Abstract
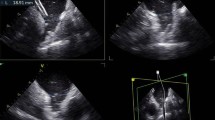
During transfemoral (TF) or transcatheter aortic valve replacement (TAVR), transesophageal echocardiography (TEE) sometimes reveals an unexpected mobile membranous mass on the catheter tip within the proximal part of the descending thoracic aorta. Such mobile masses may cause critical embolic events if the TAVR device advances into the ascending aorta in the absence of preventive measures. This study aimed to investigate the incidence and predictors of emboligenic matter (EM) during TAVR, impact of EM on the procedure, and incidence of symptomatic ischemic stroke post procedure. Among 436 consecutive patients who underwent TF–TAVR, 407 were evaluated in this study. The primary end point was incidence of symptomatic ischemic stroke within 24 h post procedure while taking appropriate preventive measures. Incidence of EM, factors associated with EM, and the impact of EM on the procedure were also investigated. Among the 407 cases, 15 cases (3.7%) of EM were identified but no ischemic stroke occurred in the EM (+) group (0% vs. 2.04%, p = 1.00). In the EM (+) group, a self-expandable valve was used in all 15 cases (100% vs. 42.6%, p < 0.0001) while 14 cases used a CoreValve’s InLine sheath system initially (93.3% vs. 27.3%, p < 0.0001). CoreValve’s InLine sheath system usage was the only independent predictor of EM. The CoreValve’s InLine delivery system was identified as a predictor of EM during TF–TAVR, but symptomatic ischemic stroke was avoided while taking appropriate embolization preventive measures.



Similar content being viewed by others
References
Hanna J, Jose C, Chandan D, Vinod T (2015) Minimalist transcatheter aortic valve replacement: the new standard for surgeons and cardiologists using transfemoral access? J Thorac Cardiovasc Surg 4:833–840
Babaliaros V, Devireddy C, Lerakis S, Leonardi R, Iturra SA, Mavromatis K, Leshnower BG, Guyton RA, Kanitkar M, Keegan P, Simone A (2014) Comparison of transfemoral transcatheter aortic valve replacement performed in the catheterization laboratory (minimalist approach) versus hybrid operating room (standard approach): outcomes and cost analysis. JACC Cardiovasc Interv 7:898–904. https://doi.org/10.1016/j.jcin.2014.04.005
Gurevich S, Oestreich B, Kelly RF, Mbai M, Bertog S, Ringsred K, Lawton A, Thooft B, Wagner J, Garcia S (2018) Outcomes of transcatheter aortic valve replacement using a minimalist approach. Cardiovasc Revasc Med 19:192–195. https://doi.org/10.1016/j.carrev.2017.08.002
Butala NM, Chung M, Secemsky EA, Manandhar P, Marquis-Gravel G, Kosinski AS, Vemulapalli S, Yeh RW, Cohen DJ (2020) Conscious sedation versus general anesthesia for transcatheter aortic valve replacement: variation in practice and outcomes. JACC Cardiovasc Interv 13:1277–1287. https://doi.org/10.1016/j.jcin.2020.03.008
Kadoya Y, Zen K, Yamano M, Yamano T, Nakamura T, Yaku H, Matoba S (2020) Exfoliated endothelium identified by transesophageal echocardiography during TAVR. JACC Cardiovasc Interv 13:e49–e50. https://doi.org/10.1016/j.jcin.2019.12.004
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD (2005) Recommendations for chamber quantification: a Report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463. https://doi.org/10.1016/j.echo.2005.10.005
Blanke P, Weir-McCall JR, Achenbach S, Delgado V, Hausleiter J, Jilaihawi H, Marwan M, Nørgaard BL, Piazza N, Schoenhagen P, Leipsic JA (2019) Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging 12:1–24. https://doi.org/10.1016/j.jcmg.2018.12.003
Kinnel M, Faroux L, Villecourt A, Tassan-Mangina S, Heroguelle V, Nazeyrollas P, Poncet A, Ruggieri VG, Metz D (2020) Abdominal aorta tortuosity on computed tomography identifies patients at risk of complications during transfemoral transcatheter aortic valve replacement. Arch Cardiovasc Dis 113:159–167. https://doi.org/10.1016/j.acvd.2019.10.006
Brody W, Matthew C, Nicos L, Lee S, Thomas B (2021) High prevalence of abdominal aortic aneurysms in patients with lung cancer. J Vasc Surg 73:850–855
Roos CJ, Witkowska AJ, de Graaf MA, Veltman CE, Delgado V, de Grooth GJ, Jukema JW, Bax JJ, Scholte AJ (2013) Association of atherosclerosis in the descending thoracic aorta with coronary artery disease on multi detector row computed tomography coronary angiography in patients with suspected coronary artery disease. Int J Cardiovasc Imaging 29:1829–1837. https://doi.org/10.1007/s10554-013-0266-y
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, Van Es GA, Hahn RT (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J 33:2403–2418. https://doi.org/10.1093/eurheartj/ehs255
Yashige M, Zen K, Kadoya Y, Matoba S (2021) Combining the CoreValve Evolut PRO and 14-French eSheath in transfemoral transcatheter aortic valve replacement. Cardiovasc Interv Ther 36:266–267. https://doi.org/10.1007/s12928-020-00659-1
Huded CP, Tuzcu EM, Krishnaswamy A, Mick SL, Kleiman NS, Svensson LG, Carroll J, Thourani VH, Kirtane AJ, Manandhar P, Kosinski AS (2019) Association between transcatheter aortic valve replacement and early postprocedural stroke. JAMA 321:2306–2315. https://doi.org/10.1001/jama.2019.7525
Mastoris I, Schoos MM, Dangas GD, Mehran R (2014) Stroke after transcatheter aortic valve replacement: incidence, risk factors, prognosis, and preventive strategies. Clin Cardiol 37:756–764. https://doi.org/10.1002/clc.22328
Toggweiler S, Gurvitch R, Leipsic J, Wood DA, Willson AB, Binder RK, Cheung A, Ye J, Webb JG (2012) Percutaneous aortic valve replacement: vascular outcomes with a fully percutaneous procedure. J Am Coll Cardiol 59:113–118. https://doi.org/10.1016/j.jacc.2011.08.069
Giustino G, Mehran R, Veltkamp R, Faggioni M, Baber U, Dangas GD (2016) Neurological outcomes with embolic protection devices in patients undergoing transcatheter aortic valve replacement: a systematic review and meta-analysis of randomized controlled trials. JACC Cardiovasc Interv 9:2124–2133. https://doi.org/10.1016/j.jcin.2016.07.024
Holger E, Axel S, Thomas V, Rajendra HM (2012) Risk of stroke after transcatheter aortic valve implantation (TAVI): a meta-analysis of 10,037 published patients. EuroIntervention 8:129–138
Grube E, Van Mieghem NM, Bleiziffer S, Modine T, Bosmans J, Manoharan G, Linke A, Scholtz W, Tchétché D, Finkelstein A, Trillo R (2017) Clinical outcomes with a repositionable self-expanding transcatheter aortic valve prosthesis: the International FORWARD Study. J Am Coll Cardiol 70:845–853
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. MY collected data, performed statistical analysis, and wrote the manuscript. KZ, MY, TY, TN, HY, and SM revised the manuscript and figures. SN, TF, KT, NI, and YK collected data and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was obtained from the Ethics Committee of Kyoto Prefectural University of Medicine. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 5423 kb)
Supplementary file2 (MP4 1755 kb)
Supplementary file3 (MP4 2777 kb)
Supplementary file4 (MP4 4592 kb)
Rights and permissions
About this article
Cite this article
Yashige, M., Zen, K., Nakamura, S. et al. Incidence and predictors of transcatheter aortic valve replacement device emboligenic matter detected by transesophageal echocardiography. Int J Cardiovasc Imaging 38, 1741–1750 (2022). https://doi.org/10.1007/s10554-022-02567-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02567-2