Abstract
Background
Cardiac damage is the leading cause of death in uremic patients. This study aimed to evaluate the application of non-invasive myocardial work index (NIMWI) by echocardiography in assessing the left ventricular (LV) systolic function in uremic patients.
Methods
Twenty-six uremic patients and 27 age- and sex-matched healthy volunteers were enrolled in the study. Except for the conventional echocardiographic parameters, the LV myocardial work (MW) parameters including GWI (myocardial global work index), GCW (global constructive work), GWW (global wasted work), and GWE (global work efficiency) were calculated in study participants. Differences in MW parameters between the uremic and normal groups were compared by independent-sample t-test. Receiver operating characteristic (ROC) curves were constructed for MW parameters to detect abnormal LV systolic function in uremic patients.
Results
Compared with the normal group, GWW was significantly increased and GWE decreased in the uremic group (P < 0.05). Area under the curve (AUC) for GWE by the ROC analysis was 0.966. The best threshold, sensitivity and specificity values of GWE to detect abnormality of LV systolic function in uremic patients were 92.5%, 0.89 and 0.96, respectively.
Conclusions
NIMWI may be applied to assess the global MW of uremic patients. The presence of reduced GWE can help identify impaired left ventricular myocardial function in uremic patients with preserved LV ejection fraction with a high sensitivity and specificity.
Similar content being viewed by others
Background
Chronic kidney disease (CKD) is a common disease which seriously threatens patients’ health and life. The disease causes damage to multiple systems and organs, especially in its end-stage (i.e. uremia). Indeed, cardiac damage is the leading cause of death in uremic patients [1]. Earlier studies have demonstrated that myocardial contraction function of the uremic patients has been impaired when the left ventricular ejection fraction (LVEF) is normal [2]. Therefore, an objective and accurate method to evaluate left ventricular (LV) systolic function in uremic patients is urgently needed.
The pressure–volume loop method measured by cardiac catheterization can assess the LV systolic function and myocardial oxygen consumption accurately [3]. However, this method is fairly invasive and has limited application in clinical practice. LVEF, measured by conventional transthoracic echocardiography, is the indicator most commonly used to predict mortality or morbidity of cardiovascular disease; Nonetheless it is often influenced by pre- and post-loads and the cardiac structure [4]. Previous studies reported that the global longitudinal strain (GLS) obtained by two-dimensional (2D) speckle tracking technology is more sensitive for diagnosing abnormalities of LV systolic function than conventional LVEF [5]. However, myocardial strain is susceptible to the cardiac afterload, which can affect the accuracy of myocardial function evaluation. The non-invasive myocardial work index (NIMWI) is a new method based on 2D speckle tracking technology that combines myocardial deformation and LV pressure to evaluate LV myocardial work (MW), which is more objective than GLS alone [6]. Russell et al. demonstrated a good correlation between NIMWI assessment and invasive and direct measurements of MW [7].
Previous studies have indicated that the NIMWI can evaluate the LV MW in patients with CKD without dialysis [8], but the MW in CKD patients undergoing haemodialysis treatment has not been studied. Thus, this study aimed to evaluate the feasibility of the NIMWI for assessing LV global MW in uremic patients with preserved ejection fraction undergoing haemodialysis, and provided reference values for the clinical evaluation of LV systolic function in these patients.
Results
Clinical characteristics
Compared with the normal group, the uremic group showed higher systolic blood pressures (SBP) and diastolic blood pressures (DBP). The differences between groups were statistically significant (both P < 0.05). There were no differences in gender, age, heart rate (HR) and body surface area (BSA) between the two groups (P > 0.05) (Table 1).
Traditional echocardiographic measurement
Compared with the normal group, the uremic group showed increased interventricular septum end-diastolic thickness (IVSTd), LV posterior wall end-diastolic thickness (LVPWTd), LV end-diastolic diameter (LVEDd), LV mass index (LVMI) and decreased GLS. The differences between groups were statistically significant (P < 0.05). There were no significant differences in LVEF between the two groups (P > 0.05) (Table 2).
Comparison of MW parameters
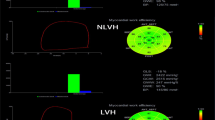
Compared with the normal group, the uremic group showed increased global wasted work (GWW) and decreased global work efficiency (GWE). The differences observed between groups were statistically significant (P < 0.05). However, differences in global work index (GWI) and global constructive work (GCW) between the two groups were not statistically significant (P > 0.05) (Table 3, Fig. 1).
A: Left ventricular MW parameters of the normal group. B: Left ventricular MW parameters of uremic patients. In each group, the LV PSL, 17-segment bull's-eye representation of GWI, and the MW parameters were given, and the MW parameters included GWI, GCW, GWW, and GWE. MW: myocardial work; PSL: pressure–strain loops; GLS: global longitudinal strain; GWI: global work index; GCW: global constructive work; GWW: global waste work; GWE: global work efficiency
Main relations of NIMWI
GWE and GWW showed a good correlation with SBP (r = − 0.83, P < 0.001 and r = 0.72, P < 0.001, respectively).
Receiver operating characteristic (ROC) curve analysis
Based on ROC curve analysis of main MW parameter, area under the curve (AUC) of GWE and GWW were 0.966 and 0.925, respectively. GWE was the best diagnostic index for identifying impaired LV myocardial function in uremic patients with preserved LV ejection fraction. The sensitivity and specificity were 89% and 96%, respectively. The best threshold of GWE was 92.5% (Fig. 2).
ROC curve analysis of the main MW parameters for identifying impaired LV myocardial function in uremic patients with preserved LV ejection fraction. On the left: ROC curve of GWW parameter (AUC = 0.925). On the right: ROC curve of GWE parameter (AUC = 0.966). GWE had better AUC than GWW with the sensitivity, specificity and optimal threshold of 89%, 96% and 92.5%, respectively. ROC: receiver operating characteristic; GWE: global work efficiency
Intra- and inter-observer variability
Intra-class correlation coefficients indicated that GWI, GCW, GWW and GWE between the intra- and inter-observer measurements were consistent (Table 4).
Discussion
Uremia is the final stage of CKD progression. Serious damage to the kidney functions promotes the production and accumulation of toxins in the body, resulting in multi-organ dysfunction and poor health. Cardiovascular complications are the main cause of death in patients with uremia [9]. Therefore, early detection of changes in myocardial contraction in uremic patients is important to enable the early control of cardiovascular complications. The results of our study showed that compared with the control group, there were no change in LVEF in uremic patients (P > 0.05), but the uremic group showed increased GWW and decreased GWE (P < 0.05), indicating that the NIMWI can identify LV systolic dysfunction in uremic patients with preserved ejection fraction. GWE was the best diagnostic index for identifying impaired LV myocardial function in uremic patients with preserved LV ejection fraction, and its sensitivity, specificity and optimal threshold were 89%, 96% and 92.5%, respectively.
Traditional evaluations of MW mainly rely on invasive pressure measurement, the feasibility of which is limited in conventional clinical practice [10, 11]. The results of MW index assessment of MW have a strong correlation with the measurement results of invasive cardiac catheterization [12]. This finding confirms the feasibility of the NIMWI for assessing MW. The NIMWI based on 2D speckle tracking technology, which combines myocardial deformation and non-invasive LV pressure to assess MW [7], is more comprehensive than GLS for the assessment of cardiac function in patients with altered afterload, and the technique can detect impaired myocardial function early, and its feasibility has been established in hypertension, hypertrophic cardiomyopathy, dilated cardiomyopathy and cardiac resynchronization [13,14,15,16].
Compared with the normal group, there were no difference in GWI and GCW, but GWW increased and GWE decreased in the uremic group, indicating that a decreased GWE of the left ventricle in uremic patients. GWE is the ratio of GCW to the sum of GCW and GWW, and there is no obvious change in the GCW. Thus, it can be seen that the decrease of GWE is mainly related to the increase of LV GWW. GWW refers to the work done by the left ventricle that is not conducive to ejection, including the total work done by cardinal elongation at systole and cardinal shortening at isovolumic diastole. Any factor affecting myocardial elongation at systole and myocardial shortening at isovolumic diastole may increase GWW. An earlier study [17] demonstrated that several factors in the body of with uremic patients, such as sodium and water retention and renin–angiotensin–aldosterone system activation, participate in the development of hypertension. The presence of long-term high loads leads to increased LV myocardial stiffness, ventricular remodelling, and myocardial oxygen consumption [18, 19]. Luca et al. [20] found that secondary nephritic anaemia in uremic patients aggravates cardinal ischaemia, hypoxia, damages cardinal cells by calcium and phosphorus imbalance, and causes microvascular ischaemia, interstitial fibrosis and cardiac myocyte hypertrophy by long-term haemodialysis-related myocardial stunning. These phenomena negatively affect myocardial contractions, resulting in an increase in global wasted work (GWW), and a decrease in the global work efficiency of the left ventricle.
In this study, GWE and GWW showed a good correlation with SBP, which is consistent with the rationale that the NIMWI technique evaluates myocardial work based on stress and strain. AUC for GWE by the ROC analysis was 0.966, which indicates that the GWE accurately evaluated LV systolic function in uremic patients. The best threshold, sensitivity and specificity values of GWE to detect abnormality of LV systolic function in uremic patients were 92.5%, 0.89 and 0.96, respectively. It can provide some reference values for the early detection of the LV systolic dysfunction in uremic patients with preserved left ventricular ejection fraction..
However, this study had some limitations that should be noted. It was a single-centre study with a relatively small sample size and no long-term follow-up of uremic patients, which will be encompassed in the next phase of the study.
Conclusions
NIMWI may be applied to assess the global MW of uremic patients. AUC, sensitivity, and specificity for GWE parameter by ROC analysis were high, revealing the accuracy of GWE for the detection of the LV systolic dysfunction in the uremic patients. The reproducibility of MW parameters can help to improve its application in clinical practice.
Methods
Study population
A total of 26 uremic patients who were treated in the nephrology department of our hospital from November 2020 to June 2021 were consecutively identified. All uremic patients were treated with regular haemodialysis three times a week and with LVEF ≥ 50% according to the 2016 European Society of Cardiology Guidelines [21]. Patients were excluded if there were valvular disease, LV outflow tract obstruction, arrhythmia, essential hypertension, diabetes, previous myocardial infarction, medium and large pericardial effusion, LV systolic dysfunction with LVEF < 50%, and patients with a poor acoustic window of transthoracic echocardiography, which was mainly manifested as unclear display of endocardium or endocardium located outside the sampling frame.
Twenty-seven healthy volunteers matched for sex, age and body surface area (BSA) were selected as the normal group. All volunteers had no history of heart disease, hypertension, diabetes or medication. Their physical examination, electrocardiogram, chest radiograph, renal function and echocardiography results were normal.
All subjects provided informed consent prior to participating in this study, and the study protocols were approved by the Hospital Ethics Committee. The participant selection process is illustrated in the flowchart in Fig. 3.
Echocardiography
GE Vivid E95 (GE Vingmed Ultrasound AS, Horten, Norway) colour Doppler ultrasound system equipped with M5Sc-D 1.4–4.6 MHz probe was used for echocardiographic image acquisition.
The subjects were instructed to assume the left-lateral position and an electrocardiogram was attached. Transthoracic echocardiography was used to measure the LVEDd, LVPWTd and IVSTd of the participants. The modified biplane Simpson method was used to calculate LVEF from the apical four- and two-chamber views. The LVMI was calculated as LV mass divided by BSA. We obtained the dynamic two-dimensional images from the LV apical four-, two- and three-chamber views at frame rate of 58—69 frames/s (average of 67.4 ± 6 frames/sec) for at least three cardiac cycles in the resting state. The images were copied, saved and exported to the workstation in Digital Imaging and Communication in Medicine (DICOM) format on a mobile hard disk for offline analysis.
All two-dimensional images and measurements were performed according to American Society of Echocardiography guideline [22], and all parameters were averaged over three consecutive cardiac cycles. The SBP and DBP of the participants were measured using a brachial artery cuff.
Two-dimensional speckle tracking image analysis
The stored images were analysed offline by an Echo PAC BT203 (GE Vingmed Ultrasound, Horten, Norway) workstation. The durations of the LV isovolumic systole and ejection period were first determined according to the opening and closing of the aortic and mitral valves, and then the automatic functional imaging mode was selected. The endocardium of the LV long axis, four-chamber and two-chamber view were depicted from the level of the mitral valve annulus to the LV apex in sequence. The software automatically tracked the endocardium and epicardium of the left ventricle. The intracardiac and epicardial wrap were manually adjusted to ensure satisfactory tracking. Finally, Approve was clicked, and the blood pressure measured by the bronchial artery cuff was entered into the MW menu to obtain the LV pressure–strain loops (PSL), GLS and NIMWI. The NIMWI parameters included GWI, GCW, GWW and GWE, as shown in Fig. 4.
Schematic diagram of the NIMWI measurement results. a Changes in systolic blood pressure measured by the cuff as a function of the global longitudinal strain of the left ventricle. Red curve: overall pressure and strain of the left ventricle. The area under curve represents the global myocardial work index of the left ventricle. b Column chart of the global constructive work and waste work of the left ventricle. c Bull’s-eye diagram of the 17-segment myocardial work index of the left ventricle. d Results of the NIMWI parameters. NIMWI: non-invasive myocardial work index
Statistical analysis
All statistical analyses were performed using SPSS version 25.0 (SPSS Inc., IBM, Chicago, USA). Continuous variables were expressed as mean ± standard deviation if normally distributed. Independent-sample t-test was used to compare continuous variables between the uremic group and normal group. The Chi-squared test was used to compare count data. Correlation between continuous variables was carried out using Pearson’s or Spearman’s correlation coefficient as appropriate.
ROC curves were performed to determine the optimal sensitivity and specificity of MW parameter. The AUC was calculated to assess the performance of MW parameter for the detection impaired myocardium in uremic patients. According to the Youden index, the best threshold of each tested MW parameter was estimated. Ten subjects were randomly selected, and two observers used infra-class correlation coefficients to carry out repeatability tests for the myocardial work parameters GWI, GCW, GWW and GWE. A P-value < 0.05 was considered statistically significant.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- NIMWI:
-
Non-invasive myocardial work index
- LV:
-
Left ventricular
- MW:
-
Myocardial work
- GWI:
-
Global work index
- GCW:
-
Global constructive work
- GWW:
-
Global wasted work
- GWE:
-
Global work efficiency
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- CKD:
-
Chronic kidney disease
- LVEF:
-
Left ventricular ejection fraction
- GLS:
-
Global longitudinal strain
- 2D:
-
Two dimensional
- SBP:
-
Systolic blood pressures
- DBP:
-
Diastolic blood pressures
- HR:
-
Heart rate
- BSA:
-
Body surface area
- IVSTd:
-
Interventricular septum end-diastolic thickness
- LVPWTd:
-
Left ventricular posterior wall end-diastolic thickness
- LVEDd:
-
Left ventricular end-diastolic diameter
- LVMI:
-
Left ventricular mass index
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- DICOM:
-
Digital Imaging and Communication in Medicine
- PSL:
-
Pressure–strain loops
References
Yan P, Li H, Hao C, Shi H, Gu Y, Huang G, et al. 2D-speckle tracking echocardiography contributes to early identification of impaired left ventricular myocardial function in patients with chronic kidney disease. Nephron Clin Pract. 2011;118(3):232–40. https://doi.org/10.1159/000321383.
Ma Y, Zhang B, Zhang Y, Dong Y, Zhang R. Ultrasonic image analysis of longitudinal strain in uremic patients with preserved left ventricular ejection fraction. Biomed Eng Online. 2018;17(1):112. https://doi.org/10.1186/s12938-018-0536-y.
Tulner SA, Klautz RJ, van Rijk-Zwikker GL, Engbers FH, Bax JJ, Baan J, et al. Perioperative assessment of left ventricular function by pressure-volume loops using the conductance catheter method. Anesth analg. 2003;97(4):950–7. https://doi.org/10.1213/01.ane.0000078814.81889.b3.
Konstam MA, Abboud FM. Ejection fraction. Circulation. 2017;135(8):717–9. https://doi.org/10.1161/CIRCULATIONAHA.116.025795.
Tops LF, Delgado V, Marsan NA, Bax JJ. Myocardial strain to detect subtle left ventricular systolic dysfunction. Eur J Heart Fail. 2017;19(3):307–13. https://doi.org/10.1002/ejhf.694.
Boe E, Skulstad H, Smiseth OA. Myocardial work by echocardiography: a novel method ready for clinical testing. Eur Heart J Cardiovasc Imaging. 2019;20(1):18–20. https://doi.org/10.1093/ehjci/jey156.
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J. 2012;33(6):724–33. https://doi.org/10.1093/eurheartj/ehs016.
Ke QQ, Xu HB, Bai J, Xiong L, Li MM. Evaluation of global and regional left ventricular myocardial work by echocardiography in patients with chronic kidney disease. Echocardiography. 2020;37(11):1784–91. https://doi.org/10.1111/echo.14864.
Sun M, Kang Y, Cheng L, Pan C, Cao X, Yao H, et al. Global longitudinal strain is an independent predictor of cardiovascular events in patients with maintenance hemodialysis: a prospective study using three-dimensional speckle tracking echocardiography. Int J Cardiovasc Imaging. 2016;32(5):757–66. https://doi.org/10.1007/s10554-016-0836-x.
Foëx P, Leone BJ. Pressure-volume loops: a dynamic approach to the assessment of ventricular function. J Cardiothorac Vasc Anesth. 1994;8(1):84.
Mclaurin LP, Grossman W, Stefadouros MA, Rolett EL, Young DT. A new technique for the study of left ventricular pressure-volume relations in man. Circulation. 1973;48(1):56–64.
Hubert A, Le Rolle V, Leclercq C, Galli E, Samset E, Casset C, et al. Estimation of myocardial work from pressure-strain loops analysis: an experimental evaluation. Eur Heart J Cardiovasc Imaging. 2018;19(12):1372–9. https://doi.org/10.1093/ehjci/jey024.
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, et al. A new approach to assess myocardial work by non-invasive left ventricular pressure–strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2019;20(1):31–9. https://doi.org/10.1093/ehjci/jey131.
Galli E, Vitel E, Schnell F, Le Rolle V, Hubert A, Lederlin M, et al. Myocardial constructive work is impaired in hypertrophic cardiomyopathy and predicts left ventricular fibrosis. Echocardiography. 2019;36(1):74–82. https://doi.org/10.1111/echo.14210.
Cui C, Liu L, Li Y, Liu Y, Huang D, Hu Y, et al. Left ventricular pressure–strain loop based quantitative examination of the global and regional myocardial work of patients with dilated cardiomyopathy. Ultrasound Med Biol. 2020;46(10):2834–45. https://doi.org/10.1016/j.ultrasmedbio.2020.06.008.
Galli E, Leclercq C, Fournet M, Hubert A, Bernard A, Smiseth OA, et al. Value of myocardial work estimation in the prediction of response to cardiac resynchronization therapy. J Am Soc Echocardiogr. 2018;31(2):220–30. https://doi.org/10.1016/j.echo.2017.10.009.
Harrison DG. The Mosaic Theory revisited: common molecular mechanisms coordinating diverse organ and cellular events in hypertension. J Am Soc Hypertens. 2013;7(1):68–74. https://doi.org/10.1016/j.jash.2012.11.007.
Brilla CG, Funck RC, Rupp H. Lisinopril-mediated regression of myocardial fibrosis in patients with hypertensive heart disease. Circulation. 2000;102(12):1388–93.
Kuznetsova T, Hooge D, Kloch-Badelek M, Sakiewicz W, Thijs L, Staessen JA. Impact of hypertension on ventricular–arterial coupling and regional myocardial work at rest and during isometric exercise. J Am Soc Echocardiog. 2012;25(8):882–90. https://doi.org/10.1016/j.echo.2012.04.018.
Di Lullo L, Gorini A, Russo D, Santoboni A, Ronco C. Left ventricular hypertrophy in chronic kidney disease patients: from pathophysiology to treatment. Cardiorenal Med. 2015;5(4):254–66. https://doi.org/10.1159/000435838.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail. 2016;18(8):891–975. https://doi.org/10.1002/ejhf.592.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imag. 2015;16(3):233–71. https://doi.org/10.1093/ehjci/jev014.
Acknowledgements
Not applicable.
Funding
This study was supported by National Natural Science Foundation of China (82071950), National Natural Science Foundation of Henan for Excellent Young Scientists (202300410364), Medical Science and Technology Research Project of Henan Province (SB201901099, LHGJ20200084).
Author information
Authors and Affiliations
Contributions
Performed the literature review: HZZ, YNL; carried out echocardiography measurements: HZZ, YNL, QQZ, YW; selected participants and collected the clinical data: HZZ, YNL, DQH; checked the validity of data: HZZ, YNL, LL; data analysis: HZZ, YNL, YYL; wrote the manuscript: HZZ; prepared the manuscript: YW, RJL; supported the experiments financially: LL; checked the paper: LL, YNL. All authors have checked and confirmed the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Fuwai Central China Cardiovascular Hospital, Henan Provincial People's Hospital, Central China Fuwai Hospital of Zhengzhou University, People's Hospital of Zhengzhou University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhu, H., Li, Y., Cui, C. et al. Non-invasive myocardial work index contributes to early identification of impaired left ventricular myocardial function in uremic patients with preserved left ventricular ejection fraction. BioMed Eng OnLine 21, 57 (2022). https://doi.org/10.1186/s12938-022-01023-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12938-022-01023-5