Abstract
Heart failure with preserved ejection fraction (HFpEF) is common in systemic sclerosis (SSc) and implies a worse prognosis therefore non-invasive assessment of left ventricular (LV) filling pressure is pivotal. Besides E/eʹ the use of maximal left atrial volume (LA Vmax index) is recommended. LA reservoir strain was also reported to be useful. The utility of LA stiffness, however, was never investigated in SSc. Thus we aimed to compare the diagnostic power of LA Vmax index, reservoir strain and stiffness in predicting elevated LV filling pressure in SSc patients. 72 SSc patients (age: 57 ± 11 years) were investigated. LA stiffness was calculated as ratio of E/eʹ to LA reservoir strain. Elevated LV filling pressure was defined as NT-proBNP > 220 pg/ml. Receiver-operating characteristic (ROC) curves were used to estimate the diagnostic performance of the investigated parameters. Average NT-proBNP level was 181 ± 154 pg/ml. NT-proBNP > 220 pg/ml was found in 21 SSc patients. LA stiffness showed the highest diagnostic performance in predicting NT-pro-BNP > 220 pg/ml, with a cut off value of 0.314 (Area under the curve: 0.719, specificity: 89.4%, sensitivity: 42.1%). AUC values for LA reservoir strain and Vmax index were 0.595 and 0.521, respectively. LA stiffness was superior to Vmax index and reservoir strain in predicting elevated NT-proBNP levels in SSc patients. Although invasive validation studies on larger samples are required, our data suggest, that the use of LA stiffness may significantly contribute to diagnostic precision in populations with a high suspicion of HFpEF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac involvement is an important adverse finding in systemic sclerosis (SSc). Epidemiologic studies show that it is responsible for 20–30% of all premature deaths in these patients [1]. Left ventricular (LV) systolic dysfunction is not common in SSc [2]. Diastolic dysfunction and the consequential heart failure with preserved ejection fraction (HFpEF) are much more frequent as they reflect the primary myocardial involvement of the disease [3]. These factors are also proved to be associated with increased risk of mortality [4,5,6]. Thus assessment of LV diastolic function and filling pressure has important diagnostic and prognostic implications in SSc. In addition to the invasive measurements, N-terminal pro-brain natriuretic peptide (NT-proBNP) levels provide reliable estimation of elevated LV filling pressure [7,8,9]. In the everyday practice, however, echocardiography is used for this purpose. The E/eʹ ratio is the most thoroughly studied index characterizing LV filling pressure and is included into the algorithms of all the relevant authoritative documents [10,11,12]. Nevertheless, recent studies have challenged the accuracy of E/eʹ in patients with or at risk for HFpEF [13,14,15,16,17]. Thus additional echocardiographic parameters are also required for identifying elevated LV filling pressure. The current recommendations suggest the use of the maximal left atrial (LA) volume index [12], as it is a reliable indicator of the duration and severity of the elevated filling pressure [18]. Recent studies proved, however, that 2-dimensional speckle tracking-derived LA reservoir strain also shows a good correlation with LV filling pressure [19,20,21], exceeding the diagnostic power of the maximal LA volume [22, 23]. LA stiffness is a further parameter of the atrial performance, representing the change in pressure required to increase the volume of the atrium in a given measure [24, 25]. It was reported as a useful index to distinguish HFpEF patients from those with asymptomatic diastolic dysfunction [25].
Thus we aimed to compare the diagnostic power of the maximal LA volume index, LA reservoir strain and LA stiffness in predicting elevated LV filling pressure in SSc patients. NT-proBNP served as non-invasive measure of the LV filling pressure in our study.
Methods
Study population
Our prospective study included 80 consecutive SSc patients diagnosed in the tertiary centre of the Department of Rheumatology and Immunology, University of Pécs. All enrolled patients needed to comply the American College of Rheumatology criteria for SSc and were categorized as suffering from limited cutaneous or diffuse cutaneous SSc according to the criteria defined by LeRoy et al. [26]. All patients fulfilled the recently revised ACR/EULAR classification criteria [27]. We performed extensive assessment of the medical history. Subjects with atrial fibrillation, pulmonary arterial hypertension, known coronary artery disease, cardiomyopathies or significant left sided valvular disease were excluded from our study. Time between the beginning of the first non-Raynaud symptom of SSc and the echocardiographic analysis was defined as duration of the disease. Limitations of physical activity were graded according to the New York Heart Association classification. 6-minute walk test was carried out on the same day as the echocardiographic measurements. All work was done in compliance with the Declaration of Helsinki and was performed with the approval of the institutional ethics committee. Written informed consent was obtained from all patients.
NT-proBNP measurements
Blood samples were obtained immediately prior to the echocardiographic studies. Plasma concentrations of NT-proBNP were analysed by electrochemiluminescence immunoassay (Elecsys 2010 system,Roche Diagnostics, Mannheim, Germany). NT-proBNP value > 220 pg/ml was defined as the evidence of the elevated LV filling pressure [10].
Echocardiography
All patients underwent echocardiographic examination performed by a single investigator using Philips EPIQ 7 ultrasound system (Philips Healthcare, Best, The Netherlands). LV ejection fraction was calculated by biplane Simpson’s method. In addition to the LV end-diastolic diameter, end-diastolic thickness of the septum and posterior wall were measured from parasternal long axis view, using M-mode. LV mass was calculated based on the Devereux formula and then indexed for body surface area (LVM index) [28]. Mitral regurgitation was evaluated according to the recent guidelines and categorized as mild, moderate, or severe [29]. Transmitral flow velocities (E, A) as well as myocardial systolic (S), early-(eʹ) and late-(aʹ) diastolic velocities were measured at the lateral and septal border of the mitral annulus. Lateral and septal myocardial velocities were averaged. Mitral E/A and E/eʹ ratios were computed. E/eʹ > 14 was regarded as elevated, while values between 10 and 14 were considered as “grey zone” values [12]. Systolic pulmonary artery pressure (PASP) was calculated from tricuspid regurgitation velocity added to the right atrial pressure (5 to 15 mmHg) estimated using the diameter and collapsibility index of the inferior vena cava [28]. Doppler measurements were acquired from ≥ 3 consecutive heart cycles.
Strain measurements
LA-focused two-dimensional echocardiographic images were obtained from apical four-, and two-chamber views for speckle tracking analysis. Care was taken to obtain true apical images and to avoid foreshortening. The frame rate was set between 80 and 90 frames/s to ensure adequate speckle-tracking. For each view three cardiac cycles were recorded and stored. A dedicated software (QLab, Philips Healthcare, Andover, MA, USA) was used for offline analysis by a single investigator, blinded to the echocardiographic and clinical data. In segments with insufficient tracking, manual readjustment of the endocardial border was applied to optimize tracking quality. The onset of R-wave on the electrocardiographic trace was used as zero-reference point of the strain analysis. LA reservoir strain was defined as the peak systolic strain, just before mitral valve opening. This was followed by a plateau and a second late peak at the onset of the P-wave indicating the contractile strain. Conduit strain was calculated as the difference between reservoir and contractile strain (Fig. 1a). Data obtained in the two views were averaged [30]. LA stiffness was calculated as ratio of E/eʹ to LA reservoir strain [24, 25].
Four-chamber view image depicting the analysis of LA strain using speckle tracking technique. The region of interest is optimized manually, and then LA strain curve is created by the speckle-tracking software (a). Using the atrial borders created for speckle tracking analysis, LA volume curves are generated by the same software (b). εR Reservoir strain, εCD conduit strain, εCT contractile strain, Vmax maximal volume, Vmin minimal volume, Vp volume at the beginning of P wave)
Volumetric measurements
LA volume curves were generated by the same software using the endocardial borders created for speckle tracking analysis. The following LA volumes were obtained: maximal LA volume (Vmax) at the end of the T-wave on the electrocardiogram, just before the mitral valve opening; minimal LA volume (Vmin) at the QRS complex, just after the mitral valve closure; and volume at atrial contraction (Vp) at the beginning of P-wave (Fig. 1b). Values from the two views were averaged and indexed for body surface area (Vmax-, Vmin- and Vp index) [31].
Statistical analysis
Categorical data were expressed as frequencies and percentages; continuous data were expressed as the mean ± SD. Comparisons of data between two groups were performed using independent-sample t-tests or independent Mann–Whitney test for continuous variables and chi square tests for categorical variables.
Since concentration of NT-proBNP did not show normal distribution, logarithmic transformation was performed. Relationship between lnNTproBNP and the investigated echocardiographic parameters was assessed using linear regression analysis. Potential determinants of the NT-proBNP level (age, body surface area, estimated glomerular filtration rate, LV ejection fraction, and duration of the disease) were also included into the analysis. In the second step, multiple stepwise linear regression analysis was performed, by entering those variables with p < 0.1 in the univariate analysis. Variance Inflation Factor (VIF) values above 2.5 were considered to have potential multicollinearity.
Receiver-operating characteristic (ROC) curves were used to examine the diagnostic performance of the echocardiographic parameters in predicting elevated LV filling pressure. Area under the curve (AUC) values were calculated. Sensitivity and specificity were computed for LA stiffness using various possible cut-off points.
Intraobserver and interobserver variability was assessed by the intraclass correlation coefficient. A p value of < 0.05 was considered significant. Data were analysed using IBM SPSS 22 statistical software.
Results
From the total cohort of 80 participants, 72 were eligible for the study. Eight patients were excluded due to LA foreshortening (n = 3), or inadequate acoustic window (n = 5). Intraclass correlation coefficients for intraobserver variability were 0.982, 0.945, 0.908, 0.944, 0.903, and 0.913 for reservoir, conduit and contractile strain, and Vmax, Vp, and Vmin, respectively. Regarding interobserver variability, intraclass correlation coefficients for reservoir, conduit and contractile strain, and Vmax, Vp, and Vmin were 0.974, 0.932, 0.898, 0.931, 0.899 and 0.882, respectively. The mean age was 57.1 ± 11.3 years, 66 (92%) were female. LV ejection fraction was preserved (≥ 55%) in 70 (97%) and mildly reduced (45–54%) in 2 (3%) patients. Detailed clinical and echocardiographic data of the 72 patients are reported in Table 1. NT-proBNP > 220 pg/ml was found in 21 (29%) patients. Characteristics of our study cohort stratified by this NT-proBNP level are shown in Table 1.
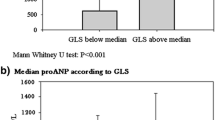
Patients with elevated NT-proBNP levels were significantly older and their walking distance was significantly shorter compared with the other subgroup. The course of the SSc was significantly longer in this population. The difference in LV ejection fraction was clinically not remarkable. Significantly higher E/eʹ values were found in the patients with elevated NT-proBNP levels: E/eʹ > 14 was found in 5 (24%) patients, while in 10 (48%) patients E/eʹ values were in the “grey zone” (between 10 and 14) in this subgroup. LA Vmax index and reservoir strain values were similar in the two subgroups. LA stiffness, on the other hand, was significantly elevated in the subgroup of patients with high NT-proBNP values.
Univariate and multivariate predictors of the NT-proBNP level are reported in Table 2. In stepwise multiple linear regression analysis estimated glomerular filtration rate, LA stiffness and LV ejection fraction became independent predictors of the NT-proBNP level (multiple r = 0.614; p = 0.000; F = 13.537). VIF values for all variables were below 2.5.
Using ROC analysis, LA stiffness showed the highest diagnostic performance in predicting NT-pro-BNP > 220 pg/ml, with an AUC of 0.719. ROC curves demonstrating the predictive power of the three LA parameters are presented in Fig. 2.
Sensitivity and specificity values were computed for LA stiffness using various possible cut-off points (Fig. 3). LA stiffness with the cutoff value of 0.314 showed a high specificity (89.4%) in predicting NT-pro-BNP > 220 pg/ml, with a sensitivity of 42.1%.
Discussion
The main finding of our study is that LA stiffness is superior to volume and strain parameters in predicting elevated NT-proBNP levels in patients with SSc.
Overt LV systolic dysfunction is rare in SSc [2]. Still, heart failure is a typical manifestation of the cardiac involvement in this disease. Primary myocardial involvement is thought to be the consequence of the repeated focal ischemic injuries resulting in irreversible myocardial fibrosis [3, 32]. If myocardial fibrosis progresses, diastolic compliance of the LV decreases and manifest HFpEF may evolve. Numerous characteristic symptoms of SSc patients (impaired functional capacity, dyspnoea, peripheral oedema) are definitely related to LV diastolic dysfunction and elevated filling pressure. In addition, these factors are proved to be associated with increased risk of mortality [4,5,6]. Heart failure symptoms in SSc, however, may be misinterpreted as pulmonary arterial hypertension or interstitial lung disease, leaving HFpEF underdiagnosed. A diagnostic hallmark of heart failure is elevated LV filling pressure, a compensatory response to sustain cardiac output. Thus assessment of LV filling pressure has important diagnostic and prognostic implications in this disease. Although cardiac catheterization remains the gold standard and elevated NT-proBNP levels may also be useful, echocardiography is usually the first test to perform. Thus there is a continuing search for non-invasive markers of elevated LV filling pressure. The previously used parameters have several limitations and reflect different physiological aspects of the diastole. E/eʹ—the ratio of the early diastolic velocity of the mitral inflow to early diastolic velocity of the mitral annulus—provides a close approximation of LV filling pressures in a wide spectrum of diseases and its prognostic value has also been proved. Nevertheless, strength of correlation between E/eʹ and LV filling pressure varied widely between studies [13,14,15,16,17]. Particularly weak correlations were observed in the so called grey zone (average E/eʹ between 10 and 14 [12]; septal E/eʹ between 8 and 15 [33]; lateral E/eʹ between 8 and 12 [34]). Thus additional echocardiographic parameters are also required for identifying elevated LV filling pressure. When indexed to body surface area, maximal LA volume has been proposed as a biomarker of the severity and duration of the elevated filling pressure, especially in patients without significant valvular heart disease or history of atrial fibrillation [18]. It has also been reported as an independent predictor of the cardiovascular outcome in the general population [35] and in SSc [5]. Increased LA volume is also known as an independent predictor of raised NT-proBNP levels in HFpEF patients [36]. Thus the current recommendation of the American Society of Echocardiography and the European Association of Cardiovascular Imaging suggests the use of maximal LA volume index as additional parameter for the evaluation of LV filling pressure [12].
Recent studies proved, however, that the enlargement of the cavity is preceded by the functional remodelling of the LA [37,38,39]. Two-dimensional speckle tracking-derived LA reservoir strain showed significant correlation with the amount of LA wall fibrosis as assessed by cardiac magnetic resonance imaging and with LA interstitial fibrosis in patients with mitral valve disease in histopathologic specimens [40, 41]. This parameter showed a good correlation with the invasively measured LV filling pressure and with NT-proBNP levels, exceeding the diagnostic power of the maximal LA volume [20,21,22,23, 38]. It was also proved to be superior to LA volume as predictor of the cardiovascular events [42]. By the help of the same technique it has been reported by our group that impaired LA mechanics was an early sign of myocardial involvement in SSc, strongly reflecting the changes in LV diastolic function [37].
In our recent study, beside LA reservoir strain, we applied a further parameter of the atrial performance, LA stiffness, which has never been investigated in SSc before. This parameter is obtained by tissue Doppler and speckle tracking techniques and represents the change in pressure required to increase the volume of the atrium in a given measure [24, 25]. Kurt et al. reported LA stiffness as a useful index to differentiate between HFpEF and asymptomatic diastolic dysfunction [25]. In the study of Pilichowska-Paszkiet et al. LA fibrosis was detected by electroanatomical mapping in patients with atrial fibrillation. LA stiffness showed more robust correlation with the extent of LA fibrosis compared with LA strain [43].
Thus in our study we aimed to compare the diagnostic power of the maximal LA volume, LA reservoir strain and LA stiffness in predicting elevated LV filling pressure in SSc patients. The cut-off value of NT-proBNP > 220 pg/ml is considered to have a high positive predictive value for the diagnosis of HFpEF [10], therefore NT-proBNP served as non-invasive measure of the LV filling pressure.
Our data show that LA stiffness has higher discriminative strength in identifying patients with elevated NT-proBNP levels compared with maximal LA volume index and LA reservoir strain. Two parameters, both reflecting LV filling pressure but obtained by completely different approaches, are combined in LA stiffness. This may explain the diagnostic efficacy of this parameter. The common principle of the previous and current echocardiographic recommendations is that cut-off values with high specificity are used to avoid false positive diagnoses of diastolic dysfunction and elevated filling pressure [12, 44]. Thus we suggest the use LA stiffness with the cut-off value of 0.314 as this value showed high specificity (with modest sensitivity) in predicting elevated LV filling pressures.
Although invasive validation studies on larger samples are required, our data suggest, that LA stiffness is superior to maximal LA volume index and LA reservoir strain and may be used as one of the reliable echocardiographic parameters in recognizing SSc patients with elevated LV filling pressure.
Limitations
Numerous limitations of our study need to be acknowledged. For obtaining LA strain values, we used a software that was developed for LV strain analysis because a dedicated software for atrial strain estimation was not available. Besides, larger sample size and prospective follow-up are needed to assess the prognostic impact of the elevated LA stiffness in SSc population. The major limitation of our study was that instead of measuring LV filling pressure invasively, it was estimated using NT-proBNP, which is known to have limited applicability in this context.
Conclusion
LA stiffness was superior to maximal LA volume index and LA reservoir strain in predicting elevated NT-proBNP levels in our SSc patients. Although invasive validation studies on larger samples are required, our data suggest, that the use of LA stiffness may significantly contribute to diagnostic precision in populations with a high suspicion of HFpEF.
References
Komócsi A, Vorobcsuk A, Faludi R et al (2012) The impact of cardiopulmonary manifestations on the mortality of SSc: a systematic review and meta-analysis of observational studies. Rheumatology (Oxford) 51:1027–1036
Allanore Y, Meune C, Vonk MC et al (2010) Prevalence and factors associated with left ventricular dysfunction in the EULAR Scleroderma Trial and Research group (EUSTAR) database of patients with systemic sclerosis. Ann Rheum Dis 69:218–221
Kahan A, Allanore Y (2006) Primary myocardial involvement in systemic sclerosis. Rheumatology (Oxford) 45:iv14–iv17
Hinchcliff M, Desai CS, Varga J et al (2012) Prevalence, prognosis, and factors associated with left ventricular diastolic dysfunction in systemic sclerosis. Clin Exp Rheumatol 30:S30–S37
Faludi R, Költő G, Bartos B et al (2014) Five-year follow-up of left ventricular diastolic function in systemic sclerosis patients: determinants of mortality and disease progression. Semin Arthritis Rheum 44:220–227
Tennøe AH, Murbræch K, Andreassen JC et al (2018) Left ventricular diastolic dysfunction predicts mortality in patients with systemic sclerosis. J Am Coll Cardiol 72:1804–1813
Bansal M, Marwick TH (2008) Natriuretic peptides and filling pressure at rest and stress. Heart Fail Clin 4:71–86
Parsonage WA, Galbraith AJ, Koerbin GL et al (2005) Value of B-type natriuretic peptide for identifying significantly elevated pulmonary artery wedge pressure in patients treated for established chronic heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 95:883–885
Tschöpe C, Kasner M, Westermann D et al (2005) The role of NT-proBNP in the diagnostics of isolated diastolic dysfunction: correlation with echocardiographic and invasive measurements. Eur Heart J 26:2277–2284
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28:2539–2550
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37:2129–2200
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 29:277–314
Lancellotti P, Galderisi M, Edvardsen T et al (2017) Echo-Doppler estimation of left ventricular filling pressure: results of the multicentre EACVI Euro-Filling study. Eur Heart J Cardiovasc Imaging 18:961–968
Obokata M, Borlaug BA (2018) The strengths and limitations of E/eʹ in heart failure with preserved ejection fraction. Eur J Heart Fail 20:1312–1314
Nauta JF, Hummel YM, van der Meer P et al (2018) Correlation with invasive left ventricular filling pressures and prognostic relevance of the echocardiographic diastolic parameters used in the 2016 ESC heart failure guidelines and in the 2016 ASE/EACVI recommendations: a systematic review in patients with heart failure with preserved ejection fraction. Eur J Heart Fail 20:1303–1311
Santos M, Rivero J, McCullough SD et al (2015) E/eʹ ratio in patients with unexplained dyspnea: lack of accuracy in estimating left ventricular filling pressure. Circ Heart Fail 8:749–756
Sharifov OF, Schiros CG, Aban I et al (2016) Diagnostic accuracy of tissue Doppler index E/eʹ for evaluating left ventricular filling pressure and diastolic dysfunction/heart failure with preserved ejection fraction: a systematic review and meta-analysis. J Am Heart Assoc 5:e002530
Douglas PS (2003) The left atrium. J Am Coll Cardiol 42:1206–1207
Singh A, Medvedofsky D, Mediratta A et al (2018) Peak left atrial strain as a single measure for the non-invasive assessment of left ventricular filling pressures. Int J Cardiovasc Imaging 35:23–32. https://doi.org/10.1007/s10554-018-1425-y
Cameli M, Sparla S, Losito M et al (2016) Correlation of left atrial strain and Doppler measurements with invasive measurement of left ventricular end-diastolic pressure in patients stratified for different values of ejection fraction. Echocardiography 33:398–405
Wakami K, Ohte N, Asada K et al (2009) Correlation between left ventricular end-diastolic pressure and peak left atrial wall strain during left ventricular systole. J Am Soc Echocardiogr 22:847–851
Lundberg A, Johnson J, Hage C et al (2018) Left atrial strain improves estimation of filling pressures in heart failure: a simultaneous echocardiographic and invasive haemodynamic study. Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1399-8.
Kurt M, Tanboga IH, Aksakal E et al (2012) Relation of left ventricular end-diastolic pressure and N-terminal pro-brain natriuretic peptide level with left atrial deformation parameters. Eur Heart J Cardiovasc Imaging 13:524–530
Cameli M, Mandoli GE, Loiacono F et al (2016) Left atrial strain: a new parameter for assessment of left ventricular filling pressure. Heart Fail Rev 21:65–76
Kurt M, Wang J, Torre-Amione G et al (2009) Left atrial function in diastolic heart failure. Circ Cardiovasc Imaging 2:10–15
LeRoy EC, Black C, Fleischmajer R et al (1988) Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 15:202–205
van den Hoogen F, Khanna D, Fransen J et al (2013) 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 72:1747–1755
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults. Eur Heart J Cardiovasc Imaging 16:233–270
Zoghbi WA, Adams D, Bonow RO et al (2017) Recommendations for noninvasive evaluation of native valvular regurgitation. J Am Soc Echocardiogr 30:303–371
Badano LP, Kolias TJ, Muraru D et al (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography. Eur Heart J Cardiovasc Imaging 19:591–600
To AC, Flamm SD, Marwick TH, Klein AL (2011) Clinical utility of multimodality LA imaging: assessment of size, function, and structure. JACC Cardiovasc Imaging 4:788–798
Meune C, Vignaux O, Kahan A et al (2010) Heart involvement in systemic sclerosis: evolving concept and diagnostic methodologies. Arch Cardiovasc Dis 103:46–52
Ommen SR, Nishimura RA, Appleton CP et al (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Mitter SS, Shah SJ, Thomas JD (2017) A test in context: E/A and E/e′ to assess diastolic dysfunction and LV filling pressure. J Am Coll Cardiol 69:1451–1464
Tsang TSM, Abhayaratna WP, Barnes ME et al (2006) Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J Am Coll Cardiol 47:1018–1023
Lim TK, Ashrafian H, Dwivedi G et al (2006) Increased left atrial volume index is an independent predictor of raised serum natriuretic peptide in patients with suspected heart failure but normal left ventricular ejection fraction: implication for diagnosis of diastolic heart failure. Eur J Heart Fail 8:38–45
Porpáczy A, Nógrádi Á, Kehl D et al (2018) Impairment of left atrial mechanics is an early sign of myocardial involvement in systemic sclerosis. J Card Fail 24:234–242
Singh A, Addetia K, Maffessanti F et al (2017) LA strain for categorization of LV diastolic dysfunction. JACC Cardiovasc Imaging 10:735–743
Brecht A, Oertelt-Prigione S, Seeland U et al (2016) Left atrial function in preclinical diastolic dysfunction: two-dimensional speckle-tracking echocardiography-derived results from the BEFRI trial. J Am Soc Echocardiogr 29:750–758
Kuppahally SS, Akoum N, Burgon NS et al (2010) Left atrial strain and strain rate in patients with paroxysmal and persistent atrial fibrillation: relationship to left atrial structural remodeling detected by delayed-enhancement MRI. Circ Cardiovasc Imaging 3:231–239
Her A-Y, Choi E-Y, Shim CY et al (2012) Prediction of left atrial fibrosis with speckle tracking echocardiography in mitral valve disease: a comparative study with histopathology. Korean Circ J 42:311–318
Cameli M, Lisi M, Focardi M et al (2012) Left atrial deformation analysis by speckle tracking echocardiography for prediction of cardiovascular outcomes. Am J Cardiol 110:264–269
Pilichowska-Paszkiet E, Baran J, Sygitowicz G et al (2018) Noninvasive assessment of left atrial fibrosis. Correlation between echocardiography, biomarkers, and electroanatomical mapping. Echocardiography 35:1326–1334
Shuai XX, Chen YY, Lu YX et al (2011) Diagnosis of heart failure with preserved ejection fraction: which parameters and diagnostic strategies are more valuable? Eur J Heart Fail 13:737–745
Acknowledgments
Open access funding provided by University of Pécs (PTE).
Funding
No funding sources were received to support the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all patients for being included in the study.
Research involving human participants and animal rights
No animal studies were carried out by the authors for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Porpáczy, A., Nógrádi, Á., Vértes, V. et al. Left atrial stiffness is superior to volume and strain parameters in predicting elevated NT-proBNP levels in systemic sclerosis patients. Int J Cardiovasc Imaging 35, 1795–1802 (2019). https://doi.org/10.1007/s10554-019-01621-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01621-w