Abstract
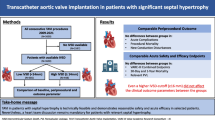
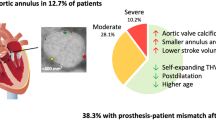
The role of sigmoid septum (SS) observed using preprocedural transthoracic echocardiography (TTE) in patients undergoing transcatheter aortic valve implantation (TAVI) remains unknown. This study aimed to compare clinical outcomes of TAVI using the current-generation transcatheter heart valves in patients with and without SS. We divided 140 consecutive patients, excluding four patients who underwent pacemaker implantation before TAVI, into two groups (those with and without SS) and compared the periprocedural outcomes, including new pacemaker implantation, within 30 days post-TAVI. Thirty-five patients (25%; 32 female patients) had SS before TAVI. The body surface area and aortic annulus area measured using computed tomography were significantly smaller in patients with SS than in those without SS (1.40 m2 vs. 1.48 m2, P = 0.03; and 372 mm2 vs. 409 mm2, P < 0.01; respectively). Device success was achieved in all patients with SS. Postprocedural TTE on 30 days post-TAVI showed no significant differences in the valvular hemodynamics between patients with and without SS. No severe prosthesis-patient mismatch was noted on TTE, although the transcatheter heart valve size tended to be smaller in patients with SS. Within 30 days of the TAVI, three (8.6%) and eight (7.6%) patients with and without SS, respectively, had new pacemaker implantation (P = 0.86). The presence of SS was not associated with periprocedural outcomes following TAVI in patients without pre-existing pacemakers. No specific assessment or treatment strategy is required for the TAVI in patients with SS using the current-generation devices.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, Masami Nishino, upon reasonable request.
References
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M et al (2019) Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 380:1695–1705. https://doi.org/10.1056/NEJMoa1814052
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D et al (2019) Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 380:1706–1715. https://doi.org/10.1056/NEJMoa1816885
Maeno Y, Abramowitz Y, Kawamori H, Kazuno Y, Kubo S, Takahashi N et al (2017) A highly predictive risk model for pacemaker implantation after TAVR. JACC Cardiovasc Imaging 10:1139–1147. https://doi.org/10.1016/j.jcmg.2016.11.020
Jilaihawi H, Zhao Z, Du R, Staniloae C, Saric M, Neuburger PJ et al (2019) Minimizing permanent pacemaker following repositionable self-expanding transcatheter aortic valve replacement. JACC Cardiovasc Interv 12:1796–1807. https://doi.org/10.1016/j.jcin.2019.05.056
Di Tommaso L, Stassano P, Mannacio V, Russolillo V, Monaco M, Pinna G et al (2013) Asymmetric septal hypertrophy in patients with severe aortic stenosis: the usefulness of associated septal myectomy. J Thorac Cardiovasc Surg 145:171–175. https://doi.org/10.1016/j.jtcvs.2011.10.0966
Giannini F, Montorfano M, Romano V, Ruparelia N, Jabbour RJ, Benincasa S et al (2016) Valve embolization with a second-generation fully-retrievable and repositionable transcatheter aortic valve. Int J Cardiol 223:867–869
de Biasi AR, Worku B, Skubas NJ, Salemi A (2015) Sigmoid septum and balloon-expandable transcatheter aortic valve replacement: a cautionary tale. J Heart Valve Dis 24:465–467. https://doi.org/10.1016/j.ijcard.2016.08.327
Yamashita K, Fujita T, Fukushima S, Shimahara Y, Kume Y, Matsumoto Y et al (2018) Transcatheter aortic valve replacement for severe aortic stenosis complicated by sigmoid septum. Circ J 82:3090–3099. https://doi.org/10.1253/circj.CJ-18-0264
Diaz T, Pencina MJ, Benjamin EJ, Aragam J, Fuller DL, Pencina KM et al (2009) Prevalence, clinical correlates, and prognosis of discrete upper septal thickening on echocardiography: the Framingham Heart Study. Echocardiography 26:247–253. https://doi.org/10.1111/j.1540-8175.2008.00806.x
Généreux P, Piazza N, Alu MC, Nazif T, Hahn RT, Pibarot P et al (2021) Valve Academic Research Consortium 3: updated endpoint definitions for aortic valve clinical research. Eur Heart J 42:1825–1857. https://doi.org/10.1093/eurheartj/ehaa799
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1-39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A et al (2009) AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Soc Echocardiogr 53:976–981. https://doi.org/10.1016/j.jacc.2008.12.013
Blanke P, Weir-McCall JR, Achenbach S, Delgado V, Hausleiter J, Jilaihawi H et al (2019) Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging 12:1–24. https://doi.org/10.1016/j.jcmg.2018.12.003
Elattar MA, Vink LW, van Mourik MS, Baan J Jr, van Bavel ET, Planken RN et al (2017) Dynamics of the aortic annulus in 4D CT angiography for transcatheter aortic valve implantation patients. PLoS ONE 12:e0184133. https://doi.org/10.1371/journal.pone.0184133
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ et al (2017) 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 38:2739–2791. https://doi.org/10.1093/eurheartj/ehx391
Izumi C, Eishi K, Ashihara K, Arita T, Otsuji Y, Kunihara T et al (2020) JCS/JSCS/JATS/JSVS 2020 guidelines on the management of valvular heart disease. Circ J 84:2037–2119. https://doi.org/10.1253/circj.CJ-20-0135
Blanke P, Pibarot P, Hahn R, Weissman N, Kodali S, Thourani V et al (2017) Computed tomography-based oversizing degrees and incidence of paravalvular regurgitation of a new generation transcatheter heart valve. JACC Cardiovasc Interv 10:810–820. https://doi.org/10.1016/j.jcin.2017.02.021
De Carlo M, Giannini C, Bedogni F, Klugmann S, Brambilla N, De Marco F et al (2012) Safety of a conservative strategy of permanent pacemaker implantation after transcatheter aortic CoreValve implantation. Am Heart J 163:492–499. https://doi.org/10.1016/j.ahj.2011.12.009
Kalich BA, Allender JE, Hollis IB (2018) Medication management of patients undergoing transcatheter aortic valve replacement. Pharmacotherapy 38:122–138. https://doi.org/10.1002/phar.2056
Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA et al (2009) Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report From the American Society of Echocardiography’s Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J Am Soc Echocardiogr 22:975–1014. https://doi.org/10.1016/j.echo.2009.07.013
Husser O, Pellegrini C, Kessler T, Burgdorf C, Thaller H, Mayr NP et al (2016) Predictors of permanent pacemaker implantations and new-onset conduction abnormalities with the SAPIEN 3 balloon-expandable transcatheter heart valve. JACC Cardiovasc Interv 9:244–254. https://doi.org/10.1016/j.jcin.2015.09.036
Kiefer NJ, Salber GC, Burke GM, Chang JD, Guibone KA, Popma JJ et al (2019) The impact of basal septal hypertrophy on outcomes after transcatheter aortic valve replacement. J Am Soc Echocardiogr 32:1416–1425. https://doi.org/10.1016/j.echo.2019.06.012
Mehrotra P, Flynn AW, Jansen K, Tan TC, Mak G, Julien HM et al (2015) Differential left ventricular outflow tract remodeling and dynamics in aortic stenosis. J Am Soc Echocardiogr 28:1259–1266. https://doi.org/10.1016/j.echo.2015.07.018
Unbehaun A, Pasic M, Dreysse S, Drews T, Kukucka M, Mladenow A et al (2012) Transapical aortic valve implantation: incidence and predictors of paravalvular leakage and transvalvular regurgitation in a series of 358 patients. J Am Coll Cardiol 59:211–221. https://doi.org/10.1016/j.jacc.2011.10.857
Yang TH, Webb JG, Blanke P, Dvir D, Hansson NC, Nørgaard BL et al (2015) Incidence and severity of paravalvular aortic regurgitation with multidetector computed tomography nominal area oversizing or undersizing after transcatheter heart valve replacement with the Sapien 3: a comparison with the Sapien XT. JACC Cardiovasc Interv 8:462–471. https://doi.org/10.1016/j.jcin.2014.10.014
Herrmann HC, Daneshvar SA, Fonarow GC, Stebbins A, Vemulapalli S, Desai ND et al (2018) Prosthesis-patient mismatch in patients undergoing transcatheter aortic valve replacement: from the STS/ACC TVT Registry. J Am Coll Cardiol 72:2701–2711. https://doi.org/10.1016/j.jacc.2018.09.001
Meguro K, Kumamaru H, Kohsaka S, Hashimoto T, Kakizaki R, Kitamura T et al (2021) Transcatheter aortic valve replacement in patients with a small annulus: from the Japanese Nationwide Registry (J-TVT). Circ J 85:967–976. https://doi.org/10.1253/circj.CJ-20-1084
Lee Y, Mori N, Nakamura D, Yoshimura T, Taniike M, Makino N et al (2014) New approach for rotational dyssynchrony using three-dimensional speckle tracking echocardiography. Echocardiography 31:492–498. https://doi.org/10.1111/echo.12406
Dogdus M, Yildirim A, Kucukosmanoglu M, Kilic S, Yavuzgil O, Nalbantgil S (2021) Are there any subclinical myocardial dysfunctions in subjects with aortic valve sclerosis? A 3D-speckle tracking echocardiography study. Int J Cardiovasc Imaging 37:207–213. https://doi.org/10.1007/s10554-020-01977-4
Acknowledgements
The authors thank Mr. John Martin for his linguistic assistance with this manuscript.
Funding
The authors have no funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MT, YE, YM, HN, KY, NO, YM, MY, and JT. The first draft of the manuscript was written by MT and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was waived by the Institutional Review Borad of Osaka Rosai Hospital in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tsuda, M., Egami, Y., Matsuhiro, Y. et al. Impact of sigmoid septum on periprocedural outcomes following transcatheter aortic valve implantation using current-generation valves. Int J Cardiovasc Imaging 38, 171–180 (2022). https://doi.org/10.1007/s10554-021-02479-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02479-7