Abstract
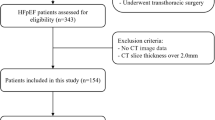
Atrial fibrillation (AF) is the most common arrhythmia and potentially increase the risk of embolic stroke and aggravate progressive heart failure in patients with hypertrophic cardiomyopathy (HCM). Recent studies demonstrated that epicardial adipose tissue (EAT) was closely associated with AF in general population. However, the relationship between EAT and AF in HCM patients remains unclear. A total of 93 consecutive patients with hypertrophic obstructive cardiomyopathy (HOCM) at Fuwai Hospital were enrolled in our study. There were 18 patients with AF and 75 patients without it. Cardiac magnetic resonance (CMR) imaging was performed in all participants. EAT volume (EATV) and left atrial volume (LAV) were determined by E-3D medical model software. HOCM patients with AF had significantly greater EATV index (EATVI, P < 0.001), LAV index (LAVI, P < 0.001) and left ventricular end-systole volume index (LVESVI, P = 0.039), and lower left ventricular ejection fraction (LVEF, P = 0.002). In multivariable logistic regression analysis, EATVI, LAVI, and LVEF remained independent determinants of AF occurrence (OR = 1.023, 95% CI, 1.003–1.043, P = 0.023, OR = 1.043, 95% CI, 1.012–1.075, P = 0.006, and OR = 0.887, 95% CI, 0.818–0.962, P = 0.004, respectively). Furthermore, receiver operating characteristic (ROC) curve analysis demonstrated that integration of EATVI, LAVI and LVEF provided better discriminatory performance for incident AF in HOCM patients with a high sensitivity of 94.4% and a specificity of 69.3% (AUC = 0.864, 95% CI, 0.771–0.958, P < 0.001). EATVI is an independent predictor of the presence of AF, and integration of EATVI, LVEF and LAVI determined by CMR provide greater discriminatory performance for identifying AF in HOCM patients.



Similar content being viewed by others
Data availability
According to the management system of Fuwai Hospital, we are not allowed to share original research data publicly.
References
Maron BJ, Maron MS (2013) Hypertrophic cardiomyopathy. Lancet 381(9862):242–255
Marian AJ, Braunwald E (2017) Hypertrophic cardiomyopathy: genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ Res 121(7):749–770
Veselka J, Anavekar NS, Charron P (2017) Hypertrophic obstructive cardiomyopathy. Lancet 389(10075):1253–1267
Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS et al (2011) 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 124(24):2761–2796
Frontera A, Wilson DG, Sekhon H, Duncan ER, Thomas G (2015) Atrial fibrillation and hypertrophic cardiomyopathy: who to anticoagulate? Clin Res Cardiol 104(10):799–802
Azarbal F, Singh M, Finocchiaro G, Le VV, Schnittger I, Wang P et al (2014) Exercise capacity and paroxysmal atrial fibrillation in patients with hypertrophic cardiomyopathy. Heart 100(8):624–630
Authors/Task Force members, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, et al (2014) 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 35(39):2733–2779
Siontis KC, Geske JB, Ong K, Nishimura RA, Ommen SR, Gersh BJ (2014) Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations, and mortality in a large high-risk population. J Am Heart Assoc 3(3):e001002
Jermendy AL, Kolossvary M, Drobni ZD, Tarnoki AD, Tarnoki DL, Karady J et al (2018) Assessing genetic and environmental influences on epicardial and abdominal adipose tissue quantities: a classical twin study. Int J Obes (Lond) 42(2):163–168
Iacobellis G, Barbaro G (2019) Epicardial adipose tissue feeding and overfeeding the heart. Nutrition 59:1–6
Iacobellis G, Bianco AC (2011) Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab 22(11):450–457
Oikonomou EK, Antoniades C (2019) The role of adipose tissue in cardiovascular health and disease. Nat Rev Cardiol 16(2):83–99
Mancio J, Oikonomou EK, Antoniades C (2018) Perivascular adipose tissue and coronary atherosclerosis. Heart 104(20):1654–1662
Wang TD, Lee WJ, Shih FY, Huang CH, Chen WJ, Lee YT et al (2010) Association of epicardial adipose tissue with coronary atherosclerosis is region-specific and independent of conventional risk factors and intra-abdominal adiposity. Atherosclerosis 213(1):279–287
Bakkum MJ, Danad I, Romijn MA, Stuijfzand WJ, Leonora RM, Tulevski II et al (2015) The impact of obesity on the relationship between epicardial adipose tissue, left ventricular mass and coronary microvascular function. Eur J Nucl Med Mol Imaging 42(10):1562–1573
Ng ACT, Strudwick M, van der Geest RJ, Ng ACC, Gillinder L, Goo SY et al (2018) Impact of epicardial adipose tissue, left ventricular myocardial fat content, and interstitial fibrosis on myocardial contractile function. Circ Cardiovasc Imaging 11(8):e007372
Wong CX, Ganesan AN, Selvanayagam JB (2017) Epicardial fat and atrial fibrillation: current evidence, potential mechanisms, clinical implications, and future directions. Eur Heart J 38(17):1294–1302
Nagueh SF, Bierig SM, Budoff MJ, Desai M, Dilsizian V, Eidem B et al (2011) American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with hypertrophic cardiomyopathy: endorsed by the American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr 24(5):473–498
Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA et al (2013) Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 14(7):611–644
Chaowu Y, Shihua Z, Jian L, Li L, Wei F (2013) Cardiovascular magnetic resonance characteristics in children with hypertrophic cardiomyopathy. Circ Heart Fail 6(5):1013–1020
Ansaldo AM, Montecucco F, Sahebkar A, Dallegri F, Carbone F (2019) Epicardial adipose tissue and cardiovascular diseases. Int J Cardiol 278:254–260
Mahajan R, Kuklik P, Grover S, Brooks AG, Wong CX, Sanders P et al (2013) Cardiovascular magnetic resonance of total and atrial pericardial adipose tissue: a validation study and development of a 3 dimensional pericardial adipose tissue model. J Cardiovasc Magn Reson 15:73
Nakamori S, Nezafat M, Ngo LH, Manning WJ, Nezafat R (2018) Left atrial epicardial fat volume is associated with atrial fibrillation: a prospective cardiovascular magnetic resonance 3D Dixon study. J Am Heart Assoc 7(6):e008232
Gaborit B, Sengenes C, Ancel P, Jacquier A, Dutour A (2017) Role of epicardial adipose tissue in health and disease: a matter of fat? Compr Physiol 7(3):1051–1082
Packer M (2018) Epicardial adipose tissue may Mediate deleterious effects of obesity and inflammation on the myocardium. J Am Coll Cardiol 71(20):2360–2372
Samanta R, Pouliopoulos J, Thiagalingam A, Kovoor P (2016) Role of adipose tissue in the pathogenesis of cardiac arrhythmias. Heart Rhythm 13(1):311–320
Patel VB, Shah S, Verma S, Oudit GY (2017) Epicardial adipose tissue as a metabolic transducer: role in heart failure and coronary artery disease. Heart Fail Rev 22(6):889–902
Thanassoulis G, Massaro JM, O’Donnell CJ, Hoffmann U, Levy D, Ellinor PT et al (2010) Pericardial fat is associated with prevalent atrial fibrillation: the Framingham Heart Study. Circ Arrhythm Electrophysiol 3(4):345–350
Al Chekakie MO, Welles CC, Metoyer R, Ibrahim A, Shapira AR, Cytron J et al (2010) Pericardial fat is independently associated with human atrial fibrillation. J Am Coll Cardiol 56(10):784–788
Batal O, Schoenhagen P, Shao M, Ayyad AE, Van Wagoner DR, Halliburton SS et al (2010) Left atrial epicardial adiposity and atrial fibrillation. Circ Arrhythm Electrophysiol 3(3):230–236
Wong CX, Abed HS, Molaee P, Nelson AJ, Brooks AG, Sharma G et al (2011) Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J Am Coll Cardiol 57(17):1745–1751
Nagashima K, Okumura Y, Watanabe I, Nakai T, Ohkubo K, Kofune T et al (2011) Association Between epicardial adipose tissue volumes on 3-dimensional reconstructed CT images and recurrence of atrial fibrillation after catheter ablation. Circ J 75(11):2559–2565
Marrouche NF, Wilber D, Hindricks G, Jais P, Akoum N, Marchlinski F et al (2014) Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA 311(5):498–506
Peters DC, Wylie JV, Hauser TH, Nezafat R, Han Y, Woo JJ et al (2009) Recurrence of atrial fibrillation correlates with the extent of post-procedural late gadolinium enhancement: a pilot study. JACC Cardiovasc Imaging 2(3):308–316
Acknowledgements
We thank Shenghui Liao (Central South University, Changsha, China) for offer of E-3D medical model software.
Funding
This work was supported by National Key Research and Development Program of China (No. 2018YFB1107102).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All of authors declare that there is no conflict of interest.
Ethical approval
Approval of Ethics Committee of Fuwai Hospital was acquired at the beginning of the study.
Informed consent
Informed consents were written by each participant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, Y., Yu, M., Cui, J. et al. The predictive value of epicardial adipose tissue volume assessed by cardiac magnetic resonance for atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy. Int J Cardiovasc Imaging 37, 1383–1393 (2021). https://doi.org/10.1007/s10554-020-02092-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02092-0