Abstract
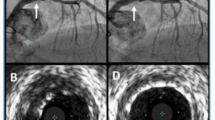
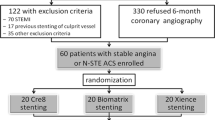
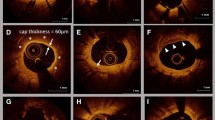
The purpose of this study was to clarify a cut-off value for acute incomplete stent apposition (ISA) volume and maximum-depth to predict ISA resolution at 1- and 3-month follow-up in patients treated with cobalt–chromium everolimus-eluting stents. In total, 95 cases and 103 stents were registered in the MECHANISM-Elective sub-study. Acute ISA-volume was measured by the trapezoid rule. ISA resolution of cut-off value at 1- and 3-month was estimated by ISA-volume and maximum-depth using receiver operatorating characteristic curve analysis. The total number of analysed acute ISAs was 202 in the 1-month group and 225 in the 3-month group. A total of 123 ISAs at 1-month and a total of 169 ISAs at 3-month had been resolved. The cut-off value of ISA resolution by ISA-volume was 0.169 mm3 at 1-month (AUC: 0.725, sensitivity: 72.2%, specificity: 61.0%) and 0.295 mm3 at 3-month (AUC: 0.757, sensitivity: 75.0%, specificity: 60.4%). The cut-off value of ISA resolution by ISA maximum-depth demonstrated was 0.285 mm at 1-month (area under curve (AUC): 0.789, sensitivity: 70.9%, specificity: 69.9%) and 0.305 mm at 3-month (AUC: 0.663, sensitivity: 60.7%, specificity: 66.9%). Incidence of ISA resolution was significantly lower in combination with cut-off values of ISA-volume and maximum-depth (33%, p < 0.001, at 1-month; 56%, p = 0.003, at 3-month). Combining the cut-off value of ISA-volume with the maximum-depth might be helpful to consider the endpoint of the PCI procedure.








Similar content being viewed by others
References
Giustino G, Baber U, Sartori S et al (2015) Duration of dual antiplatelet therapy after drug-eluting stent implantation: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Cardiol 65:1298–1310. https://doi.org/10.1016/j.jacc.2015.01.039
Stefanini GG, Siontis GC, Cao D et al (2014) Short versus long duration of DAPT after DES implantation: a meta-analysis. J Am Coll Cardiol 64:953–954. https://doi.org/10.1016/j.jacc.2014.06.1158
Kirac D, Erdem A, Avcilar T et al. (2016) Effects of genetic factors to stent thrombosis due to clopidogrel resistance after coronary stent placement. Cell Mol Biol (Noisy-le-grand) 62:51–55
Guagliumi G, Musumeci G, Sirbu V et al (2010) Optical coherence tomography assessment of in vivo vascular response after implantation of overlapping bare-metal and drug-eluting stents. JACC Cardiovasc Interv 3:531–539. https://doi.org/10.1016/j.jcin.2010.02.008
Finn AV, Nakazawa G, Joner M et al (2007) Vascular responses to drug eluting stents: importance of delayed healing. Arterioscler Thromb Vasc Biol 27:1500–1510. https://doi.org/10.1161/atvbaha.107.144220
Nakazawa G, Finn AV, Joner M et al (2008) Delayed arterial healing and increased late stent thrombosis at culprit sites after drug-eluting stent placement for acute myocardial infarction patients: an autopsy study. Circulation 118:1138–1145. https://doi.org/10.1161/circulationaha.107.762047
Karalis I, Ahmed TA, Jukema JW (2012) Late acquired stent malapposition: why, when and how to handle? Heart 98:1529–1536. https://doi.org/10.1136/heartjnl-2011-301220
Ozaki Y, Okumura M, Ismail TF et al (2010) The fate of incomplete stent apposition with drug-eluting stents: an optical coherence tomography-based natural history study. Eur Heart J 31:1470–1476. https://doi.org/10.1093/eurheartj/ehq066
Kawamori H, Shite J, Shinke T et al (2013) Natural consequence of post-intervention stent malapposition, thrombus, tissue prolapse, and dissection assessed by optical coherence tomography at mid-term follow-up. Eur Heart J Cardiovasc Imaging 14:865–875. https://doi.org/10.1093/ehjci/jes299
Inoue T, Shinke T, Otake H et al (2014) Impact of strut-vessel distance and underlying plaque type on the resolution of acute strut malapposition: serial optimal coherence tomography analysis after everolimus-eluting stent implantation. Int J Cardiovasc Imaging 30:857–865. https://doi.org/10.1007/s10554-014-0422-z
Prati F, Di Vito L, Biondi-Zoccai G et al (2012) Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the centro per la lotta contro l'infarto-optimisation of percutaneous coronary intervention (CLI-OPCI) study. Euro Interv 8:823–829. https://doi.org/10.4244/eijv8i7a125
Izumi D, Miyahara M, Fujimoto N et al (2016) Optical coherence tomography analysis of the stent strut and prediction of resolved strut malapposition at 3 months after 2nd-generation drug-eluting stent implantation. Heart Vessels 31:1247–1256. https://doi.org/10.1007/s00380-015-0737-2
Shimamura K, Kubo T, Akasaka T et al (2015) Outcomes of everolimus-eluting stent incomplete stent apposition: a serial optical coherence tomography analysis. Eur Heart J Cardiovasc Imaging 16:23–28. https://doi.org/10.1093/ehjci/jeu174
Im E, Kim BK, Ko YG et al (2014) Incidences, predictors, and clinical outcomes of acute and late stent malapposition detected by optical coherence tomography after drug-eluting stent implantation. Circ Cardiovasc Interv 7:88–96. https://doi.org/10.1161/circinterventions.113.000797
Taguchi Y, Itoh T, Oda H et al (2017) Coronary risk factors associated with OCT macrophage images and their response after CoCr everolimus-eluting stent implantation in patients with stable coronary artery disease. Atherosclerosis 265:117–123. https://doi.org/10.1016/j.atherosclerosis.2017.08.002
Gutierrez-Chico JL, Wykrzykowska J, Nuesch E et al (2012) Vascular tissue reaction to acute malapposition in human coronary arteries: sequential assessment with optical coherence tomography. Circ Cardiovasc Interv 5:20–29. https://doi.org/10.1161/circinterventions.111.965301
Otsuka F, Cheng Q, Yahagi K et al (2015) Acute thrombogenicity of a durable polymer Everolimus-eluting stent relative to contemporary drug-eluting stents with biodegradable polymer coatings assessed ex vivo in a swine shunt model. JACC Cardiovasc Interv 8:1248–1260. https://doi.org/10.1016/j.jcin.2015.03.029
Kolandaivelu K, Swaminathan R, Gibson WJ et al (2011) Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings. Circulation 123:1400–1409. https://doi.org/10.1161/circulationaha.110.003210
Sabate M, Cequier A, Iniguez A et al (2012) Everolimus-eluting stent versus bare-metal stent in ST-segment elevation myocardial infarction (EXAMINATION): 1 year results of a randomised controlled trial. Lancet 380:1482–1490. https://doi.org/10.1016/s0140-6736(12)61223-9
Kim WH, Lee BK, Lee S et al (2010) Serial changes of minimal stent malapposition not detected by intravascular ultrasound: follow-up optical coherence tomography study. Clin Res Cardiol 99:639–644. https://doi.org/10.1007/s00392-010-0163-5
Takarada S, Imanishi T, Liu Y et al (2010) Advantage of next-generation frequency-domain optical coherence tomography compared with conventional time-domain system in the assessment of coronary lesion. Catheter Cardiovasc Interv 75:202–206. https://doi.org/10.1002/ccd.22273
Okamura T, Onuma Y, Garcia-Garcia HM et al (2011) First-in-man evaluation of intravascular optical frequency domain imaging (OFDI) of Terumo: a comparison with intravascular ultrasound and quantitative coronary angiography. Euro Interv 6:1037–1045. https://doi.org/10.4244/eijv6i9a182
Fedele S, Biondi-Zoccai G, Kwiatkowski P et al (2012) Reproducibility of coronary optical coherence tomography for lumen and length measurements in humans (The CLI-VAR [Centro per la Lotta contro l'Infarto-VARiability] study). Am J Cardiol 110:1106–1112. https://doi.org/10.1016/j.amjcard.2012.05.047
Mintz GS (2007) What to do about late incomplete stent apposition? Circulation 115:2379–2381. https://doi.org/10.1161/circulationaha.107.697136
Acknowledgements
The authors are deeply grateful to the core-analysis laboratory members: Kanako Omiya and Yumiko Okuyama (ARCHIMEDES (The Academic ResearCH Group for Exploring Undiscovered Mechanisms of Cardiovascular DiseasES), Kayoko Fujiwara (secretary, ICAL) and Tatsuya Shinke (image technician, ICAL).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tomonori Itoh: Lecture honoraria (Daiichi-Sankyo, Abbott Vascular Japan). Hiromasa Otake: Lecture honoraria (Abbott Vascular Japan). Yoshihiro Morino: Research grant (Daiichi Sankyo), Lecture honoraria (Daiichi-Sankyo, Abbott Vascular). Toshiro Shinke: Research grant (Daiichi-Sankyo), Lecture honoraria (Daiichi Sankyo, Abbott Vascular). Any other authors do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uchimura, Y., Itoh, T., Oda, H. et al. Cut-off value of mal-apposition volume and depth for resolution at early phase of acute incomplete stent apposition after CoCr-EES implantation. Int J Cardiovasc Imaging 35, 1979–1987 (2019). https://doi.org/10.1007/s10554-019-01657-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01657-y