Abstract
Purpose
Women with diabetes have lower survival rates after a cervical cancer diagnosis compared to women without diabetes. Pap smears and human papilloma virus (HPV) testing are highly effective screening tests for cervical cancer, therefore, it is important to know the prevalence of guideline-concordant screening among women with diabetes and understand if their predictors of screening differ. The purpose of this analysis was to assess guideline-concordant cervical cancer screening and predictors by diabetes status.
Methods
We used the 2019 National Health Interview Survey data, limited to women aged 21–65 years without a previous diagnosis of cancer, a hysterectomy, or diagnosed with diabetes in the year prior to the survey. We considered the Pap and HPV tests together and concordance as being tested within the past 3 years as part of a routine exam. We calculated weighted, adjusted prevalence, and prevalence ratios (PRs) of screening concordance comparing women with diabetes to those without.
Results
The unadjusted prevalence of concordant screening was 66.5% for women with diabetes compared to 73.3% for women without diabetes (PR = 0.91 95% CI 0.84–0.98). In the fully adjusted model adjusting for factors known to be associated with diabetes and access to healthcare, the association was attenuated and no longer statistically significant (PR = 0.96 95% CI 0.89–1.04).
Conclusion
Cervical cancer screening concordance was lower in women with diabetes compared to those without overall but the deficit appears to be due primarily to underlying differences in sociodemographic characteristics and access to healthcare and not diabetes independently.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
While there is limited evidence that women with diabetes are at higher risk of cervical cancer, there is evidence of worse prognostic indicators and lower survival rates after a cervical cancer diagnosis compared to women without diabetes [1,2,3,4]. For example, in one study with approximately 5-year median follow-up, women with diabetes were approximately 1.5 times more likely to die from early-stage (I–IIA) cervical cancer than women without diabetes [3].
Pap smears and human papilloma virus (HPV) tests are highly effective screening tests in the prevention and early detection of cervical cancer [5]. Because of the increased mortality risk, it is imperative that women with diabetes are up to date with cervical cancer screening guidelines. However, a number of studies have found that cervical cancer screening is lower among women with diabetes [6,7,8]. Many of these studies have been conducted outside the USA, with different population demographics and health insurance systems. In addition, most studies conducted in the USA occurred before HPV testing was recommended as a screening test and before passage of the Affordable Care Act in 2010, which mandated the coverage of preventive services, such as cancer screening [9]. While a recent study using state-level estimates in the USA also found lower levels of cervical cancer screening among women with diabetes compared to those without, unfortunately, the data used were only able to assess if women were “ever screened” for cervical cancer with HPV testing and not if they were guideline concordant [8].
The prevalence of diabetes continues to increase [10], therefore, it is important to compare guideline-concordant screening by diabetes status in the USA and understand if the predictors of screening differ among women with diabetes. Using a population-based national survey, the objectives of this analysis were to assess guideline-concordant cervical cancer screening by diabetes status, compare characteristics of the women who were concordant by diabetes status, and determine predictors. Secondarily, we compared reasons for not being screened by diabetes status.
Methods
Study population
The study population for this analysis was the 2019 National Health Interview Survey (NHIS) data, limited to women aged 21–65 years. We excluded women with a previous diagnosis of cancer, a hysterectomy, or diagnosed with diabetes in the year prior to the survey. Previous cancers were excluded to help limit the study population to women under normal cancer surveillance. The diabetes exclusion was because of a noted detection bias of cancer within a year of a diabetes diagnosis [11].
Cervical cancer screening
Currently, the US Preventive Services Task Force (USPSTF) recommends either a Pap smear (every 3 years) or HPV test alone (every 5 years) or a combination of the tests (every 5 years) [5]. The NHIS asks women if they have ever had a test for cervical cancer and when their most recent test was. Although the NHIS asks about Pap smears and HPV testing separately, we considered the tests together because a previous study found that women may not know which test they received or if they received both [12]. For the purpose of this analysis, guideline-concordant screening was defined as having either test within the past 3 years to be consistent with a previous analysis of cervical cancer screening with the NHIS [12]. Because we were interested in asymptomatic cancer screening, we excluded women who reported having a cervical test because of a problem or as a follow-up of an earlier screening test. For women who had never had a cervical cancer screening test or had not had one in the last 5 years, they were asked the reason why they have not been tested.
Statistical analysis
We calculated prevalence estimates of guideline-concordant cervical cancer screening by diabetes status, which were weighted to account for non-response and selection probabilities. We used chi-squared tests to assess differences in characteristics and reasons for not getting screened by diabetes status. We calculated weighted, adjusted prevalence, and prevalence ratios (PRs) of screening concordance comparing women with diabetes to those without. This method was chosen over logistic regression to provide adjusted prevalence estimates and reduce a perceived overestimation of an association with an odds ratio [13, 14]. The variables assessed as potential predictors of screening included age group (21–39 years, 40–49, 50–59, 60–65), race/ethnicity (Hispanic, White non-Hispanic, Black non-Hispanic, Asian non-Hispanic, Other), education level [< high school (HS), HS graduate, > HS degree], household income (< $35 K, 35–49, 50–74, ≥ 75), birthplace (USA, outside USA), health insurance coverage (covered, not covered), usual place for healthcare (yes, no), saw a doctor or healthcare provider in the past year (yes, no), delayed medical care due to cost in past 12 months (yes, no), region (Northwest, Midwest, South, West), urban/rural residence (central metro, fringe metro, medium/small metro, non-metro), marital status (married/partnered, not married/partnered), current employment status (employed, not employed), self-rated health (excellent/very good/good, fair/poor), and the number of non-diabetes chronic conditions (0, 1, ≥ 2). Non-diabetes chronic conditions included hypertension, coronary heart disease, angina, myocardial infarction, stroke, COPD, and asthma. We compared PRs for concordant screening by diabetes status between three models: an unadjusted model, an age-adjusted model, and a full model adjusting for all variables potentially predictive of concordant screening. To assess whether the predictors of screening concordance differed by diabetes status, we ran separate models for diabetes and screening concordance with an interaction term for each potential predictor variable and diabetes in the fully adjusted model. Analyses were conducted in SAS 9.4 using survey procedures and SUDAAN 11.0.1 to calculate adjusted PRs.
Results
There were 11,763 women aged 21–65 years in 2019 NHIS population. After excluding women with a hysterectomy (n = 1754), previous diagnosis of cancer (n = 612), diabetes diagnosis in the past year (n = 16) or non-type I/type II diabetes (n = 20), or had a cervical test because of a problem or follow-up (n = 472), there were 8,889 women available for analysis [436 with diabetes (4.9%), 8,453 (95.1%) without].
Table 1 presents the unweighted number of participants and weighted distribution of all examined characteristics. The distribution of all characteristics was significantly different by diabetes status except for USA region and birthplace. Women with diabetes were more likely to be older, Black non-Hispanic or Hispanic, live in more rural locations, have lower education and income levels, have a usual source of healthcare and have seen a doctor in the past year, rate their health as fair or poor, and have higher numbers of non-diabetes comorbid conditions.
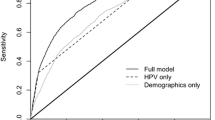
The unadjusted prevalence of concordant screening was 66.5% for women with diabetes compared to 73.3% for women without diabetes (PR = 0.91 95% CI 0.84 – 0.98) (Table 2). There was little change in the adjusted PR (aPR) in the age-adjusted only model, which was borderline statistically significant (aPR = 0.92 95% CI 0.84 – 1.00). In the fully adjusted model, the PR was attenuated toward the null and was no longer statistically significant (aPR = 0.96 95% CI 0.89 – 1.04). Not seeing a doctor in the past year was the strongest predictor of concordant screening (aPR = 0.65 95% CI 0.61 – 0.71). No health insurance and no usual source of healthcare had equivalent associations with screening but were not as strong as seeing a doctor in the past year (aPR = 0.89 for both).
When comparing all potential predictors by diabetes status (Table 3), urbanicity (p-value for interaction term = 0.02), household income (p = 0.04), and delaying care because of medical costs (p = 0.03) were the only predictors that were significantly different by diabetes status. There were too few observations for seeing a doctor in the past year and usual source of healthcare to examine stratified by diabetes status so they were not included. For urbanicity, women with diabetes in a non-metro area were significantly more likely to be concordant with screening compared to women living in a central metro area (aPR = 1.19 95% CI 1.03 – 1.38), while there was no association among women without diabetes (aPR = 0.97 95% CI 0.92 – 1.02). For delayed care, women without diabetes were slightly less likely to be concordant if they had delayed care (aPR = 0.94 95% CI 0.89 – 0.99) but among women with diabetes, the association was borderline non-significantly elevated (aPR = 1.14 95% CI 0.99 – 1.31). We also found a statistically significant interaction with income but women in all levels of income were less likely to be screened than the highest income regardless of diabetes status.
When we compared reasons for not getting screened for cervical cancer (ever or in past 5 years), there was very little difference in the distribution of reasons (Table 4; p = 0.94). For both groups, the major reason was “No reason/Never thought about it.”
Discussion
In this analysis of a nationally representative sample of women in the USA, we found that overall, women with diabetes were less likely to be concordant with cervical cancer screening; however, once controlling for other predictors of concordant screening, the association with diabetes was attenuated toward the null and no longer statistically significant. Most predictors of concordant screening were similar for women with or without diabetes but we did see evidence of heterogeneity for urbanicity, income, and delayed medical care. We also found little evidence that reasons for not being screened differed by diabetes status.
Most studies examining cervical cancer screening by diabetes status have been conducted outside of the USA. Within the USA, two studies were conducted in specific states (KY, OR) [15, 16] and all but one were conducted prior to HPV being recommended as screening test and passage of the Affordable Care Act [6, 8]. Therefore, more recent national data are needed. A recent analysis using the Behavioral Risk Factor Surveillance System (BRFSS) found a lower prevalence of cervical cancer screening among women with diabetes compared to those without even after adjustment for other factors, but that study was limited to just HPV testing and if women had ever been tested [8]. We reported on Pap smears and HPV testing combined but unlike the BRFSS analysis, once we controlled for other participant characteristics, there was no association between diabetes status and concordant screening. In the BRFSS, there was also indication of lower rates of screening in southern states, while there was no evidence of regional differences in the NHIS.
Another recent retrospective cohort study conducted in Canada with administrative data found lower cervical cancer screening rates among women with prevalent (but not incident) diabetes [7]. They found women with diabetes had a 15% lower rate of concordant cervical cancer screening compared to women without diabetes. There are a number of factors that make these analyses difficult to compare. Most notably, the population demographics differ, as well as each country’s healthcare system. Since the strongest associations we found for predictors in this analysis were healthcare related (i.e., having health insurance, a usual place for healthcare, and visiting a doctor in the past year), it is important to have data available for diabetes and cervical cancer screening in the USA where healthcare coverage is not universal. However, the results from Canada with universal healthcare coverage would indicate that having health insurance in the USA is not sufficient for equal screening concordance. Our results are consistent with previous literature in the USA demonstrating the importance of a usual source of care in addition to health insurance for receipt of preventive care [17, 18].
We did not find evidence that screening concordance by race/ethnicity differed by diabetes status. This is important because the risk of being diagnosed with and dying from diabetes and cervical cancer are both higher in Hispanic and Black non-Hispanic women [10, 19, 20]. Based on this analysis, interventions targeted to increase screening in these groups would not need to consider diabetes as a modifying factor. Access to care still appears to be the biggest obstacle regardless of diabetes. This analysis may also indicate that other chronic conditions are not specifically barriers to screening and are secondary to other patient characteristics since the number of chronic conditions was not predictive of concordant screening after adjusting for other factors.
The differences we found by diabetes status for urbanicity are interesting in that women with diabetes in rural areas were more likely to be screened for cervical cancer than women in metro areas, while women without diabetes in rural areas were less likely to be screened than women in metro areas. Breast and cervical cancer screening have been shown to be persistently lower in rural communities and these women face additional barriers to healthcare [21]. Perhaps having a chronic condition, such as diabetes, helps overcome some of these barriers in rural communities but acts more of a burden in metro areas. While studies have compared barriers to cervical cancer screening in urban and rural women [22, 23], we are unaware of any that have examined the barriers by diabetes or other chronic disease status.
A major limitation of this analysis is relying on self-reported screening, which makes it less reliable to compare Pap smears and HPV tests to each other. However, for the purposes of this analysis, the focus was on any concordant screening. Because the NHIS includes such a broad questionnaire, we were able to control for and examine many potential predictors of concordant screening. However, it should be noted that we calculated a substantial number of statistical tests and did not adjust for multiple testing. It is also important to note that these data were collected prior to the Covid-19 pandemic, which has provided substantial disruption to cancer screening schedules and routines [24]. It is unclear how these results might differ as screenings begin to recover and it is unlikely that the recovery will be equal across groups, which could exacerbate existing disparities.
Cervical cancer screening rates have been declining since 2000 [12]. Because of lower survival from cervical cancer among women with diabetes and increasing prevalence of diabetes, it is important to increase cervical cancer screening in these women. Based on the results of this study, it appears that while cervical cancer screening concordance may be lower in women with diabetes compared to those without overall, the deficit appears to be due primarily to underlying differences in sociodemographic characteristics and access to healthcare and not diabetes independently.
Data availability
Data available by download from https://www.cdc.gov/nchs/nhis/2019nhis.htm
Code availability
Relevant code is available by request.
References
Chen S, Tao M, Zhao L, Zhang X (2017) The association between diabetes/hyperglycemia and the prognosis of cervical cancer patients: a systematic review and meta-analysis. Medicine (Baltimore) 96(40):e7981
Gillani SW, Zaghloul HA, Ansari IA et al (2019) Multivariate analysis on the effects of diabetes and related clinical parameters on cervical cancer survival probability. Sci Rep 9(1):1084
Kuo HY, Lin ZZ, Kuo R et al (2015) The prognostic impact of type 2 diabetes mellitus on early cervical cancer in Asia. Oncologist 20(9):1051–1057
Anastasi E, Filardi T, Tartaglione S et al (2018) Linking type 2 diabetes and gynecological cancer: an introductory overview. Clin Chem Lab Med 56(9):1413–1425
Force USPST, Curry SJ, Krist AH et al (2018) Screening for cervical cancer: US preventive services task force recommendation statement. JAMA 320(7):674–686
Bhatia D (2020) IC Lega, W Wu, and LL Lipscombe, Breast, cervical and colorectal cancer screening in adults with diabetes: a systematic review and meta-analysis. Diabetologia 63(1):34–48
Bhatia D, Sutradhar R, Austin PC et al (2022) Periodic screening for breast and cervical cancer in women with diabetes: a population-based cohort study. Cancer Causes Control 33(2):249–259
McDaniel CC, Hallam HH, Cadwallader T, Lee HY, Chou C (2021) Disparities in cervical cancer screening with HPV test among females with diabetes in the deep south. Cancers (Basel). 13(24):6319
Moyer VA, Force USPST (2012) Screening for cervical cancer: US preventive services task force recommendation statement. Ann Intern Med 156(12):880–891
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services.
Dankner R, Boffetta P, Balicer RD et al (2016) Time-dependent risk of cancer after a diabetes diagnosis in a cohort of 2.3 million adults. Am J Epidemiol 183(12):1098–1106
Watson M, Benard V, King J, Crawford A, Saraiya M (2017) National assessment of HPV and Pap tests: changes in cervical cancer screening. National Health Interview Survey Prev Med 100:243–247
Bieler GS, Brown GG, Williams RL, Brogan DJ (2010) Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol 171(5):618–623
Tamhane AR, Westfall AO, Burkholder GA, Cutter GR (2017) Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Stat Med 36(23):3760
Fleming ST, Love MM, Bennett K (2011) Diabetes and cancer screening rates among Appalachian and non-Appalachian residents of Kentucky. J Am Board Fam Med 24(6):682–692
Liu BY, O’Malley J, Mori M et al (2014) The association of type and number of chronic diseases with breast, cervical, and colorectal cancer screening. J Am Board Fam Med 27(5):669–681
Blewett LA, Johnson PJ, Lee B, Scal PB (2008) When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med 23(9):1354–1360
DeVoe JE, Fryer GE, Phillips R, Green L (2003) Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health 93(5):786–791
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics. CA Cancer J Clin 70(1):7–30
Murphy SL, Xu J, Kochanek KD, Arias E, Tejada-Vera B (2021) Deaths: final data for 2018. Natl Vital Stat Rep 69(13):1–83
Doescher MP, Jackson JE (2009) Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract 15(3):200–209
Bazargan M, Bazargan SH, Farooq M, Baker RS (2004) Correlates of cervical cancer screening among underserved Hispanic and African-American women. Prev Med 39(3):465–473
Coughlin SS, King J, Richards TB, Ekwueme DU (2006) Cervical cancer screening among women in metropolitan areas of the United States by individual-level and area-based measures of socioeconomic status, 2000–2002. Cancer Epidemiol Biomarkers Prev 15(11):2154–2159
Miller MJ, Xu L, Qin J et al (2021) Impact of COVID-19 on Cervical Cancer Screening Rates Among Women Aged 21–65 Years in a Large Integrated Health Care System - Southern California, January 1-September 30, 2019, and January 1-September 30, 2020. MMWR Morb Mortal Wkly Rep 70(4):109–113
Acknowledgments
Disclaimer: Opinions expressed by the authors are their own and this material should not be interpreted as representing the official viewpoint of the US Department of Health and Human Services, the National Institutes of Health, or the National Cancer Institute.
Funding
None. Work carried out as regular duties as US Government employees.
Author information
Authors and Affiliations
Contributions
EAM: contributed to conceptualization, methodology, formal analysis, and writing, reviewing, and editing of the manuscript. PP: contributed to methodology and writing, reviewing, and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
Not applicable. Secondary data analysis.
Consent to participate
None.
Consent for publication
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miller, E.A., Pinsky, P.F. Cervical cancer screening and predictors of screening by diabetes status. Cancer Causes Control 33, 1305–1312 (2022). https://doi.org/10.1007/s10552-022-01615-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-022-01615-5