Abstract
Purpose
We aimed to disclose the impact of the pandemic on breast cancer patients in a specialized breast cancer center (BCC).
Methods
A total of 501 breast cancer patients with a first appointment in the BCC from April 1st, 2019 to March 31st, 2021 were divided into four consecutive periods of 6 months. Data from the homologous semesters was compared. Patients with an appointment in the BCC during the study period were eligible for the secondary aim of our study (BCC workload).
Results
After the pandemic declaration (period 3), we found a decrease in the referral by screening programs (p = 0.002) and a reduction in the waiting time between the primary care referral and the first BCC appointment (p < 0.001). There were higher rates of palpable axillary nodes (p = 0.001), an increase in N stage 2 and 3 (p = 0.050), and a trend for primary endocrine therapy as the first treatment (p = 0.021) associated with higher rates of complete axillary node dissection (p = 0.030). In period 4, there were more outward diagnoses (p = 0.003) and a higher rate of surgery as the first treatment (p = 0.013).
Conclusion
COVID-19 pandemic implied a more advanced nodal stage, which may be related to the delay in breast cancer screening.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most common malignant tumor amongst Portuguese women; it also corresponds to the second cause of cancer-related death [1].
Over the past few years, due to screening programs and education for health, we verified a reduction in the stage of BC at diagnosis as well as an increase in the proportion of early-stage disease [2]. Biennially screening mammography is the most powerful tool available: if performed in women aged 50–69 years it reduces the mortality due to BC by 16.5% [3]. These facts substantiated an increase in overall survival [4] as well as an increase in breast-conserving surgery [5], that leads to better quality-of-life outcomes, especially in younger patients [6].
The emergence of a new disease resulting from the SARS-Cov2 infection had an undeniable impact all around the world. The World Health Organization (WHO) declared it as a pandemic on March 11, 2020. In Portugal, the first case was diagnosed on March 2, 2020 [7], and the Portuguese government decreed the first period of “state of emergency” on March 18, 2020 [8]. Portuguese Public Health Services (PPHS) adapted [9] to respond to the pandemic and to the rise in the demand for hospital care between these two dates. Hospital management boards outlined contingency plans, which included serious limitations to outpatient care, hospitalization, cancer treatments (chemotherapy and radiotherapy) and surgical treatments in the operating room [10]. Citizens were advised not to go to health institutions through the media unless it was compulsory [11].
Access to BC screening programs was interrupted and the private entities, which have contracts for providing breast imaging exams for the PPHS, also deeply reduced their operation [12].
These limitations to health care access, although alleviated, re-endured during the summer of 2020 and accentuated in autumn, with the development of the second pandemic wave, leading to the reduction of the number of breast pathology consultations [13] and mammograms [14]. Also, there is a perception among clinicians that more severe cases of breast cancer have manifested during the pandemic [15]. We postulate that these limitations to the access to health care have led to a worsening in the presentation of the breast malignant tumors.
The main aim of this study was to evaluate the impact of the COVID-19 pandemic on the new patients with breast cancer, considering the clinical presentation of the disease, the stage at diagnosis and the treatment strategy.
Secondary aim was to analyze the impact of the COVID-19 pandemic on the work volume of the breast cancer center (BCC) of the Centro Hospitalar Universitário São João (CHUSJ), particularly the numbers of out-patient consultations, patients treated, as well as breast cancer surgeries.
Methods
Type of study
This is a retrospective cohort study, comparing four consecutive sets of patients with breast cancer, treated at the BCC of CHUSJ, from April 1st, 2019 to March 31st, 2021.
The pandemic groups were compared with the homologous groups during the pre-COVID time. The distribution of the patients is displayed in Fig. 1.
Concerning our secondary aim, we compared the monthly figures in each period with the homologous period. The distribution of the data during each period is displayed in Table 3.
Admission criteria
Patients over 18 years old with primary invasive or in situ breast cancer and with a first appointment in the BCC during the study period were eligible for our study.
To study BCC workload (the secondary aim of our study), patients with an appointment in the BCC during the study period were eligible.
Exclusion criteria
Patients with secondary breast cancer and those with only one appointment in the BCC were excluded from our main objective analysis.
Data collection
Cancer type was defined according to the International Classification of Disease 10th Revision (ICD-10). The American Joint Committee on Cancer (AJCC) Cancer Manual 8th Edition was used to staging the disease.
The variables collected for our main analysis were: age at diagnosis; dimension of the main lesion [clinically, (mm)]; dimension of the main lesion [mammography, (mm)]; dimension of the main lesion [ultrasound, (mm)], date of the referral by the primary care (PC); date of the first appointment at BCC; date of the first multidisciplinary meeting (MDM) to define treatment; referral method; outward diagnosis; cN; uN; tumour grade (OMS classification; needle biopsy); clinical stage; first treatment strategy; lymph node procedure.
For our secondary aim, we analyzed the number of MDM assessments; number of BCC appointments; number of patients on surgery waiting list; number of patients that entered surgery waiting list, number of patients on appointment waiting list, number of patients that entered appointment waiting list, waiting time for surgery and waiting time for the first appointment in the BCC.
Statistics
Data management and statistical analysis were performed using IBM® SPSS® Statistics version 26.0. Categorical variables were expressed using counts and percentages, and continuous variables as means and standard deviation or as medians and range, as appropriate.
The chi-square test or Fisher’s test were used to assess the differences between groups. Continuous variables were analyzed using the median test. In all analyses, a p-value equal or below to 0.05 was considered statistically significant.
Missing data was not included in our analysis.
Ethics
The study “The impact of the COVID-19 pandemic in the clinical assistance to breast cancer patients” was approved by the Ethics Committee of the CHUSJ on December 18th, 2020—CES 485-20.
Confidentiality and data safety
Every case was designated by a serial number. Every study serial number was associated with a clinical file patient number. Only the principal investigator had access to that association database. Data was obtained retrospectively, retrieved from the patients' digital records and was further anonymized.
Results
Patients characteristics
In Period 1 we studied 149 patients, with a median age of 54 years (range: 32–93); in Period 2 there were 95 patients, with a median age of 58 years (range: 27–93 years); in Period 3 there were 131 patients with a median age of 59 years (range: 32–97 years); in Period 4 we analyzed 126 patients, with a median age of 56.5 years (range: 30–83 years) (Fig. 1). In the pre-pandemic Period we gathered 244 patients and in the pandemic period we collected 257 patients. There was no statistical difference in age between the groups.
The demographics and clinical variables are shown in Tables 1 and 2.
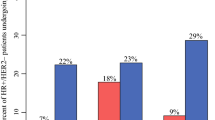
Period 3 versus period 1 (April to September of 2020 vs. April to September 2019)
There was a decrease in the referral by cancer screening programs (7.0% vs. 20.4%) (p = 0.002). There were more palpable axillary nodes in the physical exam (cN) (24.2% vs. 9.5%) (p = 0.001). Ultrasound evaluation of the lymph nodes showed an increase in the uN2 (3.8% vs. 0.0%) and uN3 (0.8% vs. 0.0%) (p = 0.050). We found an increase in the proportion of Grade 3 tumors (52.7% vs. 35.8%; p = 0.017).
Concerning the first treatment, we observed a trend to an increase in the endocrine therapy (16.0% vs. 6.0%) and a decrease in the primary surgery (56.5% vs. 67.1%) (p = 0.021).
Regarding the first lymph node approach, there was a decrease in primary sentinel node biopsies (66.4% vs. 80.4%), at the expense of an increase in primary axillary lymph node dissections (19.8% vs. 11.5%) (p = 0.030).
We verified a strong reduction in the median waiting time for the first BCC appointment after PC referral (6.0 vs. 12.0 days; p < 0.001).
There were no statistical differences between the studied periods concerning the following variables: age at diagnosis, size of main lesion (clinically, mammography and ultrasound), outward diagnosis and clinical stage. The comparison between the two time periods are shown in Tables 1 and 2.
Period 4 versus period 2 (October 2020 to March 2021 vs. October 2019 to March 2020)
There were more outward diagnoses in period 4 (19.0% vs. 5.3%; p = 0.003). There was an increase in surgery as first-line treatment (69.0% vs. 52.6%; p = 0.013). The median waiting time for the first BCC observation was reduced (6.0 vs. 11.0 days; p = 0.009). There were no statistical differences between the studied periods in the following variables: age at diagnosis, time between PC referral and first MDM discussion (days), time between first BCC appointment and first MDM discussion (days), time between first MDM assessment and first surgery, referral method, cN, uN, grade (needle biopsy) and clinical stage. The statistical results of the patients are shown in Tables 1 and 2.
BCC workload
Results on the BCC workload are displayed in the Table 3 and Figs. 2, 3. In Period 4 (vs. Period 2), the median waiting time for surgery was reduced (p = 0.002), but no meaningful differences were observed in Period 3 (vs. Period 1). There were no statistical differences between the studied periods concerning the number of MDM assessments, BCC appointments, patients on surgery waiting lists, patients that entered surgery waiting lists, patients on appointment waiting lists, patients that entered appointment waiting lists and the median of waiting time for first appointment in the BCC.
Discussion
The screening program for breast cancer consists of a biennial mammogram, in asymptomatic women between the ages of 50 and 69 years. Breast cancer screening rates for women aged 50–69 years in Portugal are over 80% [16].
Nationally, since the implementation of the screening program in 1986, more than 4.3 million screening mammograms were performed (until 2020), which resulted in the early treatment of more than 20,000 women. Therefore, treatment was less aggressive and in some cases, it led to a total cure [17].
Due to the pandemic, in many countries, including Portugal, there was an interruption of breast cancer screening programs from March 16 to June 16 of 2020, which resulted in a lower number of mammograms being performed and subsequently, a lower number of potential tumors being detected. In fact, there was a reduction of 21% in the number of mammograms performed, which corresponded to an absolute value of 169.485 fewer women with a registered mammogram than in the 2 previous years (2019 vs. 2020) [18].
Owing to the pause in the screening programs, during Period 3 (April to September of 2020), we observed that the number of patients referred to the BCC by these programs diminished, while the percentage of patients referred by other health care specialists such as their Primary Care Doctor increased. Primary Care Doctors, other health specialists and self-referral (via emergency department) played an important role in the link between the patients and hospital care during the pandemic since the interruption of the screening program.
During the second period of the pandemic, Period 4, (October 2020 to March 2021), there were more outward diagnoses. This may be explained by the higher demand for private doctors during the pandemic, thanks to the preconceived idea of limited access to family doctors and to public hospital care. This finding is consistent with a study conducted in Bangladesh, which reported that approximately 75% of the responders sought diagnosis assistance from private hospitals during the pandemic [19].
For several weeks there were no referrals from the primary care. Consequently, there were no patients accumulated waiting for consultation. Thus, when patients started to get referred again, the time for the consultation was lower. This resulted in fewer days between referral by the PC and the first BCC consultation during both pandemic periods.
During Period 3, there were also fewer days between the first BCC appointment and the first MDM discussion. Since the workload of BCC lowered, a quicker response could be given to patients.
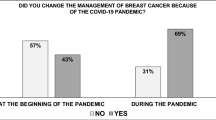
Although there was a higher percentage of patients being referred to the BCC by their Primary Care Doctor and other health specialists during the first half of the pandemic, patients were afraid of going to the hospital and leaving their homes. This fear might have contributed to some cancers not being diagnosed in time. A survey by the American College of Emergency Physicians demonstrated that nearly a third of patients (29%) had delayed or avoided seeking medical care due to the fear of contracting the coronavirus in March/April, 2020 [20]. In fact, COVID-19-related anxiety could also affect the patient’s decision-making process [21], leading to a lower number of patients seeking medical help and treatment.
The evaluation of axillary lymph nodes is an important factor in the management and staging of breast cancer as it is a predictor of survival outcome [22]. In the first pandemic period (Period 3), we found higher rates of palpable axillary nodes on physical examination and an increase in N stages 2 and 3. Ultrasound evaluation was in line with the clinical findings during the physical examination. Other recently published studies conducted in Italy demonstrated that a 2 month stop in mammographic screening produced a significant increase in node-positive breast cancer [23] and that during 2020 there was an increase in symptomatic patients being diagnosed [24] which is consistent with our results and with our hypothesis.
Since more suspected nodes were present at diagnosis, a higher number of needle biopsies were performed to characterize these nodes. If the biopsy confirmed lymph node metastasis, patients were submitted to lymph node dissection instead of a sentinel node biopsy [25]. Therefore, in juxtaposition with alternative research [26], we observed a lower number of sentinel node procedures and a higher number of lymph node axillary dissections because of the higher number of metastatic nodes at diagnosis.
To offload hospitals and better treat patients during the pandemic without compromising their health, many societies made extraordinary recommendations. One of these was to postpone surgery in favor of neoadjuvant endocrine therapy in early-stage ER-positive and HER-negative patients until regular workload could be resumed [27, 28]. This change in the treatment approach is consistent with the result that we observed with an increase in endocrine therapy, with a subsequent decrease in the primary surgery rates. A multicenter international analysis on the effect of the COVID-19 pandemic in EUSOMA-certified breast cancer centers (which includes BCC) showed that neoadjuvant treatment was used safely to delay surgery, although there was a significantly higher lymph node stage at presentation [29].
Due to the contingency plans implemented by hospital management boards, there were serious limitations on access to surgeries and oncologic treatments, which resulted in a lower rate of surgical treatments. In the USA, during the early stages of the global pandemic, breast cancer surgery declined significantly as well [30].
In the 4th period, there was a recovery in surgery as first-line treatment, and a decrease in chemotherapy and endocrine therapy, which might have resulted from the alleviation of the governmental limitations, leading to the return of normal surgical activity. Indeed, finding aligns with a recently published study that documents a complete recovery in number of breast surgeries performed since the second half of the lockdown period [31]
Patients also underwent surgery faster during this post-limitations period since there was a lowering in the absolute number of patients that were waiting for surgery, which resulted in a lower median time of waiting for surgery. It has been shown that there were statistically significant differences, favoring 2020, when analyzing time-to surgery and time-to radiotherapy [32]. While it is important to minimize unnecessary delays, the emphasis on breast cancer treatment should move away from striving to meet a specific time limit for surgery. Instead, the priority should be placed on ensuring that every aspect of patient’s care contributes effectively and optimally to their overall management [33].
One limitation of the present study is its retrospective design. In fact, multiple healthcare professionals were involved in patient care, which resulted in a less accurate and consistent database than the one that could be achieved with a prospective cohort study.
Treatment approaches were adapted rapidly due to the dedication and effort put into by the BCC team. Although at the beginning of the pandemic, most health care services stopped or slowed down their work volume, the BCC team was able to efficiently treat breast cancer patients without increasing waiting times. In fact, the effect of the COVID-19 pandemic on EUSOMA-certified breast cancer centers showed that the quality of breast cancer care was well maintained during the pandemic period [29].
Conclusion
This study showed no impact of the COVID-19 pandemic on BC T stage at diagnosis. However, the presence of lymph node metastasis at diagnosis was more frequent than before and this resulted in differences in the treatment strategy. At the same time, the referrals from the screening program diminished significantly.
Considering the BCC work volume and waiting times, COVID-19 pandemic didn’t had a significant impact.
Data availability
Due to the nature of the research, due to [ethical/legal/commercial] supporting data is not available.
References
Liga Portuguesa Contra o Cancro (2020) https://www.ligacontracancro.pt/cancro-da-mama. Accessed 23 Nov 2020
Verdial FC, Etzioni R, Duggan C, Anderson BO (2017) Demographic changes in breast cancer incidence, stage at diagnosis and age associated with population-based mammographic screening. J Surg Oncol 115(5):517–522. https://doi.org/10.1002/jso.24579
Mandelblatt JS, Cronin KA, Bailey S, Berry DA, de Koning HJ, Draisma G et al (2009) Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med 151(10):738–747. https://doi.org/10.7326/0003-4819-151-10-200911170-00010
Tabár L, Dean PB, Chen TH, Yen AM, Chen SL, Fann JC et al (2019) The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening. Cancer 125(4):515–523. https://doi.org/10.1002/cncr.31840
Zorzi M, Puliti D, Vettorazzi M, De Lisi V, Falcini F, Federico M et al (2006) Mastectomy rates are decreasing in the era of service screening: a population-based study in Italy (1997–2001). Br J Cancer 95(9):1265–1268. https://doi.org/10.1038/sj.bjc.6603405
Veiga DF, Campos FSM, Ribeiro LM, Junior Archangelo I, Filho Veiga J, Juliano Y et al (2010) Mastectomy versus conservative surgical treatment: the impact on the quality of life of women with breast cancer. Revista Brasileira de Saúde Materno Infantil 10(1):51–57. https://doi.org/10.1590/S1519-3829201000010000
SNS Serviço Nacional de Saúde (2020) Covid-19 dissemination in Portugal. https://www.sns.gov.pt/noticias/2020/09/28/covid-19-disseminacao-em-portugal/. Accessed 20 Nov 2020
Portugal.gov.pt (2020) Decreto do Governo que regulamenta o estado de emergência. https://www.portugal.gov.pt/pt/gc22/comunicacao/documento?i=decreto-do-governo-que-regulamenta-o-estado-de-emergencia. Accessed 20 Nov 2020
Governo de Portugal (2020) Comunicado do Conselho de Ministros de 12 de março de 2020—Medidas extraordinárias de resposta à epidemia do novo coronavírus. https://www.portugal.gov.pt/pt/gc22/governo/comunicado-de-conselho-de-ministros?i=330. Accessed 20 Nov 2020
Portal-chsj.min-saude.pt (2020) Plano de Contingência Covid-19. https://portal-chsj.min-saude.pt/pages/1034. Accessed 26 Nov 2020
Koca B, Yildirim M (2021) Delay in breast cancer diagnosis and its clinical consequences during the coronavirus disease pandemic. J Surg Oncol 124(3):261–267
Liga Portuguesa Contra o Cancro (2020) Plano de Contingência COVID-19 no Núcleo Regional do Norte—Notícias. https://www.ligacontracancro.pt/noticias/detalhe/url/plano-de-contingencia-covid-19-no-nucleo-regional-do-norte/. Accessed 20 Nov 2020
Saudemais.tv (2020) Covid-19: Quase mil cancros da mama, colo do útero e colorretal ficaram por diagnosticar—Liga, (2020). https://www.saudemais.tv/noticia/24180-covid-19-quase-%20mil-cancros-da-mama-colo-do-utero-e-colorretal-ficaram-por-diagnosticar. Accessed 22 Nov 2020
Sinalaberto.pt (2020) Efeitos colaterais da covid-19. https://sinalaberto.pt/efeitos-colaterais-da-covid-19-2/. Accessed 22 Nov 2020
Saudemais.tv (2022) Impacto da pandemia no cancro ainda por apurar mas há mais casos graves (2022). https://saudemais.tv/noticia/37595-impacto-da-pandemia-no-cancro-ainda-por-apurar-mas-ha-mais-casos. Accessed 6 Feb 2022
OECD (2016) Health status (Edition 2016). OECD Health Statistics (database). https://doi.org/10.1787/a70ec4d5-en
Liga Portuguesa Contra o Cancro (2022) Rastreio e diagnóstico precoce. https://www.ligacontracancro.pt/servicos/detalhe/url/programa-de-rastreio-de-cancro-da-mama/. Accessed 11 Aug 2022
Transparencia.sns.gov.pt (2022) Rastreios oncológicos 2022. https://transparencia.sns.gov.pt/explore/dataset/rastreios-oncologicos/table/?disjunctive.regiao&disjunctive.aces&sort=tempo. Accessed 15 Aug 2022
Akhtar K, Akhtar K, Nahar S, Hossain S, Rahman MM (2023) Current treatment status and treatment seeking time of breast cancer patients during COVID-19 pandemic in Bangladesh. Asian Pac J Cancer Prev 24(6):1835–1840. https://doi.org/10.31557/APJCP.2023.24.6.1835
American College of Emergency Physicians (2020). American college of emergency physicians Covid-19. https://www.emergencyphysicians.org/globalassets/emphysicians/all-pdfs/acep-mc-covid19-april-poll-analysis.pdf. Accessed 11 July 2022
Vanni G, Materazzo M, Pellicciaro M, Ingallinella S, Rho M, Santori F et al (2020) Breast cancer and COVID-19: the effect of fear on patients’ decision-making process. Vivo 34(3):1651–1659. https://doi.org/10.21873/invivo.11957
Park KU, Caudle A (2018) Management of the axilla in the patient with breast cancer. Surg Clin North Am 98(4):747–760. https://doi.org/10.1016/j.suc.2018.04.001
Toss A, Isca C, Venturelli M, Nasso C, Ficarra G, Bellelli V et al (2021) Two-month stop in mammographic screening significantly impacts on breast cancer stage at diagnosis and upfront treatment in the COVID era. ESMO open 6(2):100055. https://doi.org/10.1016/j.esmoop.2021.100055
Mentrasti G, Cantini L, Vici P, D’Ostilio N, La Verde N, Chiari R et al (2022) Rising incidence of late stage breast cancer after COVID-19 outbreak. Real-world data from the Italian COVID-DELAY study. Breast 65:164–171. https://doi.org/10.1016/j.breast.2022.08.007
Abe H, Schmidt RA, Sennett CA, Shimauchi A, Newstead GM (2007) US-guided core needle biopsy of axillary lymph nodes in patients with breast cancer: why and how to do it. Radiographics 27(Suppl 1):S91–S99. https://doi.org/10.1148/rg.27si075502
Borella F, Bertero L, Di Giovanni F, Witel G, Orlando G, Ricci AA, Pittaro A, Castellano I, Cassoni P (2023) COVID-19 and breast cancer: analysis of surgical management of a large referral center during the 2020–2021 pandemic period. Curr Oncol 30(5):4767–4778. https://doi.org/10.3390/curroncol30050359
ESMO (2020) ESMO management and treatment adapted recommendations in the COVID-19 era: breast cancer. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic/breast-cancer-in-the-covid-19-era. Accessed 19 Nov 2020
Di Lena É, Hopkins B, Wong SM, Meterissian S (2022) Delays in operative management of early-stage, estrogen receptor-positive breast cancer during the COVID-19 pandemic: a multi-institutional matched historical cohort study. Surgery 171(3):666–672. https://doi.org/10.1016/j.surg.2021.10.033
van Dam P, Tomatis M, Ponti A, Marotti L, Aristei C, Biganzoli L et al (2022) The impact of the SARS-COV-2 pandemic on the quality of breast cancer care in EUSOMA-certified breast centres. Eur J Cancer 177:72–79. https://doi.org/10.1016/j.ejca.2022.09.027
Yin K, Singh P, Drohan B, Hughes KS (2020) Breast imaging, breast surgery and cancer genetics in the age of COVID-19. Cancer 126(20):4466–4472. https://doi.org/10.1002/cncr.33113
Vissio E, Falco EC, Collemi G et al (2021) Impact of COVID-19 lockdown measures on oncological surgical activity: analysis of the surgical pathology caseload of a tertiary referral hospital in Northwestern Italy. J Surg Oncol 123(24):24–31. https://doi.org/10.1002/jso.26256
Losurdo A, Lisa AVE, Tomatis M, Ponti A, Montemezzi S, Bonzano E et al (2022) Highly specialized breast centers did not experience delay of care during COVID-19 pandemic in Italy: the senonetwork experience. Breast Cancer Res Treat 196(1):87–95. https://doi.org/10.1007/s10549-022-06694-1
Xu J, Bromley L, Chew G, Yeo B (2020) “First do no harm”: significance of delays from diagnosis to surgery in patients with non-metastatic breast cancer. World J Surg 44(11):3812–3820. https://doi.org/10.1007/s00268-020-05725-6
Funding
Open access funding provided by FCT|FCCN (b-on). The authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Data collection was performed by IR and JLF. Formal analysis and interpretation were performed by IR and BP. The first draft of the manuscript was written by IR and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. The study design, surgical procedures, supervision and conceptualization were performed by JLF.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The study “The impact of the COVID-19 pandemic in the clinical assistance to breast cancer patients” was approved by the Ethics Committee of the CHUSJ on December 18th, 2020—CES 485-20.
Informed consent
The retrospective nature of the analysis supported the informed consent waiver, for the sake of feasibility.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ribeiro, I., Peleteiro, B. & Fougo, J.L. The impact of the COVID-19 pandemic in the clinical assistance to breast cancer patients. Cancer Causes Control 35, 63–72 (2024). https://doi.org/10.1007/s10552-023-01762-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01762-3