Abstract
Background
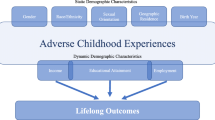
Adverse childhood experiences (ACEs) have been associated with higher odds of cancer in adulthood. One potential explanation for this association is the impact of ACEs on cancer screening. To address this shortcoming, this study examined how ACEs were associated with current compliance and ever use of prostate, breast, cervical, and colorectal cancer screening.
Methods
Data from the 2014 Kansas Behavioral Risk Factor Surveillance System were used (n = 11,794). Logistic regressions were used to calculate odds of cancer screening behaviors from each of nine different ACE items and a count of ACEs.
Results
Individual ACE items were associated with lower odds of compliance with PSA screening, clinical breast exam, and pap test guidelines. Certain ACEs were associated with increased odds of compliance with colorectal cancer screening guidelines among women and lower odds of compliance among men. ACEs were associated with ever screening for PSA and ever use of colonoscopy or sigmoidoscopy among men and women. Physical abuse was most consistently associated with cancer screening, across outcomes.
Conclusions
Most significant associations showed that specific ACEs were associated with lower odds of cancer screening. Therefore, efforts should be made to promote screening among those with histories of ACEs.
Similar content being viewed by others
References
Meester RG, Doubeni CA, Zauber AG et al (2015) Public health impact of achieving 80% colorectal cancer screening rates in the United States by 2018. Cancer 121:2281–2285
Vaccarella S, Franceschi S, Engholm G, Lönnberg S, Khan S, Bray F (2014) 50 years of screening in the Nordic countries: quantifying the effects on cervical cancer incidence. Br J Cancer 111:965–969
Myers ER, Moorman P, Gierisch JM et al (2015) Benefits and harms of breast cancer screening: a systematic review. Jama 314:1615–1634
Jemal A, Fedewa SA, Ma J et al (2015) Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. Jama 314:2054–2061
Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. (2014) Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ Br Med J 348:g366
Rutten LJF, Nelson DE, Meissner HI. (2004) Examination of population-wide trends in barriers to cancer screening from a diffusion of innovation perspective (1987–2000). Prev Med 38:258–268
Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. (2005) Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Med Care 43:939–944
Hsia J, Kemper E, Kiefe C et al. (2000) The importance of health insurance as a determinant of cancer screening: evidence from the women’s health initiative. Prev Med. 31:261–270
Farley M, Golding JM, Minkoff JR. (2002) Is a history of trauma associated with a reduced likelihood of cervical cancer screening?. J Fam Pract 51:827–831
Alcalá HE, Keim-Malpass J, Mitchell E (2017) Colorectal cancer screening and adverse childhood experiences: which adversities matter? Child Abuse Negl 69:145–150
Alcalá HE, Mitchell E, Keim-Malpass J (2017) Adverse childhood experiences and cervical cancer screening. J Women’s Health 26:58–63
Holman DM, Ports KA, Buchanan ND et al (2016) The association between adverse childhood experiences and risk of cancer in adulthood: a systematic review of the literature. Pediatrics 138:S81–S91
Brown MJ, Thacker LR, Cohen SA (2013) Association between adverse childhood experiences and diagnosis of cancer. PloS ONE 8:e65524
Brown DW, Anda RF, Felitti VJ et al (2010) Adverse childhood experiences are associated with the risk of lung cancer: a prospective cohort study. BMC Public Health 10:20
Kelly-Irving M, Lepage B, Dedieu D et al (2013) Childhood adversity as a risk for cancer: findings from the 1958 British birth cohort study. BMC Public Health 13:767
Mouton CP, Hargreaves MK, Liu J, Fadeyi S, Blot WJ (2016) Adult cancer risk behaviors associated with adverse childhood experiences in a low income population in the southeastern United States. J Health Care Poor Underserved 27:68–83
Felitti VJ, Anda RF, Nordenberg D et al. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med 14:245–258
Society AC. (2017) History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms. American Cancer Society
US Preventive Services Task Force (2008) Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med 149:627
Martuzzi M, Elliott P (1998) Estimating the incidence rate ratio in cross-sectional studies using a simple alternative to logistic regression. Ann Epidemiol 8:52–55
Tamhane AR, Westfall AO, Burkholder GA, Cutter GR (2016) Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Stat Med 35:5730–5735
Cadman L, Waller J, Ashdown-Barr L, Szarewski A (2012) Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plan Reprod Health Care. 38: 214 – 20
Ackerson K (2012) A history of interpersonal trauma and the gynecological exam. Qual Health Res. 22:679–688
Arrossi S, Thouyaret L, Herrero R et al. Effect of self-collection of HPV DNA offered by community health workers at home visits on uptake of screening for cervical cancer (the EMA study): a population-based cluster-randomised trial. Lancet Glob Health. 3: e85-e94
Arrossi S, Paolino M, Thouyaret L, Laudi R, Campanera A (2017) Evaluation of scaling-up of HPV self-collection offered by community health workers at home visits to increase screening among socially vulnerable under-screened women in Jujuy Province, Argentina. Implement Sci 12: 17
Smith M, Lew JB, Simms K, Canfell K (2016) Impact of HPV sample self-collection for underscreened women in the renewed Cervical Screening Program. Med J Aust 204:1941e-7
Albertsen PC. (2010) Efficacy vs effectiveness in prostate-specific antigen screening. J Natl Cancer Inst 102: 288–289
Slatkoff S, Gamboa S, Zolotor AJ, Mounsey AL, Jones K (2011) PSA testing: when it’s useful, when it’s not. J Fam Pract 60:357–360
Gulati R, Tsodikov A, Wever EM et al. (2012) The impact of PLCO control arm contamination on perceived PSA screening efficacy. Cancer Causes Control 23:827–835
Alcalá HE, Tomiyama AJ, von Ehrenstein OS (2017) Gender differences in the association between adverse childhood experiences and cancer. Women’s Health Issues 27:625–631
Alcalá HE. (2016) Making the connection between child abuse and cancer: definitional, methodological, and theoretical issues. Soc Theor Health 14:458–474
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alcalá, H.E., Mitchell, E.M. & Keim-Malpass, J. Heterogeneous impacts: adverse childhood experiences and cancer screening. Cancer Causes Control 29, 343–351 (2018). https://doi.org/10.1007/s10552-018-1007-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-018-1007-2