Abstract
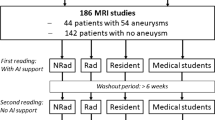
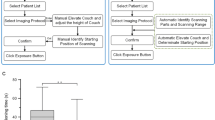
Three-dimensional printing has an increasing number of clinical applications in pediatric cardiology. Time required for dataset segmentation and conversion to stereolithography (STL) format remains a significant limitation. We investigated the impact of semi-automated cardiovascular-specific segmentation software on time and reproducibility of segmentation. Magnetic resonance angiograms (MRAs) of 19 patients undergoing intervention for right ventricular outflow lesions were segmented to demonstrate the right heart. STLs were created by two independent clinicians using semi-automated cardiovascular segmentation (SAS) and traditional manual segmentation (MS). Time was recorded and geometric STL disagreement was determined (0 % = no disagreement, 100 % = complete disagreement). MRA datasets were categorized as clean when only right heart structures were present in the MRA, or contaminated when left heart structures were also present and required removal. Eighteen (seven clean and 11 contaminated) cases were successfully segmented with both methods. Time to STL for clean datasets was faster with MS than SAS [median 209 s (IQR 192–252) vs. 296 s (272–317), p = 0.018] while contaminated datasets were faster with SAS [455 s (384–561) vs. 866 s (310–1429), p = 0.033]. Interobserver STL geometric disagreement was significantly lower using SAS than MS overall (0.70 ± 1.15 % vs. 1.31 ± 1.52 %, p = 0.030), and for the contaminated subset (0.81 ± 1.08 % vs. 1.75 ± 1.57 %, p = 0.036). Most geometric disagreement occurred at areas where left heart contamination was removed. Semi-automated segmentation was faster and more reproducible for contaminated datasets, while MS was faster but equally reproducible for clean datasets. Semi-automated segmentation methods are preferable for contaminated datasets and continued refinement of these tools should be supported.



Similar content being viewed by others
References
Dankowski R, Baszko A, Sutherland M, Firek L, Kalmucki P, Wroblewska K, Szyszka A, Groothuis A, Siminiak T (2014) 3D heart model printing for preparation of percutaneous structural interventions: description of the technology and case report. Kardiol Pol 6:546–551. doi:10.5603/KP.2014.0119
Olivieri L, Krieger A, Chen MY, Kim P, Kanter JP (2014) 3D heart model guides complex stent angioplasty of pulmonary venous baffle obstruction in a mustard repair of D-TGA. Int J Cardiol 2:e297–e298. doi:10.1016/j.ijcard.2013.12.192
O’Neill B, Wang DD, Pantelic M, Song T, Guerrero M, Greenbaum A, O’Neill WW (2015) Transcatheter caval valve implantation using multimodality imaging: roles of TEE, CT, and 3D printing. J Am Coll Cardiol Cardiovasc Imaging 2:221–225. doi:10.1016/j.jcmg.2014.12.006
Mathur M, Patil P, Bove A (2015) The role of 3D printing in structural heart disease: all that glitters is not gold. J Am Coll Cardiol Cardiovasc Imaging 8:987–988. doi:10.1016/j.jcmg.2015.03.009
Babar JL, Jones RG, Hudsmith L, Steeds R, Guest P (2010) Application of MR imaging in assessment and follow-up of congenital heart disease in adults. Radiographics 4:1145. doi:10.1148/rg.e40
Fratz S, Chung T, Greil GF, Samyn MM, Taylor AM, Valsangiacomo Buechel ER, Yoo SJ, Powell AJ (2013) Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson 15(1):51. doi:10.1186/1532-429X-15-51
Heathfield E, Hussain T, Qureshi S, Valverde I, Witter T, Douiri A, Bell A, Beerbaum P, Razavi R, Greil GF (2013) Cardiovascular magnetic resonance imaging in congenital heart disease as an alternative to diagnostic invasive cardiac catheterization: a single center experience. Congenit Heart Dis 4:322–327. doi:10.1111/chd.12032
Kilner PJ, Geva T, Kaemmerer H, Trindade PT, Schwitter J, Webb GD (2010) Recommendations for cardiovascular magnetic resonance in adults with congenital heart disease from the respective working groups of the European Society of Cardiology. Eur Heart J 7:794–805. doi:10.1093/eurheartj/ehp586
Ntsinjana HN, Hughes ML, Taylor AM (2011) The role of cardiovascular magnetic resonance in pediatric congenital heart disease. J Cardiovasc Magn Reson 13(1):51. doi:10.1186/1532-429X-13-51
Valsangiacomo Buechel ER, Grosse-Wortmann L, Fratz S, Eichhorn J, Sarikouch S, Greil GF, Beerbaum P, Bucciarelli-Ducci C, Bonello B, Sieverding L, Schwitter J, Helbing WA, Eacvi, Galderisi M, Miller O, Sicari R, Rosa J, Thaulow E, Edvardsen T, Brockmeier K, Qureshi S, Stein J (2015) Indications for cardiovascular magnetic resonance in children with congenital and acquired heart disease: an expert consensus paper of the Imaging Working Group of the AEPC and the Cardiovascular Magnetic Resonance Section of the EACVI. Eur Heart J Cardiovasc Imaging 3:281–297. doi:10.1093/ehjci/jeu129
Valverde I, Parish V, Hussain T, Rosenthal E, Beerbaum P, Krasemann T (2011) Planning of catheter interventions for pulmonary artery stenosis: improved measurement agreement with magnetic resonance angiography using identical angulations. Catheter Cardiovasc Interv 3:400–408. doi:10.1002/ccd.22695
Chung R, Taylor AM (2014) Imaging for preintervention planning: transcatheter pulmonary valve therapy. Circ Cardiovasc Imaging 1:182–189. doi:10.1161/CIRCIMAGING.113.000826
Goreczny S, Eicken A, Ewert P, Morgan GJ, Fratz S (2014) A new strategy to identify potentially dangerous coronary arterial patterns before percutaneous pulmonary valve implantation. Postep Kardiol Interwencyjnej 4:294–297. doi:10.5114/pwki.2014.46773
Khambadkone S (2012) Percutaneous pulmonary valve implantation. Ann Pediatr Cardiol 1:53–60. doi:10.4103/0974-2069.93713
Schievano S, Migliavacca F, Coats L, Khambadkone S, Carminati M, Wilson N, Deanfield JE, Bonhoeffer P, Taylor AM (2007) Percutaneous pulmonary valve implantation based on rapid prototyping of right ventricular outflow tract and pulmonary trunk from MR data. Radiology 2:490–497. doi:10.1148/radiol.2422051994
Hussain T, Greil GF, Bilska K, Miller OI (2011) Toward defining pulmonary sequestration in infancy using two-dimensional echocardiography and novel high temporal resolution "keyhole" three-dimensional magnetic resonance angiography. Congenit Heart Dis 5:488–491. doi:10.1111/j.174-0803.2011.00551.x
Zou KH, Warfield SK, Bharatha A, Tempany CM, Kaus MR, Haker SJ, Wells WM 3rd, Jolesz FA, Kikinis R (2004) Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol 2:178–189
Willinek WA, Hadizadeh DR, von Falkenhausen M, Urbach H, Hoogeveen R, Schild HH, Gieseke J (2008) 4D time-resolved MR angiography with keyhole (4D-TRAK): more than 60 times accelerated MRA using a combination of CENTRA, keyhole, and SENSE at 3.0T. J Magn Reson Imaging 6:1455–1460. doi:10.1002/jmri.21354
Prieto C, Uribe S, Razavi R, Atkinson D, Schaeffter T (2010) 3D undersampled golden-radial phase encoding for DCE-MRA using inherently regularized iterative SENSE. Magn Reson Med 2:514–526. doi:10.1002/mrm.22446
Rapacchi S, Han F, Natsuaki Y, Kroeker R, Plotnik A, Lehrman E, Sayre J, Laub G, Finn JP, Hu P (2014) High spatial and temporal resolution dynamic contrast-enhanced magnetic resonance angiography using compressed sensing with magnitude image subtraction. Magn Reson Med 5:1771–1783. doi:10.1002/mrm.24842
Acknowledgments
AT, TH, and GFG were supported by the Early Career Research Award, Children’s Clinical Research Advisory Committee, Children’s Medical Center, Dallas.
Author contribution
AT and TH performed the segmentation. SZ, TH, and AT performed data analysis. All authors contributed to project design, drafting the article, and critical revision of the article. All authors approve of the content of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors report no conflict of interest. AT, AKD, JMD, GFG, and TH all work at Children’s Medical Center, Dallas. We have full control of the primary data and agree to allow review of the data if requested.
Rights and permissions
About this article
Cite this article
Tandon, A., Byrne, N., Nieves Velasco Forte, M. et al. Use of a semi-automated cardiac segmentation tool improves reproducibility and speed of segmentation of contaminated right heart magnetic resonance angiography. Int J Cardiovasc Imaging 32, 1273–1279 (2016). https://doi.org/10.1007/s10554-016-0906-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0906-0