Abstract
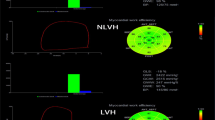
This study aimed to quantitatively evaluate myocardial work (MW) in advanced stage 3–5 chronic kidney disease (CKD) by a novel non-invasive left ventricular (LV) Pressure–strain loop analysis (PSL). 144 patients with CKD were included (68 with stage 3 CKD group, 76 with stage 4/5 CKD group), and 48 healthy patients were recruited as the control group. All subjects had undergone transthoracic echocardiography. LV myocardial work and efficiency were estimated from LV PSL analysis. There was a significant progressive increase in global work waste (GWW) and reduction in global work efficiency (GWE) in CKD compared to normal controls. No difference in global work index (GWI) and global constructive work (GCW) was observed among the three groups. Subdivided analysis according to systolic blood pressure (SBP) and LV geometry discovered that increased GWW seems to be present frequently in CKD patients with elevated SBP or LV hypertrophy (LVH). Multivariate analysis showed increased peak strain dispersion (PSD), SBP, LV mass index (LVMI), and decreased estimated glomerular filtration rate (eGFR) were significantly associated with increased GWW. The decline of renal function followed by impaired paralleled myocardial energy exploitation. Moreover, increased PSD, SBP, LVMI, and decreased eGFR might be potential drivers of increased GWW.



Similar content being viewed by others
References
Essig M, Escoubet B, de Zuttere D, Blanchet F, Arnoult F, Dupuis E, Michel C, Mignon F, Mentre F, Clerici C, Vrtovsnik F (2008) Cardiovascular remodelling and extracellular fluid excess in early stages of chronic kidney disease. Nephrol Dial Transpl 23(1):239–248. https://doi.org/10.1093/ndt/gfm542
Unger ED, Dubin RF, Deo R, Daruwalla V, Friedman JL, Medina C, Beussink L, Freed BH, Shah SJ (2016) Association of chronic kidney disease with abnormal cardiac mechanics and adverse outcomes in patients with heart failure and preserved ejection fraction. Eur J Heart Fail 18(1):103–112. https://doi.org/10.1002/ejhf.445
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, Haugaa KH, Opdahl A, Fjeld JG, Gjesdal O, Edvardsen T, Smiseth OA (2012) A novel clinical method for quantification of regional left ventricular Pressure–strain loop area: a non-invasive index of myocardial work. Eur Heart J 33(6):724–733. https://doi.org/10.1093/eurheartj/ehs016
KDIGO (2018) 2018 clinical practice guideline for the prevention, diagnosis, evaluation, and treatment of hepatitis C in chronic kidney disease. Kidney Int Suppl 8:3
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002
Shehata IE, Eldamanhory AS, Shaker A (2020) Early predictors of left ventricular dysfunction in hypertensive patients: comparative cross-section study. Int J Cardiovasc Imaging 36(6):1031–1040. https://doi.org/10.1007/s10554-020-01790-z
Drazner MH (2011) The progression of hypertensive heart disease. Circulation 123(3):327–334. https://doi.org/10.1161/CIRCULATIONAHA.108.845792
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270. https://doi.org/10.1093/ehjci/jev014
Hubert A, Le Rolle V, Leclercq C, Galli E, Samset E, Casset C, Mabo P, Hernandez A, Donal E (2018) Estimation of myocardial work from pressure–strain loops analysis: an experimental evaluation. Eur Heart J Cardiovasc Imaging 19(12):1372–1379. https://doi.org/10.1093/ehjci/jey024
Edwards NFA, Scalia GM, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Khandheria BK, Chan J (2019) Global myocardial work is superior to global longitudinal strain to predict significant coronary artery disease in patients with normal left ventricular function and wall motion. J Am Soc Echocardiogr 32(8):947–957. https://doi.org/10.1016/j.echo.2019.02.014
Chalmers JO, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L, Neal B, Rodgers A, Ni CM, Clark T (1999) 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens 17(2):151–183
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Scalia GM (2019) A new approach to assess myocardial work by non-invasive left ventricular pressure–strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 20(1):31–39. https://doi.org/10.1093/ehjci/jey131
Galli E, Vitel E, Schnell F, Le Rolle V, Hubert A, Lederlin M, Donal E (2019) Myocardial constructive work is impaired in hypertrophic cardiomyopathy and predicts left ventricular fibrosis. Echocardiography (Mount Kisco, NY) 36(1):74–82. https://doi.org/10.1111/echo.14210
El Mahdiui M, van der Bijl P, Abou R, Ajmone Marsan N, Delgado V, Bax JJ (2019) Global left ventricular myocardial work efficiency in healthy individuals and patients with cardiovascular disease. J Am Soc Echocardiogr 32(9):1120–1127. https://doi.org/10.1016/j.echo.2019.05.002
Galli E, Leclercq C, Hubert A, Bernard A, Smiseth OA, Mabo P, Samset E, Hernandez A, Donal E (2018) Role of myocardial constructive work in the identification of responders to CRT. Eur Heart J Cardiovasc Imaging 19(9):1010–1018. https://doi.org/10.1093/ehjci/jex191
Galli E, Leclercq C, Fournet M, Hubert A, Bernard A, Smiseth OA, Mabo P, Samset E, Hernandez A, Donal E (2018) Value of myocardial work estimation in the prediction of response to cardiac resynchronization therapy. J Am Soc Echocardiogr 31(2):220–230. https://doi.org/10.1016/j.echo.2017.10.009
Boe E, Russell K, Eek C, Eriksen M, Remme EW, Smiseth OA, Skulstad H (2015) Non-invasive myocardial work index identifies acute coronary occlusion in patients with non-ST-segment elevation-acute coronary syndrome. Eur Heart J Cardiovasc Imaging 16(11):1247–1255. https://doi.org/10.1093/ehjci/jev078
Manganaro R, Marchetta S, Dulgheru R, Ilardi F, Sugimoto T, Robinet S, Cimino S, Go YY, Bernard A, Kacharava G, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Hagendorff A, Hristova K, Lopez-Fernandez T, de la Morena G, Popescu BA, Penicka M, Ozyigit T, Rodrigo Carbonero JD, van de Veire N, Von Bardeleben RS, Vinereanu D, Zamorano JL, Rosca M, Calin A, Moonen M, Magne J, Cosyns B, Galli E, Donal E, Carerj S, Zito C, Santoro C, Galderisi M, Badano LP, Lang RM, Oury C, Lancellotti P (2019) Echocardiographic reference ranges for normal non-invasive myocardial work indices: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging 20(5):582–590. https://doi.org/10.1093/ehjci/jey188
Shi F, Feng S, Zhu J, Wu Y, Chen J (2018) Left ventricular strain and dyssynchrony in young and middle-aged peritoneal dialysis patients and healthy controls: a case-matched study. Cardiorenal Med 8(4):271–284. https://doi.org/10.1159/000490395
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Gjesdal O, Edvardsen T, Smiseth OA (2013) Assessment of wasted myocardial work: a novel method to quantify energy loss due to uncoordinated left ventricular contractions. Am J Physiol Heart Circ Physiol 305(7):H996-1003. https://doi.org/10.1152/ajpheart.00191.2013
Hayashi SY, Seeberger A, Lind B, Nowak J, Nascimento MM, Lindholm B, Brodin LA (2008) A single session of haemodialysis improves left ventricular synchronicity in patients with end-stage renal disease: a pilot tissue synchronization imaging study. Nephrol Dial Transpl 23(11):3622–3628. https://doi.org/10.1093/ndt/gfn311
Murata T, Dohi K, Onishi K, Sugiura E, Fujimoto N, Ichikawa K, Ishikawa E, Nakamura M, Nomura S, Takeuchi H, Nobori T, Ito M (2011) Role of haemodialytic therapy on left ventricular mechanical dyssynchrony in patients with end-stage renal disease quantified by speckle-tracking strain imaging. Nephrol Dial Transpl 26(5):1655–1661. https://doi.org/10.1093/ndt/gfq590
Funding
This study was supported by grants from the Key Science and Technology Research Project of the Department of Education, Jiangxi Province (Grant No. 19002); Postgraduate Innovation Special Fund project of Nanchang University (Grant No. CX 2019135).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Research involving human rights
The work described has been carried out in accordance with the World Medical Association Declaration of Helsinki for experiments involving humans.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, FZ., Wang, XL. & Zhang, CQ. Quantitative assessment of left ventricular myocardial work in chronic kidney disease patients by a novel non-invasive pressure–strain loop analysis method. Int J Cardiovasc Imaging 37, 1567–1575 (2021). https://doi.org/10.1007/s10554-020-02132-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02132-9