Abstract
Purpose
To evaluate the possible influence of chest wall conformation on myocardial strain parameters in a cohort of mitral valve prolapse (MVP) patients with and without mitral annular disjunction (MAD).
Methods
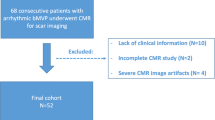
All consecutive middle-aged patients with MVP referred to our Outpatient Cardiology Clinic for performing two-dimensional (2D) transthoracic echocardiography (TTE) as part of work up for primary cardiovascular prevention between March 2018 and May 2022, were included into the study. All patients underwent clinic visit, physical examination, modified Haller index (MHI) assessment (the ratio of chest transverse diameter over the distance between sternum and spine) and conventional 2D-TTE implemented with speckle tracking analysis of left ventricular (LV) global longitudinal strain (GLS) and global circumferential strain (GCS). Independent predictors of MAD presence on 2D-TTE were assessed.
Results
A total of 93 MVP patients (54.2 ± 16.4 yrs, 50.5% females) were prospectively analyzed. On 2D-TTE, 34.4% of MVP patients had MAD (7.3 ± 2.0 mm), whereas 65.6% did not. Compared to patients without MAD, those with MAD had: 1) significantly shorter antero-posterior (A-P) thoracic diameter (13.5 ± 1.2 vs 14.8 ± 1.3 cm, p < 0.001); 2) significantly smaller cardiac chambers dimensions; 3) significantly increased prevalence of classic MVP (84.3 vs 44.3%, p < 0.001); 4) significantly impaired LV-GLS (-17.2 ± 1.4 vs -19.4 ± 3.0%, p < 0.001) and LV-GCS (-16.3 ± 4.1 vs -20.4 ± 4.9, p < 0.001), despite similar LV ejection fraction (63.7 ± 4.2 vs 63.0 ± 3.9%, p = 0.42). A-P thoracic diameter (OR 0.25, 95%CI 0.10–0.82), classic MVP (OR 3.90, 95%CI 1.32–11.5) and mitral annular end-systolic A-P diameter (OR 2.76, 95%CI 1.54–4.92) were the main independent predictors of MAD. An A-P thoracic diameter ≤ 13.5 cm had 59% sensitivity and 84% specificity for predicting MAD presence (AUC = 0.81). In addition, MAD distance was strongly influenced by A-P thoracic diameter (r = − 0.96) and MHI (r = 0.87), but not by L-L thoracic diameter (r = 0.23). Finally, a strong inverse correlation between MHI and both LV-GLS and LV-GCS was demonstrated in MAD patients (r = − 0.94 and − 0.92, respectively), but not in those without (r = − 0.51 and − 0.50, respectively).
Conclusions
A narrow A-P thoracic diameter is strongly associated with MAD presence and is a major determinant of the impairment in myocardial strain parameters in MAD patients, in both longitudinal and circumferential directions.






Similar content being viewed by others
Abbreviations
- 2D:
-
Two-dimensional
- A-P:
-
Antero-posterior
- AUC:
-
Area under the curve
- CIs:
-
Confidence intervals
- CXR:
-
Chest-X ray
- ECG:
-
Electrocardiogram
- EROA:
-
Effective regurgitant orifice area
- GCS:
-
Global circumferential strain
- GLS:
-
Global longitudinal strain
- ICC:
-
Intraclass correlation coefficient
- LAVi:
-
Left atrial volume index
- L-L:
-
Latero-lateral
- LV:
-
Left ventricular
- LVEDDi:
-
Left ventricular end-diastolic diameter index
- LVEF:
-
Left ventricular ejection fraction
- LVMi:
-
Left ventricular mass index
- MAD:
-
Mitral annular disjunction
- MHI:
-
Modified Haller index
- MR:
-
Mitral regurgitation
- MRI:
-
Magnetic resonance imaging
- MVP:
-
Mitral valve prolapse
- NS-STT:
-
Nonspecific ST-segment and T-wave
- NSVT:
-
Nonsustained ventricular tachycardia
- PM:
-
Papillary muscles
- ROC:
-
Receiver operating characteristics
- SPAP:
-
Systolic pulmonary artery pressure
- SD:
-
Standard deviation
- SPB:
-
Supraventricular premature beats
- STE:
-
Speckle tracking echocardiography
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TTE:
-
Transthoracic echocardiography
- VPB:
-
Ventricular premature beats
References
Putnam AJ, Kebed K, Mor-Avi V et al (2020) Prevalence of mitral annular disjunction in patients with mitral valve prolapse and severe regurgitation. Int J Cardiovasc Imaging 36:1363–1370
Essayagh B, Sabbag A, Antoine C et al (2021) The Mitral Annular Disjunction of Mitral Valve Prolapse: Presentation and Outcome. JACC Cardiovasc Imaging 14:2073–2087
Hutchins GM, Moore GW, Skoog DK (1986) The association of floppy mitral valve with disjunction of the mitral annulus fibrosus. N Engl J Med 314:535–540
Angelini A, Ho SY, Anderson RH, Becker AE, Davies MJ (1988) Disjunction of the mitral annulus in floppy mitral valve. N Engl J Med 318:188–189
Konda T, Tani T, Suganuma N et al (2017) The analysis of mitral annular disjunction detected by echocardiography and comparison with previously reported pathological data. J Echocardiogr 15:176–185
Carmo P, Andrade MJ, Aguiar C, Rodrigues R, Gouveia R, Silva JA (2010) Mitral annular disjunction in myxomatous mitral valve disease: a relevant abnormality recognizable by transthoracic echocardiography. Cardiovasc Ultrasound 8:53
Konda T, Tani T, Suganuma N et al (2020) Mitral annular disjunction in patients with primary severe mitral regurgitation and mitral valve prolapse. Echocardiography 37:1716–1722
Basso C, Perazzolo Marra M, Rizzo S et al (2015) Arrhythmic Mitral Valve Prolapse and Sudden Cardiac Death. Circulation 132:556–566
Nordhues BD, Siontis KC, Scott CG et al (2016) Bileaflet Mitral Valve Prolapse and Risk of Ventricular Dysrhythmias and Death. J Cardiovasc Electrophysiol 27:463–468
Perazzolo Marra M, Basso C, De Lazzari M et al (2016) Morphofunctional Abnormalities of Mitral Annulus and Arrhythmic Mitral Valve Prolapse. Circ Cardiovasc Imaging 9:e005030
Bennett S, Thamman R, Griffiths T et al (2019) Mitral annular disjunction: A systematic review of the literature. Echocardiography 36:1549–1558
Lee AP, Jin CN, Fan Y, Wong RHL, Underwood MJ, Wan S (2017) Functional Implication of Mitral Annular Disjunction in Mitral Valve Prolapse: A Quantitative Dynamic 3D Echocardiographic Study. JACC Cardiovasc Imaging 10:1424–1433
Wang TKM, Kwon DH, Abou-Hassan O et al (2021) Strain evaluation for mitral annular disjunction by echocardiography and magnetic resonance imaging: A case-control study. Int J Cardiol 334:154–156
Sonaglioni A, Baravelli M, Vincenti A et al (2018) A New modified anthropometric haller index obtained without radiological exposure. Int J Cardiovasc Imaging 34:1505–1509
Faletra FF, Leo LA, Paiocchi VL et al (2019) Anatomy of mitral annulus insights from non-invasive imaging techniques. Eur Heart J Cardiovasc Imaging 20:843–857
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1-39.e14
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Freed LA, Benjamin EJ, Levy D et al (2002) Mitral valve prolapse in the general population: the benign nature of echocardiographic features in the Framingham Heart Study. J Am Coll Cardiol 40:1298–1304
Parwani P, Avierinos JF, Levine RA, Delling FN (2017) Mitral Valve Prolapse: Multimodality Imaging and Genetic Insights. Prog Cardiovasc Dis 60:361–369
Tagarakis GI, Karantzis I, Tsolaki F, Stylianakis GE, Daskalopoulos ME, Tsilimingas NB (2012) Classic and non-classic forms of mitral valve prolapse. Anadolu Kardiyol Derg 12:2–4
Levine RA, Hagége AA, Judge DP et al (2015) Mitral valve disease–morphology and mechanisms. Nat Rev Cardiol 12:689–710
Pu M, Prior DL, Fan X et al (2001) Calculation of mitral regurgitant orifice area with use of a simplified proximal convergence method: initial clinical application. J Am Soc Echocardiogr 14:180–185
Zoghbi WA, Enriquez-Sarano M, Foster E et al (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 16:777–802
Nishimura RA, Otto CM, Bonow RO et al (2017) 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 135:e1159–e1195
Eriksson MJ, Bitkover CY, Omran AS et al (2005) Mitral annular disjunction in advanced myxomatous mitral valve disease: echocardiographic detection and surgical correction. J Am Soc Echocardiogr 18:1014–1022
Pavon AG, Monney P, Schwitter J (2021) Mitral Valve Prolapse, Arrhythmias, and Sudden Cardiac Death: The Role of Multimodality Imaging to Detect High-Risk Features. Diagnostics (Basel) 11:683
Galderisi M, Cosyns B, Edvardsen T et al (2017) Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 18:1301–1310
Sugimoto T, Dulgheru R, Bernard A et al (2017) Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging 18:833–840
Salomon J, Shah PM, Heinle RA (1975) Thoracic skeletal abnormalities in idiopathic mitral valve prolapse. Am J Cardiol 36:32–36
Kelly RE, Goretsky MJ, Obermeyer R et al (2010) Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg 252:1072–1081
Wright CD (2017) Straight back syndrome. Thorac Surg Clin 27:133–137
Sidden CR, Katz ME, Swoveland BC, Nuss D (2001) Radiologic considerations in patients undergoing the Nuss procedure for correction of pectus excavatum. Pediatr Radiol 31:429–434
Sonaglioni A, Nicolosi GL, Granato A, Lombardo M, Anzà C, Ambrosio G (2021) Reduced Myocardial Strain Parameters in Subjects With Pectus Excavatum: Impaired Myocardial Function or Methodological Limitations Due to Chest Deformity? Semin Thorac Cardiovasc Surg 33:251–262
Sonaglioni A, Nicolosi GL, Lombardo M, Gensini GF, Ambrosio G (2021) Influence of chest conformation on myocardial strain parameters in healthy subjects with mitral valve prolapse. Int J Cardiovasc Imaging 37:1009–1022
Lollert A, Emrich T, Eichstädt J et al (2018) Differences in myocardial strain between pectus excavatum patients and healthy subjects assessed by cardiac MRI: a pilot study. Eur Radiol 28:1276–1284
Chao CJ, Jaroszewski D, Gotway M et al (2018) Effects of Pectus Excavatum Repair on Right and Left Ventricular Strain. Ann Thorac Surg 105:294–301
Truong VT, Li CY, Brown RL et al (2017) Occult RV systolic dysfunction detected by CMR derived RV circumferential strain in patients with pectus excavatum. PLoS ONE 12:e0189128
Sonaglioni A, Esposito V, Caruso C et al (2021) Chest conformation spuriously influences strain parameters of myocardial contractile function in healthy pregnant women. J Cardiovasc Med (Hagerstown) 22:767–779
Sonaglioni A, Nicolosi GL, Braga M, Villa MC, Migliori C, Lombardo M (2021) Does chest wall conformation influence myocardial strain parameters in infants with pectus excavatum? J Clin Ultrasound 49:918–928
Sonaglioni A, Caminati A, Nicolosi GL, Lombardo M, Harari S (2022) Influence of chest wall conformation on spirometry parameters and outcome in mild-to-moderate idiopathic pulmonary fibrosis. Intern Emerg Med 17:989–999
Mignot A, Donal E, Zaroui A et al (2010) Global longitudinal strain as a major predictor of cardiac events in patients with depressed left ventricular function: a multicenter study. J Am Soc Echocardiogr 23:1019–1024
Dahl JS, Videbæk L, Poulsen MK, Rudbæk TR, Pellikka PA, Møller JE (2012) Global strain in severe aortic valve stenosis: relation to clinical outcome after aortic valve replacement. Circ Cardiovasc Imaging 5:613–620
Bertini M, Ng AC, Antoni ML et al (2012) Global longitudinal strain predicts long-term survival in patients with chronic ischemic cardiomyopathy. Circ Cardiovasc Imaging 5:383–391
Levy PT, El-Khuffash A, Patel MD et al (2017) Maturational Patterns of Systolic Ventricular Deformation Mechanics by Two-Dimensional Speckle-Tracking Echocardiography in Preterm Infants over the First Year of Age. J Am Soc Echocardiogr 30:685-698.e1
Bijnens BH, Cikes M, Claus P, Sutherland GR (2009) Velocity and deformation imaging for the assessment of myocardial dysfunction. Eur J Echocardiogr 10:216–226
Fukuda S, Song JK, Mahara K et al (2016) Basal Left Ventricular Dilatation and Reduced Contraction in Patients With Mitral Valve Prolapse Can Be Secondary to Annular Dilatation: Preoperative and Postoperative Speckle-Tracking Echocardiographic Study on Left Ventricle and Mitral Valve Annulus Interaction. Circ Cardiovasc Imaging 9:e005113
Nutter DO, Wickliffe C, Gilbert CA, Moody C, King SB 3rd (1975) The pathophysiology of idiopathic mitral valve prolapse. Circulation 52:297–305
van Wijngaarden SE, Abou R, Hiemstra YL, Ajmone Marsan N, Bax JJ, Delgado V (2018) Regional Left Ventricular Myocardial Mechanics in Degenerative Myxomatous Mitral Valve Disease: A Comparison Between Fibroelastic Deficiency and Barlow’s Disease. JACC Cardiovasc Imaging 11:1362–1364
Muthukumar L, Jahangir A, Jan MF, Perez Moreno AC, Khandheria BK, Tajik AJ (2020) Association Between Malignant Mitral Valve Prolapse and Sudden Cardiac Death: A Review. JAMA Cardiol 5:1053–1061
Mantegazza V, Tamborini G, Muratori M et al (2019) Mitral Annular Disjunction in a Large Cohort of Patients With Mitral Valve Prolapse and Significant Regurgitation. JACC Cardiovasc Imaging 12:2278–2280
Wunderlich NC, Ho SY, Flint N, Siegel RJ (2021) Myxomatous Mitral Valve Disease with Mitral Valve Prolapse and Mitral Annular Disjunction: Clinical and Functional Significance of the Coincidence. J Cardiovasc Dev Dis 8:9
Basso C, Perazzolo Marra M (2018) Mitral Annulus Disjunction: Emerging Role of Myocardial Mechanical Stretch in Arrhythmogenesis. J Am Coll Cardiol 72:1610–1612
Dejgaard LA, Skjølsvik ET, Lie ØH et al (2018) The Mitral Annulus Disjunction Arrhythmic Syndrome. J Am Coll Cardiol 72:1600–1609
Brochhausen C, Turial S, Müller FK et al (2012) Pectus excavatum: history, hypotheses and treatment options. Interact Cardiovasc Thorac Surg 14:801–806
Nomura K, Ajiro Y, Nakano S et al (2019) Characteristics of mitral valve leaflet length in patients with pectus excavatum: A single center cross-sectional study. PLoS ONE 14:e0212165
Nicolosi GL (2020) The strain and strain rate imaging paradox in echocardiography: overabundant literature in the last two decades but still uncertain clinical utility in an individual case. Arch Med Sci Atheroscler Dis 5:e297–e305
Toh H, Mori S, Izawa Y et al (2021) Prevalence and extent of mitral annular disjunction in structurally normal hearts: comprehensive 3D analysis using cardiac computed tomography. Eur Heart J Cardiovasc Imaging 22:614–622
Voigt JU, Pedrizzetti G, Lysyansky P et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16:1–11
Author information
Authors and Affiliations
Contributions
AS: Conceptualization; Data curation; Investigation; Methodology; Software; Visualization; Writing—original draft. ER: Conceptualization; Data curation; Methodology; Writing—review & editing. GLN: Conceptualization; Supervision; Validation; Writing—review & editing. ML: Conceptualization; Supervision; Validation; Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
We wish to confirm that there are no conflicts of interest associated with this publication. Andrea Sonaglioni declares that he has no conflict of interest. Gian Luigi Nicolosi declares that he has no conflict of interest. Elisabetta Rigamonti declares that she has no conflict of interest. Michele Lombardo declares that he has no conflicts of interest.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sonaglioni, A., Nicolosi, G.L., Rigamonti, E. et al. The influence of chest wall conformation on myocardial strain parameters in a cohort of mitral valve prolapse patients with and without mitral annular disjunction. Int J Cardiovasc Imaging 39, 61–76 (2023). https://doi.org/10.1007/s10554-022-02705-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02705-w