Abstract
Objectives
Anatomical substrate and mechanical trigger co-act in arrhythmia’s onset in patients with bileaflet mitral valve prolapse (bMVP). Feature tracking (FT) may improve risk stratification provided by cardiac magnetic resonance (CMR). The aim was to investigate differences in CMR and FT parameters in bMVP patients with and without complex arrhythmias (cVA and no-cVA).
Methods
In this retrospective study, 52 patients with bMVP underwent 1.5 T CMR and were classified either as no-cVA (n = 32; 12 males; 49.6 ± 17.4 years) or cVA (n = 20; 3 males; 44.7 ± 11.2 years), the latter group including 6 patients (1 male; 45.7 ± 12.7 years) with sustained ventricular tachycardia or ventricular fibrillation (SVT-FV). Twenty-four healthy volunteers (11 males, 36.2 ± 12.5 years) served as control. Curling, prolapse distance, mitral annulus disjunction (MAD), and late gadolinium enhancement (LGE) were recorded and CMR-FT analysis performed. Statistical analysis included non-parametric tests and binary logistic regression.
Results
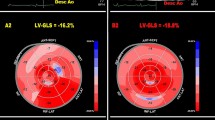
LGE and MAD distance were associated with cVA with an odds ratio (OR) of 8.51 for LGE (95% CI 1.76, 41.28; p = 0.008) and of 1.25 for MAD (95% CI 1.02, 1.54; p = 0.03). GLS 2D (− 11.65 ± 6.58 vs − 16.55 ± 5.09 1/s; p = 0.04), PSSR longitudinal 2D (0.04 ± 1.62 1/s vs − 1.06 ± 0.35 1/s; p = 0.0001), and PSSR radial 3D (3.95 ± 1.97 1/s vs 2.64 ± 1.03 1/s; p = 0.0001) were different for SVT-VF versus the others. PDSR circumferential 2D (1.10 ± 0.54 vs. 0.84 ± 0.34 1/s; p = 0.04) and 3D (0.94 ± 0.42 vs. 0.69 ± 0.17 1/s; p = 0.04) differed between patients with and without papillary muscle LGE.
Conclusions
CMR-FT allowed identifying subtle myocardial deformation abnormalities in bMVP patients at risk of SVT-VF. LGE and MAD distance were associated with cVA.
Key Points
• CMR-FT allows identifying several subtle myocardial deformation abnormalities in bMVP patients, especially those involving the papillary muscle.
• CMR-FT allows identifying subtle myocardial deformation abnormalities in bMVP patients at risk of SVT and VF.
• In patients with bMVP, the stronger predictor of cVA is LGE (OR = 8.51; 95% CI 1.76, 41.28; p = 0.008), followed by MAD distance (OR = 1.25; 95% CI 1.02, 1.54; p = 0.03).



Similar content being viewed by others
Abbreviations
- bMVP:
-
Bileaflet mitral valve prolapse
- cVA:
-
Complex ventricular arrhythmias
- EF:
-
Ejection fraction
- FT:
-
Feature tracking
- GCS:
-
Global circumferential strain
- GLS:
-
Global longitudinal strain
- GRS:
-
Global radial strain
- HC:
-
Healthy control
- MAD:
-
Mitral annulus disjunction
- MVP:
-
Mitral valve prolapse
- no-cVA:
-
Non-complex ventricular arrhythmias
- PD:
-
Prolapse distance
- PDSR:
-
Peak diastolic strain rate
- PSSR:
-
Peak systolic strain rate
- SVT:
-
Sustained ventricular tachycardia
- VA:
-
Ventricular arrhythmia
- VF:
-
Ventricular fibrillation
References
Hayek E, Gring CN, Griffin BP (2005) Mitral valve prolapse. Lancet 365:507–518. https://doi.org/10.1016/S0140-6736(05)17869-6
Delling FN, Vasan RS (2014) Epidemiology and pathophysiology of mitral valve prolapse. Circulation 129:2158–2170. https://doi.org/10.1161/CIRCULATIONAHA.113.006702
Jeresaty RM (1986) Mitral valve prolapse: definition and implications in athletes. J Am Coll Cardiol 7:231–236. https://doi.org/10.1016/S0735-1097(86)80286-8
Basso C, Iliceto S, Thiene G, Perazzolo Marra M (2019) Mitral valve prolapse, ventricular arrhythmias, and sudden death. Circulation 140:952–964. https://doi.org/10.1161/CIRCULATIONAHA.118.034075
Barlow JB, Pocock WA (1963) The significance of late systolic murmurs and mid-late systolic clicks. Md State Med J 12:76–77
Sriram CS, Syed FF, Ferguson ME et al (2013) Malignant bileaflet mitral valve prolapse syndrome in patients with otherwise idiopathic out-of-hospital cardiac arrest. J Am Coll Cardiol 62:222–230. https://doi.org/10.1016/j.jacc.2013.02.060
Nishimura RA, Otto CM, Bonow RO et al (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary. Circulation 129:2440–2492. https://doi.org/10.1161/CIR.0000000000000029
Basso C, Perazzolo Marra M, Rizzo S et al (2015) Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation 132:556–566. https://doi.org/10.1161/CIRCULATIONAHA.115.016291
Dejgaard LA, Skjølsvik ET, Lie ØH et al (2018) The mitral annulus disjunction arrhythmic syndrome. J Am Coll Cardiol 72:1600–1609. https://doi.org/10.1016/j.jacc.2018.07.070
Pradella S, Grazzini G, Brandani M et al (2019) Cardiac magnetic resonance in patients with mitral valve prolapse: focus on late gadolinium enhancement and T1 mapping. Eur Radiol 29:1546–1554. https://doi.org/10.1007/s00330-018-5634-5
Bui AH, Roujol S, Foppa M et al (2017) Diffuse myocardial fibrosis in patients with mitral valve prolapse and ventricular arrhythmia. Heart 103:204–209. https://doi.org/10.1136/heartjnl-2016-309303
Chitiboi T, Axel L (2017) Magnetic resonance imaging of myocardial strain: a review of current approaches. J Magn Reson Imaging 46:1263–1280. https://doi.org/10.1002/jmri.25718
Ermakov S, Gulhar R, Lim L et al (2019) Left ventricular mechanical dispersion predicts arrhythmic risk in mitral valve prolapse. Heart 105:1063–1069. https://doi.org/10.1136/heartjnl-2018-314269
Han Y, Peters DC, Salton CJ et al (2008) Cardiovascular magnetic resonance characterization of mitral valve prolapse. JACC Cardiovasc Imaging 1:294–303. https://doi.org/10.1016/j.jcmg.2008.01.013
Gatti M, Palmisano A, Faletti R et al (2019) Two-dimensional and three-dimensional cardiac magnetic resonance feature-tracking myocardial strain analysis in acute myocarditis patients with preserved ejection fraction. Int J Cardiovasc Imaging 35:1101–1109. https://doi.org/10.1007/s10554-019-01588-8
Kramer CM, Barkhausen J, Flamm SD et al (2013) Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson 15:91. https://doi.org/10.1186/1532-429X-15-91
Nacif MS, Barranhas AD, Türkbey E et al (2012) Left atrial volume quantification using cardiac MRI in atrial fibrillation: comparison of the Simpson’s method with biplane area-length, ellipse, and three-dimensional methods. Diagn Interv Radiol. https://doi.org/10.5152/dir.2012.002
Perazzolo Marra M, Basso C, De Lazzari M et al (2016) Morphofunctional abnormalities of mitral annulus and arrhythmic mitral valve prolapse. Circ Cardiovasc Imaging 9. https://doi.org/10.1161/CIRCIMAGING.116.005030
Gilbert BW, Schatz RA, VonRamm OT et al (1976) Mitral valve prolapse. Two-dimensional echocardiographic and angiographic correlation. Circulation 54:716–723. https://doi.org/10.1161/01.CIR.54.5.716
Eriksson MJ, Bitkover CY, Omran AS et al (2005) Mitral annular disjunction in advanced myxomatous mitral valve disease: echocardiographic detection and surgical correction. J Am Soc Echocardiogr 18:1014–1022. https://doi.org/10.1016/j.echo.2005.06.013
Kitkungvan D, Nabi F, Kim RJ et al (2018) Myocardial fibrosis in patients with primary mitral regurgitation with and without prolapse. J Am Coll Cardiol 72:823–834. https://doi.org/10.1016/j.jacc.2018.06.048
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Schulz-Menger J, Bluemke DA, Bremerich J et al (2013) Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) Board of Trustees Task Force on Standardized Post Processing. J Cardiovasc Magn Reson 15:35. https://doi.org/10.1186/1532-429X-15-35
Schulz-Menger J, Bluemke DA, Bremerich J et al (2020) Standardized image interpretation and post-processing in cardiovascular magnetic resonance - 2020 update. J Cardiovasc Magn Reson 22:19. https://doi.org/10.1186/s12968-020-00610-6
Di Leo G, Sardanelli F (2020) Statistical significance: p value, 0.05 threshold, and applications to radiomics—reasons for a conservative approach. Eur Radiol Exp 4:18. https://doi.org/10.1186/s41747-020-0145-y
Bennett S, Thamman R, Griffiths T et al (2019) Mitral annular disjunction: a systematic review of the literature. Echocardiography 36:1549–1558. https://doi.org/10.1111/echo.14437
Slavich M, Palmisano A, Pannone L et al (2019) Hidden danger behind the prolapse. Circ Cardiovasc Imaging 12. https://doi.org/10.1161/CIRCIMAGING.119.009639
Kalam K, Otahal P, Marwick TH (2014) Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart 100:1673–1680. https://doi.org/10.1136/heartjnl-2014-305538
Huttin O, Pierre S, Venner C et al (2016) Interactions between mitral valve and left ventricle analysed by 2D speckle tracking in patients with mitral valve prolapse: one more piece to the puzzle. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jew075
Wang J, Khoury DS, Thohan V et al (2007) Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation 115:1376–1383. https://doi.org/10.1161/CIRCULATIONAHA.106.662882
Ruivo C, Vilela EM, Ladeiras-Lopes R et al (2019) Myocardial deformation measures by cardiac magnetic resonance tissue tracking in myocarditis: relationship with systolic function and myocardial damage. Rev Port Cardiol 38:767–776. https://doi.org/10.1016/j.repc.2019.01.008
Kempny A, Fernández-Jiménez R, Orwat S et al (2012) Quantification of biventricular myocardial function using cardiac magnetic resonance feature tracking, endocardial border delineation and echocardiographic speckle tracking in patients with repaired tetralogy of fallot and healthy controls. J Cardiovasc Magn Reson 14:32. https://doi.org/10.1186/1532-429X-14-32
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Riccardo Faletti.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Healthy volunteer cohort has been previously reported in Gatti M, Palmisano A, Faletti R, Benedetti G, Bergamasco L, Bioletto F, Peretto G, Sala S, De Cobelli F, Fonio P, Esposito A. Two-dimensional and three-dimensional cardiac magnetic resonance feature-tracking myocardial strain analysis in acute myocarditis patients with preserved ejection fraction. Int J Cardiovasc Imaging. 2019;35:1101–1109.
Methodology
• Retrospective
• Case-control study
• Multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gatti, M., Palmisano, A., Esposito, A. et al. Feature tracking myocardial strain analysis in patients with bileaflet mitral valve prolapse: relationship with LGE and arrhythmias. Eur Radiol 31, 7273–7282 (2021). https://doi.org/10.1007/s00330-021-07876-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07876-z