankin KO, Gidding SS, Lima JAC (2017) Association of aortic root dilation from early adulthood to middle age with cardiac structure and function: the CARDIA study. J Am Soc Echocardiogr 30:1172–1179
Masugata H, Senda S, Murao K, Okuyama H, Inukai M, Hosomi N, Iwado Y, Noma T, Kohno M, Himoto T, Goda F (2011) Aortic root dilatation as a marker of subclinical left ventricular diastolic dysfunction in patients with cardiovascular risk factors. J Int Med Res 39:64–70
Milan A, Avenatti E, Tosello F, Iannaccone A, Leone D, Magnino C, Veglio F (2013) Aortic root dilatation in essential hypertension: prevalence according to new reference values. J Hypertens 31:1189–1195
Devereux RB, de Simone G, Arnett DK, Best LG, Boerwinkle E, Howard BV, Kitzman D, Lee ET, Mosley TH Jr, Weder A, Roman MJ (2012) Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons >/=15 years of age. Am J Cardiol 110:1189–1194
Niwa K (2013) Aortopathy in congenital heart disease in adults: aortic dilatation with decreased aortic elasticity that impacts negatively on left ventricular function. Korean Circ J 43:215–220
Shiina Y, Murakami T, Kawamatsu N, Niwa K (2017) Aortopathy in adults with tetralogy of Fallot has a negative impact on the left ventricle. Int J Cardiol 228:380–384
Schlatmann TJ, Becker AE (1977) Histologic changes in the normal aging aorta: implications for dissecting aortic aneurysm. Am J Cardiol 39:13–20
Namba T, Masaki N, Matsuo Y, Sato A, Kimura T, Horii S, Yasuda R, Yada H, Kawamura A, Takase B, Adachi T (2016) Arterial stiffness is significantly associated with left ventricular diastolic dysfunction in patients with cardiovascular disease. Int Heart J 57:729–735
Mori S, Yamashita T, Takaya T, Kinugasa M, Takamine S, Shigeru M, Ito T, Fujiwara S, Nishii T, Kono AK, Hirata K (2014) Association between the rotation and three-dimensional tortuosity of the proximal ascending aorta. Clin Anat 27:1200–1211
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:107–133
Gnakamene JB, Safar ME, Levy BI, Escoubet B (2018) Left ventricular torsion associated with aortic stiffness in hypertension. J Am Heart Assoc. https://doi.org/10.1161/jaha.117.007427
Hoffman JI, Mahajan A, Coghlan C, Saleh S, Buckberg GD (2008) A new look at diastole. Heart Fail Clin 4:347–360
Matsuhisa H, Yoshimura N, Higuma T, Misaki T, Onuma Y, Ichida F, Oshima Y, Okita Y (2013) Ventricular septal dysfunction after surgical closure of multiple ventricular septal defects. Ann Thorac Surg 96:891–897
Milan A, Tosello F, Naso D, Avenatti E, Leone D, Magnino C, Veglio F (2013) Ascending aortic dilatation, arterial stiffness and cardiac organ damage in essential hypertension. J Hypertens 31:109–116
Wan SH, Vogel MW, Chen HH (2014) Pre-clinical diastolic dysfunction. J Am Coll Cardiol 63:407–416
Kamimura D, Uchino K, Ogawa H, Shimizu M, Shigemasa T, Morita Y, Kimura K, Umemura S (2014) Small proximal aortic diameter is associated with higher central pulse pressure and poor outcome in patients with congestive heart failure. Hypertens Res 37:57–63
de Simone G, Roman MJ, De Marco M, Bella JN, Izzo R, Lee ET, Devereux RB (2015) Hemodynamic correlates of abnormal aortic root dimension in an adult population: the strong heart study. J Am Heart Assoc 4:e002309
Forte A, Galderisi U, Cipollaro M, De Feo M, Della Corte A (2016) Epigenetic regulation of TGF-beta1 signaling in dilative aortopathy of the thoracic ascending aorta. Clin Sci (Lond) 130:1389–1405
Acknowledgements
The authors thank Dr. Shinya Hatakeyama for assistance with data collection, Dr. Goki Matsumura for advice regarding the manuscript, and Edanz Group (http://www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fukushima, N., Fukushima, K., Sato, H. et al. Association of aortic root dilatation with left ventricular function in patients with postoperative ventricular septal defect. Heart Vessels 34, 1491–1498 (2019). https://doi.org/10.1007/s00380-019-01372-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01372-7