Abstract
Purpose
Despite widespread promotion of breast and cervical cancer (BCC) screening, uptake remains low in rural communities. Barriers to healthcare, which often result in poorer health outcomes, differentially impact residents of rural communities. Effective interventions addressing the unique needs of rural women may target these barriers and increase BCC screening participation. Our objective is to review and assess the published literature on interventions to increase BCC screening in rural communities.
Methods
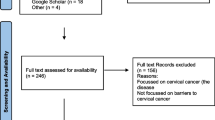
A systematic scoping review of PubMed/Medline was performed to identify BCC screening interventions conducted in rural settings. English language articles from peer-reviewed journals published from January 2006 to October 2019 were included if they reported results for BCC screening interventions in rural communities in the United States.
Results
We reviewed 228 articles and identified eight articles consistent with our inclusion criteria. Studies varied in sample population characteristics, geographic location, design, and mode of intervention delivery. Interventions included patient navigation strategies, educational outreach programs, peer counseling, and small media initiatives. Interventions focused on promoting uptake of initial or one-time screening rather than targeted repeat screening, and few studies detailed the cost-effectiveness of the interventions.
Conclusion
This review may inform efforts to develop strategies to increase BCC screening among rural women. Additional cancer prevention and control research gaps in rural communities include the examination of the theoretical foundations, design, delivery, and cost-effectiveness of BCC screening interventions for rural communities. Future research might focus on methods to promote repeat BCC screening and effective translation of these interventions for other rural populations.

Similar content being viewed by others
References
Doescher MP, Jackson JE (2009) Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract 15(3):200–209. https://doi.org/10.1097/PHH.0b013e3181a117da
Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker B, Richardson LC (2017) Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties—United States. MMWR Surveill Summ 66(14):1–13. https://doi.org/10.15585/mmwr.ss6614a1
Mille JW, Royalty J, Henley J, White A, Richardson LC (2015) Breast and cervical cancers diagnosed and stage at diagnosis among women served through the National Breast and Cervical Cancer Early Detection Program. Cancer Causes Control CCC 26(5):741–747. https://doi.org/10.1007/s10552-015-0543-2
Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T (2005) Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health 21(3):206–213. https://doi.org/10.1111/j.1748-0361.2005.tb00084.x
Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P (2015) Challenges of rural cancer care in the United States. Oncology 29(9):633–640
Chan L, Hart LG, Goodman DC (2006) Geographic access to health care for rural Medicare beneficiaries. J Rural Health 22(2):140–146. https://doi.org/10.1111/j.1748-0361.2006.00022.x
Schoenberg NE, Studts CR, Hatcher-Keller J, Buelt E, Adams E (2013) Patterns and determinants of breast and cervical cancer non-screening among Appalachian women. Women Health 53(6):552–571. https://doi.org/10.1080/03630242.2013.809400
Yu L, Sabatino S, White M (2019) Rural-urban and racial disparities in invasive cervical cancer incidence in the United States, 2010–2014. Prev Chron Dis. https://doi.org/10.5888/pcd16.180447
National Advisory Committee on Rural Health and Human Services (2019) Examining Rural Cancer Prevention and Control Efforts: Policy Brief and Recommendations to the Secretary https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2019-Cancer-Control.pdf
Meissner HI, Breen N, Coyne C, Legler JM, Green DT, Edwards BK (1998) Breast and cervical cancer screening interventions: an assessment of the literature. Cancer Epidemiol Biomark Prev 7(10):951–961
Chan DNS, So WKW (2015) A systematic review of randomised controlled trials examining the effectiveness of breast and cervical cancer screening interventions for ethnic minority women. Eur J Oncol Nurs 19(5):536–553. https://doi.org/10.1016/j.ejon.2015.02.015
Probst JC, Moore CG, Glover SH, Samuels ME (2004) Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health 94(10):1695–1703. https://doi.org/10.2105/ajph.94.10.1695
Ratcliffe M, Burd C, Holder K, Fields A (2016) Defining rural at the US Census Bureau. Am Community Survey Geogr Brief. https://doi.org/10.13140/RG.2.2.16410.64969
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E (2018) Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 18(1):143. https://doi.org/10.1186/s12874-018-0611-x
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB (2015) Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 13(3):141–146
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850%JAnnalsofInternalMedicine
Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, Melillo S, Carvalho M, Taplin S, Bastani R, Rimer BK, Vernon SW, Melvin CL, Taylor V, Fernandez M, Glanz K (2012) Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med 43(1):97–118. https://doi.org/10.1016/j.amepre.2012.04.009
Gellert K, Braun KL, Morris R, Starkey V (2006) The `Ohana Day Project: a community approach to increasing cancer screening. Prev Chron Dis 3(3):A99
Bencivenga M, DeRubis S, Leach P, Lotito L, Shoemaker C, Lengerich EJ (2008) Community partnerships, food pantries, and an evidence-based intervention to increase mammography among rural women. J Rural Health 24(1):91–95. https://doi.org/10.1111/j.1748-0361.2008.00142.x
Luque JS, Tarasenko YN, Reyes-Garcia C, Alfonso ML, Suazo N, Rebing L, Ferris DG (2017) Salud es Vida: a cervical cancer screening intervention for rural Latina immigrant women. J Cancer Educ 32(4):690–699
Katz ML, Tatum CM, Degraffinreid CR, Dickinson S, Paskett ED (2007) Do cervical cancer screening rates increase in association with an intervention designed to increase mammography usage? J Women’s Health 16(1):24–35. https://doi.org/10.1089/jwh.2006.0071
Thompson B, Carosso EA, Jhingan E, Wang L, Holte SE, Byrd TL, Benavides MC, Lopez C, Martinez-Gutierrez J, Ibarra G, Gonzalez VJ, Gonzalez NE, Duggan CR (2016) Results of a randomized controlled trial to increase cervical cancer screening among rural Latinas. Cancer 123(4):666–674. https://doi.org/10.1002/cncr.30399
Falk D, Cubbin C, Jones B, Carrillo-Kappus K, Crocker A, Rice C (2016) Increasing breast and cervical cancer screening in rural and border Texas with friend to friend plus patient navigation. J Cancer Educ. https://doi.org/10.1007/s13187-016-1147-6
Nuño T, Martinez ME, Harris R, García F (2011) A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.–Mexico border: a randomized controlled trial. Cancer Causes Control 22(3):367–374. https://doi.org/10.1007/s10552-010-9705-4
Thompson B, Coronado G, Chen L, Islas I (2006) Celebremos la salud! a community randomized trial of cancer prevention (United States). Cancer Causes Control 17(5):733–746
US Census Bureau (2010) Census regions and divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
U.S. Preventive Services Task Force (2018) Final Update Summary: Breast Cancer: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1?ds=1&s=breast. Accessed Sept 24, 2018
U.S. Preventive Services Task Force (2018) Final update summary: Cervical cancer: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1?ds=1&s=breast. Accessed Sept 24, 2018
Oeffinger KC, Fontham EH, Etzioni R et al (2015) Breast cancer screening for women at average risk: 2015 guideline update from American Cancer Society. JAMA 314(15):1599–1614. https://doi.org/10.1001/jama.2015.12783
Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, Garcia FAR, Moriarty AT, Waxman AG, Wilbur DC, Wentzensen N, Downs LS, Spitzer M, Moscicki A-B, Franco EL, Stoler MH, Schiffman M, Castle PE, Myers ER (2012) American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin 62(3):147–172. https://doi.org/10.3322/caac.21139
Glanz K, Rimer BK, Viswanath K (2008) Health behavior and health education: theory, research, and practice. Wiley, Hoboken
Green LW, Kreuter MW (1993) Health promotion planning: an educational and ecological approach. McGraw-Hill, New York
Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, Fiore C, Harlow LL, Redding CA, Rosenbloom D (1994) Stages of change and decisional balance for 12 problem behaviors. Health Psychol 13(1):39
McGuire WJ (1984) Public communication as a stratey for inducing health-promoting behaviorial change. Prev Med 13:299–319
Bracht NF (1999) Health promotion at the community level: new advances, vol 15. Sage Publications, Thousand Oaks
Sheeran P, Orbell S (2000) Using implementation intentions to increase attendance for cervical cancer screening. Health Psychol 19(3):283
Slater JS, Nim Ha C, Malone ME, McGovern P, Madigan SD, Finnegan JR, Casey-Paal AL, Margolis KL, Lurie N (1998) A randomized community trial to increase mammography utilization among low-income women living in public housing. Prev Med 27(6):862–870. https://doi.org/10.1006/pmed.1998.0370
Community Preventive Services Task Force (2013) Increasing Cancer Screening: One-on-One Education for Clients. Guide to Community Preventive Services. https://www.thecommunityguide.org/sites/default/files/assets/Cancer-Screening-One-on-One-Education.pdf. Accessed Sept 24, 2018
Sohl SJ, Moyer A (2007) Tailored interventions to promote mammography screening: a meta-analytic review. Prev Med 45(4):252–261. https://doi.org/10.1016/j.ypmed.2007.06.009
Myers RE, Randa S, Terry H, Michael R, Vernon WS, James C, Thomas W, Jocelyn A, Richard W (2007) A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening. Cancer 110(9):2083–2091. https://doi.org/10.1002/cncr.23022
Baron RC, Rimer BK, Breslow RA, Coates RJ, Kerner J, Melillo S, Habarta N, Kalra GP, Chattopadhyay S, Wilson KM, Lee NC, Mullen PD, Coughlin SS, Briss PA (2008) Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening: a systematic review. Am J Prev Med 35(1):S34–S55. https://doi.org/10.1016/j.amepre.2008.04.002
U.S. Department of Health and Human Services HRSA, Maternal and Child Health Bureau (2013) Rural and Urban Women. Women’s Health USA 2013
Community Preventive Services Task Force (2017) Multicomponent Interventions to Increase Cancer Screening—Breast Cancer. Accessed Apr 1, 2019
Administration HRaS Defining Rural Population. Health Resources and Services Administration (HRSA). https://www.hrsa.gov/rural-health/about-us/definition/index.html. Accessed Sept 24, 2018
Wheeler SB, Davis MM (2017) “Taking the bull by the horns”: four principles to align public health, primary care, and community efforts to improve rural cancer control. J Rural Health 33(4):345–349
Pollard K, Jacobsen LA (2012) The Appalachian region: a data overview from the 2006–2010 American Community Survey Chartbook. Appalachian Regional Commission, Washington, DC
The Appalachian Region. Appalachian Regional Commission. https://www.arc.gov/appalachian_region/TheAppalachianRegion.asp. Accessed Mar 29, 2019
Maps by topic: economic status. Appalachian Regional Commission. https://www.arc.gov/research/MapsofAppalachia.asp?F_CATEGORY_ID=1. Accessed Mar 29, 2019
Zahnd WE, Jenkins WD, Mueller-Luckey GS (2017) Cancer mortality in the Mississippi Delta region: descriptive epidemiology and needed future research and interventions. J Health Care Poor Unders 28(1):315–328
Delta Regional Authority (2015) Today’s Delta 2.0. Clarksdale, MS: Delta Regional Authority. https://www.dra.gov/images/uploads/content_files/Todays_Delta_FINAL_print-w-borders.pdf. Accessed Mar 29 2019
Falk D (2018) A mixed methods review of education and patient navigation interventions to increase breast and cervical cancer screening for rural women. Social Work Public Health 33(3):173–186
Acknowledgments
All authors have read and approved the abstract. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC) or Oak Ridge Institute for Science and Education (ORISE). Ms. Atere-Roberts’ role as an author of this manuscript was initially supported by her appointment to the Research Participation Program at the CDC administered by ORISE through an interagency agreement between the U.S. Department of Energy and CDC. Ms. Atere-Roberts is currently affiliated with the University of North Carolina at Chapel Hill.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Atere-Roberts, J., Smith, J.L. & Hall, I.J. Interventions to increase breast and cervical cancer screening uptake among rural women: a scoping review. Cancer Causes Control 31, 965–977 (2020). https://doi.org/10.1007/s10552-020-01340-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01340-x