Abstract
Purpose
The incidence of cutaneous melanoma is rising, and Melanoma related deaths are highest among people aged 65–74. Herein, we aim to understand the impact of novel and established melanoma treatment methods on CM related mortality and all-cause mortality. We further compared these effects among Hispanic and non-Hispanic Whites (NHW).
Methods
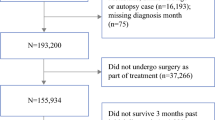
The data was extracted from the Texas Cancer Registry from 2007 to 2017. A Cox Proportional Hazard regression analysis was performed to assess treatment effect on melanoma mortality and all-cause mortality, with race-ethnicity as an effect modifier.
Results
A higher percentage of Hispanic patients presented with CM-related mortality (22.11%) compared to NHW patients (14.39%). In both the Hispanic and NHW, post-diagnosis radiation (HR = 1.610, 95% CI 0.984–2.634, HR = 2.348, 95% CI 2.082–2.648, respectively), post-diagnosis chemotherapy (HR = 1.899, 95% CI 1.085–3.322, HR = 2.035, 95% CI 1.664–2.489, respectively), and post-diagnosis immunotherapy (HR = 2.100, 95% CI 1.338–3.296, HR = 2.402, 95% CI 2.100–2.748) are each associated with an increased risk in CM-related mortality. Similar results were seen with post-diagnosis radiation (Hispanic HR = 1.640, 95% CI 1.121–2.400, NHW HR = 1.800, 95% CI 1.644–1.971), post-diagnostic chemotherapy (Hispanic HR = 1.457, 95% CI 0.898–2.364, NHW HR = 1.592, 95% CI 1.356–1.869), and post-diagnosis immunotherapy (Hispanic HR = 2.140, 95% CI 1.494–3.065, NHW HR = 2.190, 95% CI 1.969–2.435) with respect to all-cause mortality. Post-diagnosis surgery (HR = 0.581, 95% CI 0.395–0.856, HR = 0.622, 95% CI 0.571–0.678) had the opposite effect in CM-related mortality for Hispanics and NHWs respectively.
Conclusion
Our results propose differences in all-cause and CM-only related mortality with separate treatment modalities, particularly with chemotherapy, radiation therapy and immunotherapy. In addition, this retrospective cohort study showed that health disparities exist in the Hispanic Medicare population of Texas with CM.

Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- (US):
-
United States
- (FDA):
-
US Food and drug administration
- (PCP):
-
Primary care physician
- (SEER):
-
Surveillance, epidemiology, and end results
- (ALS):
-
Amyotrophic lateral sclerosis
- (TCR):
-
Texas cancer registry
- (CI):
-
Confidence interval
- (MEK):
-
Mitogen-activated protein kinase
- (TLR7/8):
-
Toll-like receptor 7 and 8
- (TNF):
-
Tumor necrosis factor
- (DMAC):
-
Data management and analysis core
- (CM):
-
Cutaneous melanoma
- (NHW):
-
Non-Hispanic White
- (HMO):
-
Health maintenance organization
- (cci):
-
Charlson’s comorbidity index
- (PH):
-
Cox proportional hazard
- (E&M):
-
Evaluation and management
- (HR):
-
Hazard ratio
References
Guy GP Jr, Thomas CC, Thompson T, Watson M, Massetti GM, Richardson LC (2015) Vital signs: melanoma incidence and mortality trends and projections - United States, 1982–2030, (in eng). MMWR Morb Mortal Wkly Rep 64(21):591–596
Leiter U, Keim U, Garbe C (2020) Epidemiology of skin cancer: update 2019, (in eng). Adv Exp Med Biol 1268:123–139. https://doi.org/10.1007/978-3-030-46227-7_6
Cormier JN et al (2006) Ethnic differences among patients with cutaneous melanoma, (in eng). Arch Intern Med 166(17):1907–1914. https://doi.org/10.1001/archinte.166.17.1907
Ward-Peterson M et al (2016) Association between race/ethnicity and survival of melanoma patients in the United States over 3 decades a secondary analysis of SEER Data. Medicine 95(17):e3315. https://doi.org/10.1097/md.0000000000003315
Garnett E, Townsend J, Steele B, Watson M (2016) Characteristics, rates, and trends of melanoma incidence among Hispanics in the USA, (in eng). Cancer Causes Control 27(5):647–659. https://doi.org/10.1007/s10552-016-0738-1
Qian Y, Johannet P, Sawyers A, Yu J, Osman I, Zhong J (2021) The ongoing racial disparities in melanoma: An analysis of the Surveillance, Epidemiology, and End Results database (1975–2016), (in eng). J Am Acad Dermatol 84(6):1585–1593. https://doi.org/10.1016/j.jaad.2020.08.097
Sanchez DP et al (2020) Racial and ethnic disparities in melanoma awareness: A cross-sectional survey, (in eng). J Am Acad Dermatol 83(4):1098–1103. https://doi.org/10.1016/j.jaad.2020.04.137
healthinsurance.org. "Health insurance coverage options in Texas | healthinsurance.org." https://www.healthinsurance.org/states/texas/ (accessed 2022).
Xie L, Kariburyo MF, Du J, Baser O (2014) Assessing the economic burden and health care utilization of U. S. medicare patients diagnosed with melanoma (in eng). Value Health 17(7):A625. https://doi.org/10.1016/j.jval.2014.08.2225
"Melanoma skin cancer statistics." https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html#:~:text=The%20average%20age%20of%20people,adults%20(especially%20young%20women). (accessed 9 Sep, 2023).
Gogebakan KC, Mukherjee K, Berry EG, Sonmez K, Leachman SA, Etzioni R (2021) Impact of novel systemic therapies on the first-year costs of care for melanoma among Medicare beneficiaries, (in eng). Cancer 127(16):2926–2933. https://doi.org/10.1002/cncr.33515
Seiger K, Schmults CD, Silk AW, Ruiz ES (2020) Cost and utilization of immunotherapy and targeted therapy for melanoma: Cross-sectional analysis in the Medicare population, 2013 and 2015, (in eng). J Am Acad Dermatol 82(3):761–764. https://doi.org/10.1016/j.jaad.2019.10.023
Zell JA, Cinar P, Mobasher M, Ziogas A, Meyskens FL Jr, Anton-Culver H (2008) Survival for patients with invasive cutaneous melanoma among ethnic groups: the effects of socioeconomic status and treatment, (in eng). J Clin Oncol 26(1):66–75. https://doi.org/10.1200/jco.2007.12.3604
Merrill RM, Pace ND, Elison AN (2010) Cutaneous malignant melanoma among white Hispanics and non-Hispanics in the United States (in eng). Ethn Dis 20(4):353–8
Wang Y, Zhao Y, Ma S (2016) Racial differences in six major subtypes of melanoma: descriptive epidemiology (in eng). BMC Cancer 16(1):691. https://doi.org/10.1186/s12885-016-2747-6
Perez MI (2019) Skin Cancer in Hispanics in the United States, (in eng). J Drugs Dermatol 18(3):s117-120
Trofymenko O, Bordeaux JS, Zeitouni NC (2018) Melanoma of the Face and Mohs Micrographic Surgery: Nationwide Mortality Data Analysis, (in eng). Dermatol Surg 44(4):481–492. https://doi.org/10.1097/dss.0000000000001429
Hartman RI, Lin JY (2019) Cutaneous Melanoma-A Review in Detection, Staging, and Management, (in eng). Hematol Oncol Clin North Am 33(1):25–38. https://doi.org/10.1016/j.hoc.2018.09.005
J. A. Sosman. "Overview of the management of advanced cutaneous melanoma - UpToDate." UpToDate. https://www-uptodate-com.libraryaccess.elpaso.ttuhsc.edu/contents/overview-of-the-management-of-advanced-cutaneous-melanoma?search=melanoma&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3 (accessed June 2022, 2022).
Rozeman EA, Dekker TJA, Haanen J, Blank CU (2018) Advanced melanoma: current treatment options, biomarkers, and future perspectives, (in eng). Am J Clin Dermatol 19(3):303–317. https://doi.org/10.1007/s40257-017-0325-6
Mishra H, Mishra PK, Ekielski A, Jaggi M, Iqbal Z, Talegaonkar S (2018) Melanoma treatment: from conventional to nanotechnology, (in eng). J Cancer Res Clin Oncol 144(12):2283–2302. https://doi.org/10.1007/s00432-018-2726-1
Bhatia S, Tykodi SS, Thompson JA (2009) Treatment of metastatic melanoma: an overview, (in eng). Oncology (Williston Park) 23(6):488–496
Sankey EW et al (2019) Operative and peri-operative considerations in the management of brain metastasis, (in eng). Cancer Med 8(16):6809–6831. https://doi.org/10.1002/cam4.2577
TCR. Cancer Statistics. https://www.dshs.texas.gov/tcr/data/statistics.aspx (accessed.
Shah BR, Hux JE, Laupacis A, Zinman B, Cauch-Dudek K, Booth GL (2007) Administrative data algorithms can describe ambulatory physician utilization, (in eng). Health Serv Res 42(4):1783–1796. https://doi.org/10.1111/j.1475-6773.2006.00681.x
Quan H et al (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data, (in eng). Med Care 43(11):1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
R. S. Young JL Jr, Ries LAG, Fritz AG,Hurlbut AA, 2001 SEER Summary Staging Manual - 2000: Codes and Coding Instructions, NIH Pub. No. 01-4969
Hu S et al (2009) Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida, (in eng). Arch Dermatol 145(12):1369–1374. https://doi.org/10.1001/archdermatol.2009.302
Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY (2008) Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis, (in eng). Lancet Oncol 9(3):222–231. https://doi.org/10.1016/s1470-2045(08)70032-9
Miller DR et al (1996) Melanoma awareness and self-examination practices: results of a United States survey, (in eng). J Am Acad Dermatol 34(6):962–970. https://doi.org/10.1016/s0190-9622(96)90273-x
Chao LX, Patterson SSL, Rademaker AW, Liu D, Kundu RV (2017) Melanoma perception in people of color: a targeted educational intervention, (in eng). Am J Clin Dermatol 18(3):419–427. https://doi.org/10.1007/s40257-016-0244-y
Ortiz CA, Goodwin JS, Freeman JL (2005) The effect of socioeconomic factors on incidence, stage at diagnosis and survival of cutaneous melanoma, (in eng). Med Sci Monit 11(5):163–172
Falcon K, Fors M, Palacios Alvarez S, Veintimilla K, Lasso N, Navas C (2019) Assessment of predictors of sun sensitivity as defined by fitzpatrick skin phototype in an ecuadorian population and its correlation with skin damage, (in eng). Dermatology 235(5):400–406. https://doi.org/10.1159/000500635
Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, Davis D, Escamilla-Cejudo JA (2016) Hispanic health in the USA: a scoping review of the literature, (in eng). Public Health Rev 37:31. https://doi.org/10.1186/s40985-016-0043-2
Dominguez K et al (2015) Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among Hispanics in the United States - 2009–2013, (in eng). MMWR Morb Mortal Wkly Rep 64(17):469–478
Eriksson H et al (2013) Low level of education is associated with later stage at diagnosis and reduced survival in cutaneous malignant melanoma: a nationwide population-based study in Sweden, (in eng). Eur J Cancer 49(12):2705–2716. https://doi.org/10.1016/j.ejca.2013.03.013
Coups EJ, Geller AC, Weinstock MA, Heckman CJ, Manne SL (2010) Prevalence and correlates of skin cancer screening among middle-aged and older white adults in the United States, (in eng). Am J Med 123(5):439–445. https://doi.org/10.1016/j.amjmed.2009.10.014
Vaidya T, Zubritsky L, Alikhan A, Housholder A (2018) Socioeconomic and geographic barriers to dermatology care in urban and rural US populations, (in eng). J Am Acad Dermatol 78(2):406–408. https://doi.org/10.1016/j.jaad.2017.07.050
Coups EJ, Stapleton JL, Hudson SV, Medina-Forrester A, Goydos JS, Natale-Pereira A (2012) Skin cancer screening among Hispanic adults in the United States: results from the 2010 National Health Interview Survey. In Arch Dermatol 148(7):861–3
Brown AE, Najmi M, Duke T, Grabell DA, Koshelev MV, Nelson KC (2022) Skin cancer education interventions for primary care providers: a scoping review, (in eng). J Gen Intern Med 37(9):2267–2279. https://doi.org/10.1007/s11606-022-07501-9
Haque W, Verma V, Butler EB, Teh BS (2019) Racial and socioeconomic disparities in the delivery of immunotherapy for metastatic melanoma in the United States, (in eng). J Immunother 42(6):228–235. https://doi.org/10.1097/cji.0000000000000264
Molina G, Kasumova GG, Qadan M, Boland GM (2020) Use of immunotherapy and surgery for stage IV melanoma, (in eng). Cancer 126(11):2614–2624. https://doi.org/10.1002/cncr.32817
Al-Qurayshi Z, Crowther JE, Hamner JB, Ducoin C, Killackey MT, Kandil E (2018) Disparities of immunotherapy utilization in patients with stage III cutaneous melanoma: a national perspective, (in eng). Anticancer Res 38(5):2897–2901. https://doi.org/10.21873/anticanres.12536
Moyers JT, Patel A, Shih W, Nagaraj G (2020) Association of sociodemographic factors with immunotherapy receipt for metastatic melanoma in the US, (in eng). JAMA Netw Open 3(9):e2015656. https://doi.org/10.1001/jamanetworkopen.2020.15656
Ikeguchi A, Machiorlatti M, Vesely SK (2020) Disparity in outcomes of melanoma adjuvant immunotherapy by demographic profile (in eng). Melanoma Manag 7(2):Mmt43. https://doi.org/10.2217/mmt-2020-0002
Dranitsaris G, Zhu X, Adunlin G, Vincent MD (2018) Cost effectiveness vs. affordability in the age of immuno-oncology cancer drugs (in eng). Expert Rev Pharmacoecon Outcomes Res 18(4):351–357. https://doi.org/10.1080/14737167.2018.1467270
Shaw DL, Dhruva SS, Ross JS (2018) coverage of novel therapeutic agents by medicare prescription drug plans following FDA approval, (in eng). J Manag Care Spec Pharm 24(12):1230–1238. https://doi.org/10.18553/jmcp.2018.24.12.1230
Singh SRK, Malapati SJ, Kumar R, Willner C, Wang D (2021) NCDB Analysis of melanoma 2004–2015: epidemiology and outcomes by subtype, sociodemographic factors impacting clinical presentation, and real-world survival benefit of immunotherapy approval (in eng). Cancers (Basel). https://doi.org/10.3390/cancers13061455
Mangin MA et al (2021) Decreased survival in patients treated by chemotherapy after targeted therapy compared to immunotherapy in metastatic melanoma, (in eng). Cancer Med 10(10):3155–3164. https://doi.org/10.1002/cam4.3760
Acknowledgements
Texas cancer data have been provided by the Texas Cancer Registry, Cancer Epidemiology and Surveillance Branch, Texas Department of State Health Services, 1100 West 49th Street, Austin, TX 78756 (www.dshs.texas.gov/tcr). Data from the Texas Cancer Registry is supported by the following: Cooperative Agreement #1NU58DP007140 from the Centers for Disease control and Prevention, Contract #75N91021D00011 from the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) Program, and the Cancer Prevention and Research Institute of Texas.
Funding
Jessica Chacon and David S. Lopez were supported by Cancer Prevention and Research Institute of Texas (CPRIT), Grant #: RP210130. Cancer Prevention and Research Institute of Texas, RP210130
Author information
Authors and Affiliations
Contributions
FR: Investigation, Project administration, Writing—Original draft preparation HR: Writing—Review and editing BD: Writing—Review and editing, Investigation MS: Writing – Review and editing LF: Writing—Review and editing SM: Writing—Review and editing RV: Writing—Review and editing DSL: Conceptualization, Supervision, Writing—Review and editing JC: Conceptualization, Supervision, Writing—Review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no funding, employment, financial or non-financial interests to disclose.
Ethical approval
The secondary data analysis was approved by Institutional review Board at the Texas Tech University Health Sciences Center El Paso, El Paso, TX, IRB#00009946.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramirez, F., Riva, H., Digbeu, B. et al. Effects of treatment methods on cutaneous melanoma related mortality and all-cause mortality in Texas: TCR-Medicare 2007–2017 database. Cancer Causes Control 35, 265–275 (2024). https://doi.org/10.1007/s10552-023-01780-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01780-1