Abstract
Alcohol consumption is postulated to be a risk factor for pancreatic cancer (PCA), but clarification of degree of risk related to consumption characteristics is lacking. We examined the association between alcohol consumption and PCA in a population-based case–control study (532 cases, 1,701 controls) in the San Francisco Bay Area. Population-based controls were frequency-matched by sex, age within 5-year categories and county of residence to cases identified by the cancer registry’s rapid case ascertainment. Detailed alcohol consumption data, including binge drinking (≥5 drinks/day), were collected during in-person interviews. Odds ratios (OR) and 95% confidence intervals (95% CI) were computed using adjusted unconditional logistic regression. Depending on dose, duration, and pattern of drinking, ORs were increased 1.5- to 6-fold among men but not women. In men, ORs increased with increasing overall alcohol consumption (22–35 drinks/week OR = 2.2, 95% CI = 1.1–4.0; ≥35 drinks/week OR = 2.6, 95% CI = 1.3–5.1, p-trend = 0.04). Most notable were effects with a history of binge drinking (OR = 3.5, 95% CI = 1.6–7.5) including increased number of drinks per day (p-trend = 0.002), and increased years of binge drinking (p-trend = 0.0006). In fully adjusted models that included smoking and other confounders, ORs for binge drinking in men were somewhat higher than in age-adjusted models. Results from our detailed analyses provide support for heavy alcohol consumption (including binge drinking) as a risk factor for PCA in men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is diagnosed in over 124,000 individuals globally per year and is nearly uniformly fatal in the developing and developed areas, with the lowest overall 5-year survival rate of all site-specific cancers [1, 2]. The lethality of pancreatic cancer requires dedicated attention to understanding the causes and modifiable risk factors associated with development of this disease.
Alcohol has been identified inconsistently as a risk factor for pancreatic cancer [3–42]. Particularly important reasons for inconsistency that may have resulted in report of no association between alcohol consumption and pancreatic cancer may have included incomplete assessment and analysis of dose of alcohol consumption risk across wide ranges, as well as pattern of alcohol consumption. Thus, more large population-based studies are required to examine this association while adjusting for other putative risk factors, and considering the relationship of dose and pattern of alcohol exposure. We conducted the current analyses as part of a large, population-based case–control study in the San Francisco Bay Area to examine the relationship between pancreatic cancer and alcohol consumption, with particular attention to the associated exposure characteristics of timing of consumption onset, duration, and dose, including binge drinking.
Materials and methods
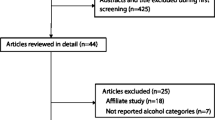
Detailed methods for this case–control study have been published elsewhere [43–49]; a brief summary of methods follows. Cases were newly diagnosed with adenocarcinoma of the exocrine pancreas between 1995 and 1999, residents of one of six Bay Area counties at the time of diagnosis, and were identified using rapid case ascertainment by the Northern California Cancer Center. Diagnoses of pancreatic cancer were confirmed by participants’ physicians and by the Surveillance, Epidemiology and End Results abstracts that included histologic confirmation of disease when available. Eligible cases that were included were alive at contact (no proxy interviews were conducted), 21–85 years of age, and able to complete an interview in English.
Control participants were selected from the same target population as the cases using random-digit dial and were frequency-matched to cases by sex, age within 5-year categories and county. Identification of controls older than 65 years was supplemented by random selection from the United States Health-Care Finance Administration (now the Centers for Medicare and Medicaid Services) lists. Approximately three controls were identified for each case participant. Sixty-seven percent of eligible cases and 67% of eligible controls completed an in-person interview using structured questionnaires. Written consent was obtained from each study participant prior to the interview. This study was reviewed and approved by the University of California San Francisco Committee on Human Research.
Alcohol consumption
Participants self-reported their history of alcohol consumption, including type of alcohol consumed (beer, wine, and/or liquor). One drink was defined as one can, bottle or 12 oz glass of beer, one 4 oz glass of wine, or one shot of liquor because they each contain approximately 14 g of alcohol. The average weekly consumption of beer, wine, and liquor was recorded separately by decade of age, starting in their 20s, i.e., 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, and 80+. Lifetime total alcohol consumption was computed by summing the total number of drinks of beer, wine, and liquor in each decade. Average number of drinks consumed per week in the past decade + current decade; the past two decades + current decade; and the past three decades + current decade also were determined. Participants also were grouped as: never drinkers, exclusive consumers of beer, wine or liquor, and those who consumed two or three types of alcohol. Under the a priori hypothesis that the pattern of alcohol consumption of alcohol might be related to pancreatic cancer, binge alcohol consumption was assessed as frequency, volume, and duration of alcohol consumption beyond their usual drinking patterns. For analyses, we defined “binge drinking” as consumption of five or more drinks per day (70 g of alcohol), following the definition used by the United States Behavioral Risk Factor Surveillance System study [50, 51]. For ease of comparison, analyses of the primary measure of risk (lifetime weekly alcohol consumption) were conducted using categories from an earlier similar study of pancreatic cancer and alcohol consumption [16]. For other categories of alcohol consumption, weekly alcohol consumption was categorized into quartiles based on the frequency distribution among the controls. Because binge drinking was determined separately from usual drinking patterns, individuals who were characterized as binge drinkers were distributed across the range of quartiles of typical drinking patterns. For example, some binge drinkers who on occasion drank five or more drinks per day were included in lower quartiles of overall alcohol consumption based upon the average number of drinks typically consumed per week.
Statistical methods
Demographic data and data for potential confounders were collected and defined as follows: race was self-reported, and categorized as white, black/African American, Asian/Pacific Islander, or other. Body mass index (BMI) was estimated from usual adult weight and height [weight (kg)/height (m2)], and was categorized based on World Health Organization criteria: <25.0 (lean to normal), 25.0–29.9 (overweight), and ≥30.0 (obese). Frequency of recreational physical activity for at least 30 min per episode was recorded as never or <1/month, 1–2/month, 3–4/month, 2–3/week, 4–6/week, and ≥1/day. Participants were defined as smokers if they had smoked ≥100 cigarettes, or cigars or pipes at least once a month for ≥6 months in their lifetime. Cigarette smokers were categorized into four groups: never smokers; former smokers (two groups) who quit >15 years ago or 1–15 years prior to diagnosis/interview; and current smokers including those who had quit within 1 year of diagnosis/interview. Total caloric intake (expressed as kilocalories per day), vitamin intake (vitamins A, B1–B12, C, E, D), and calcium intake were estimated based on results of a food-frequency questionnaire and divided into quartiles based on consumption among controls as described previously [52, 53]. Education level was categorized as less than high school graduate, high school graduate, some college, college graduate, and graduate work. Participants also were asked if they ever had been told by a physician that they had diabetes or pancreatitis. Odds ratios (OR) and 95% confidence intervals (95% CI) were computed using unconditional logistic regression to estimate the relative risk (hereafter called risk) of pancreatic cancer by categories of alcohol consumption. The reference group for alcohol analyses was those who never drank or drank less than 1 drink per month. Analyses were stratified by sex and adjusted for age. Results for the association between weekly alcohol consumption and pancreatic cancer were further stratified by smoking status–smokers (defined as cigarette, pipe, or cigar smokers and former smokers who quit <15 years prior to interview), versus non-smokers (defined as never smokers, or former smokers who quit ≥ 15 years prior to interview). Former smokers who quit ≥15 years prior to interview were grouped with never smokers as our analyses showed no association between this group and increased pancreatic cancer risk (data not shown). Analyses of alcohol consumption and risk restricted only to current smokers also are provided. Because of sample size constraints, the referent group for analyses restricted to smokers was those who drank less than 1 drink/month over their lifetime, or ≤4 drinks/week in the 20 years prior to interview. Analyses stratified by type of alcohol also are presented. For comparability with other studies and our earlier published results of data from this study, we present results from parsimonious models adjusted for age alone, and from multivariable models additionally adjusted for potential confounders of race, education, smoking, history of diabetes, BMI, caloric intake, and physical activity. Exploratory analyses adjusting for history of pancreatitis also were conducted, but results are not presented as risk estimates did not differ by at least 10%. Odds ratios and 95% CIs are not presented in tables when the number of observations was five or fewer. All statistical tests were two-sided and considered statistically significant when p < 0.05. Statistical analyses were conducted using SAS software V9.1 (SAS Institute, Inc., Cary, NC) and results are presented for age-adjusted and final multivariable models.
Results
Characteristics of the study population have been reported previously [43–49] and are noted in Table 1. Five hundred and thirty-two eligible cases and 1,701 controls completed in-person interviews. Alcohol consumption was associated with pancreatic cancer among men but not women, with increased risk ranging from 1.5- to 6-fold based on the dose, duration, and pattern of alcohol consumption reported (Tables 2, 3). Results from more detailed analyses pertaining to heavy drinking are limited to men (Tables 2, 3, 4, 5).
Effect of alcohol dose and duration of consumption
Among men, ORs for pancreatic cancer increased with increasing duration and increasing dose of heavy alcohol consumption (all p-trend < 0.04, Table 2). Relative to never or infrequent drinkers, men with the highest lifetime alcohol consumption had a greater than twofold increased risk of pancreatic cancer that remained elevated when assessment of alcohol consumption was limited to the past 20 years (Table 2). Risk was elevated regardless of when in the past the heavy consumption had occurred; ORs ranged from 2 to 2.6 for heavy drinking in the past 10, 20, or 30 years (data not shown). When analyses were restricted to the heaviest drinkers, results showed that risk increased with increasing decades of heavy consumption (>21 drinks/week p-trend = 0.02, >35 drinks/week p-trend = 0.01, Table 2).
Binge drinking and risk
Irregular pattern of heavy alcohol consumption, assessed as binge drinking, was associated with risk of pancreatic cancer (Table 3). A history of binge consumption of large amounts of alcohol (≥5 drinks per drinking episode or >70 g alcohol per episode) [50, 51] conferred a 3.5-fold increased risk of pancreatic cancer in men. Risk was increased regardless of age when binge drinking first occurred, although there was some evidence that risk was greatest for binge drinking that began at 21–30 years of age (p-trend = 0.007). A similar pattern was observed for years since last binge drinking episode. Risk was increased more than threefold regardless of when binge drinking last occurred, although men whose last binge drinking episode occurred 6–10 years before diagnosis/interview had a greater than sixfold increased risk of pancreatic cancer. Dose–response analyses provided additional support that binge drinking increased risk of pancreatic cancer in men. Risk was positively associated with increasing average number of alcoholic drinks consumed during binge drinking (>15 drinks: OR = 4.4, p-trend = 0.002) and with increasing years duration of binge drinking (>10 years: OR = 3.7, p-trend = 0.0006). Risk also was persistently increased regardless of frequency of binge drinking each month. Indeed, there was some evidence that even less frequent binge drinking was associated with the elevated risk in men (OR = 4.3). In fully adjusted models that included smoking and other confounders, ORs for binge drinking in men were somewhat higher than in models adjusted for age only (Table 3).
Effect of dose and pattern of alcohol consumption stratified by smoking status
In smoking-stratified analyses of the association of alcohol consumption with pancreatic cancer among men, most estimates were based on a small number of exposed individuals and were imprecise with wide confidence intervals that included unity with few exceptions (Tables 4, 5). In general, risk of pancreatic cancer was greatest in the highest alcohol consumption-related categories regardless of smoking status. However, results from multivariable analyses suggested that heavy drinkers and the heaviest binge drinkers who were current smokers may be at greater risk of pancreatic cancer than former/never smokers (Table 5, binge drinking >10 years OR = 9.5, 95% CI = 1.8–50, p-trend = 0.01; ≥15 drinks/day during binge drinking OR = 9.5, 95% CI = 1.4–64, p-trend = 0.01; >35 drinks/week during the past 20 years OR = 4.2, 95% CI = 1.6–12, p-trend = 0.002, p-interaction between heavy drinking and smoking status >0.30).
Alcohol type and risk
Analyses of risk of pancreatic cancer stratified by type of alcohol consumed were generally limited by sample size considerations. Significant associations among men by alcohol type or combination of alcohol types were noted for wine (OR = 2.8, 95% CI = 1.2–6.3), consumption of beer and liquor (OR = 2.3, 95% CI = 1.3–4.1), and the combination of beer, wine, and liquor consumption (OR = 1.7, 95% CI = 1.0–2.8). As was observed for the overall analyses, no association between type of alcohol consumption and risk for pancreatic cancer was observed among women.
Discussion
Our results have demonstrated that heavy alcohol consumption and binge drinking were associated with increased risk estimates for pancreatic cancer in men but not among women. Our data further suggested that either binge or consistent heavy alcohol consumption was associated with persistent increased risk of pancreatic cancer regardless of the temporal proximity of consumption to pancreatic cancer diagnosis. Results from smoking-stratified analyses that suggested a possible interaction between current smoking and heavy drinking should be interpreted with caution and require further validation in larger pooled studies, particularly given that the p-interactions for these analyses were >0.3. The association between alcohol consumption and pancreatic cancer in earlier studies has been discordant, with some hospital-based [24–28, 54–59] and population-based case–control [3, 5, 6, 8, 10, 11, 13, 14, 17, 19, 31, 60] and cohort studies [4, 7, 9, 32, 33, 38, 42, 61, 62] showing no association, and other hospital-based [29, 30] and population-based case–control [15, 16, 18] and cohort [20, 21, 34, 36, 37, 41, 63] studies suggesting increased risk. Discordant observations in the published literature may be due to small numbers of cases, residual confounding by risk factors associated with alcohol consumption such as smoking and chronic pancreatitis, unmeasured genetic factors, or absence of detailed data on alcohol exposure [16, 17, 23, 34, 39].
Discordant results due to residual confounding associated with smoking are less likely given that, as one of the few identified risk factors, most epidemiologic studies have included tobacco use in their analyses of alcohol consumption and pancreatic cancer risk. Indeed, in several studies that reported a positive association between alcohol and pancreatic cancer, the association persisted even among non-smokers [16, 17, 20, 36]. In our study, data were consistent with persistent increased risk among non-smokers, but not statistically significant. Notably, the number of never smokers available for analysis in our study required pooling of data from never smokers with those who quit smoking over 15 years prior to interview; this may have biased our estimates comparing risk among non-smokers to smokers toward finding a smaller risk difference than actually present. However, because there was a small sample of never smokers, and the ability to adjust for more detailed smoking characteristics (such as pack-years of smoking) was limited, it is possible that residual confounding due to smoking cannot be completely excluded.
Unmeasured molecular and genetic characteristics within individuals and their cancers also may explain some discordant observations. For example, particular mutations in the K-ras oncogene may be more common in alcohol consumers with pancreatic cancers, and may be initiating or end mediators of pancreas cancer associated with heavy alcohol exposure [23, 64, 65].
Misclassification of alcohol consumption related to recall bias or inadequate measurement of detailed alcohol consumption over time may be a more likely explanation for the discordant published results. The potential for recall bias is inherent to all retrospective studies and also has been noted in several prospective cohort studies [9, 10, 12, 20, 21]. The extensive measures taken in our study to diminish the effects of recall bias are noted below.
Measurement error with respect to characterization of the dose, duration, and pattern of alcohol consumption may explain some discordant findings between alcohol consumption and pancreatic cancer risk [40]. Few population-based studies have analyzed the relationship between pancreas cancer and binge alcohol consumption [6, 14, 16, 61]. Of these, one study observed that increased risks were mainly in the highest categories of alcohol consumption, and were stronger among African Americans than for whites [16]. Although the authors reported no association between pancreatic cancer and binge drinking [16], the definition of binge drinking that was used (≥3 drinks/week) was lower than that used in our analyses based upon the United States Behavioral Risk Factor Surveillance System study [50, 51]. Our observation that binge drinking (≥5 drinks/episode, >70 g of alcohol)—even when occurring years before diagnosis or among moderate alcohol consumers—was associated with increased cancer risk, suggests that the pattern of drinking may be an important mediator of effect. Averaging alcohol exposure over weeks, months, or years, classifying consumption into broad categories, and/or computing lifetime alcohol exposures to measure total consumption, may not accurately assess toxicity that results from high and/or binge doses of alcohol. Thus, use of these methods may limit the ability to identify associations between alcohol exposure and pancreatic cancer.
Several biologic mechanisms have been proposed to explain the observed increased risk of pancreatic cancer related to heavy alcohol consumption. Alcohol may initiate inflammatory responses that result in overt chronic pancreatitis or diabetes mellitus, perhaps via induction of mitogenic stimuli [22, 23]. Alcohol consumption also may lead to asymptomatic chronic pancreatitis that then leads to pancreatic cancer [66–71], although the prevalence of the history of pancreatitis is small in the overall population of pancreatic cancer patients. In addition, oxidative and non-oxidative pancreatic damage due to metabolism of alcohol can initiate inflammatory and fibrotic cascades that may result in subsequent carcinogenesis [22]. Further detailed study of alcohol consumption, including dose, duration, and pattern of exposure, is needed to discern the biologic mechanisms that are important in pancreatic cancer development.
A null or protective association for alcohol and pancreatic cancer among women has been noted in most, [6, 9, 10, 14, 17, 24, 27, 28, 36, 38, 39, 41, 42, 55, 56, 59, 61, 62], but not all [16, 20, 34, 37] earlier studies. In our study, the proportion of women who reported heavy and/or binge drinking was much lower than for men. Therefore, the lack of an observed association may be attributable to sample size constraints. Further research is necessary to understand differences in pancreatic cancer risk between men and women.
Possible limitations of case–control studies should be considered when interpreting our results. Recall bias may be a problem in studies that query people about past events, although the effects of recall bias may have been diminished by requesting that participants report detailed alcohol consumption in multiple ways and over multiple time periods. Interviewers were highly trained and monitored to avoid interviewer bias and data were collected using a standardized questionnaire that included recent and past exposures. Because our results showed consistent trends between pancreatic cancer and dose and duration of alcohol exposure and, as noted earlier, underreporting would have diminished the risk estimates toward the null, recall bias may have had limited influence. Although rapid case ascertainment methods were used, similar to other population-based studies of pancreatic cancer, a large number of patients had died prior to initial contact due to the aggressive nature of the disease. The potential effect of these non-interviewed patients on risk estimates is unknown, as alcohol consumption data were not available for non-interviewed cases who died shortly after diagnosis. Our prior comparison of demographic data from SEER abstracts for interviewed and non-interviewed cases who were identified as part of our study showed that non-interviewed cases tended to be slightly older, with a slightly greater proportion of women than men, somewhat more minorities, fewer known tumor characteristics, and shorter survival times [44].
In summary, our findings support an association between heavy alcohol consumption and pancreatic cancer among men that may be mediated by dose, duration, and pattern of alcohol consumption, including binge drinking. If the observed relationship with heavy alcohol consumption and binge drinking is confirmed by other large studies that have collected detailed alcohol exposure data, targeted interventions to reduce heavy drinking and binge drinking (which is prevalent and increasing in frequency [51, 72]) may be of even greater importance than previously recognized. The difficulty of early diagnosis, and the rapid progression from diagnosis to death calls for concerted cancer prevention efforts to identify and intervene on all potentially modifiable risk factors for pancreatic cancer, including alcohol consumption.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59(4):225–249
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
Bueno de Mesquita HB, Maisonneuve P, Moerman CJ, Runia S, Boyle P (1992) Lifetime consumption of alcoholic beverages, tea and coffee and exocrine carcinoma of the pancreas: a population-based case–control study in The Netherlands. Int J Cancer 50(4):514–522
Norell SE, Ahlbom A, Erwald R, Jacobson G, Lindberg-Navier I, Olin R et al (1986) Diet and pancreatic cancer: a case–control study. Am J Epidemiol 124(6):894–902
Lyon JL, Mahoney AW, French TK, Moser R Jr (1992) Coffee consumption and the risk of cancer of the exocrine pancreas: a case–control study in a low-risk population. Epidemiology 3(2):164–170
Mack TM, Yu MC, Hanisch R, Henderson BE (1986) Pancreas cancer and smoking, beverage consumption, and past medical history. J Natl Cancer Inst 76(1):49–60
Farrow DC, Davis S (1990) Risk of pancreatic cancer in relation to medical history and the use of tobacco, alcohol and coffee. Int J Cancer 45(5):816–820
Jain M, Howe GR, St. Louis P, Miller AB (1991) Coffee and alcohol as determinants of risk of pancreas cancer: a case–control study from Toronto. Int J Cancer 47(3):384–389
Michaud DS, Giovannucci E, Willett WC, Colditz GA, Fuchs CS (2001) Coffee and alcohol consumption and the risk of pancreatic cancer in two prospective United States cohorts. Cancer Epidemiol Biomarkers Prev 10(5):429–437
Inoue M, Tajima K, Takezaki T, Hamajima N, Hirose K, Ito H et al (2003) Epidemiology of pancreatic cancer in Japan: a nested case–control study from the Hospital-based Epidemiologic Research Program at Aichi Cancer Center (HERPACC). Int J Epidemiol 32(2):257–262
Baghurst PA, McMichael AJ, Slavotinek AH, Baghurst KI, Boyle P, Walker AM (1991) A case–control study of diet and cancer of the pancreas. Am J Epidemiol 134(2):167–179
Lin Y, Tamakoshi A, Kawamura T, Inaba Y, Kikuchi S, Motohashi Y et al (2002) A prospective cohort study of cigarette smoking and pancreatic cancer in Japan. Cancer Causes Control 13(3):249–254
Ghadirian P, Simard A, Baillargeon J (1991) Tobacco, alcohol, and coffee and cancer of the pancreas. A population-based, case–control study in Quebec, Canada. Cancer 67(10):2664–2670
Ji BT, Chow WH, Dai Q, McLaughlin JK, Benichou J, Hatch MC et al (1995) Cigarette smoking and alcohol consumption and the risk of pancreatic cancer: a case–control study in Shanghai, China. Cancer Causes Control 6(4):369–376
Olsen GW, Mandel JS, Gibson RW, Wattenberg LW, Schuman LM (1989) A case–control study of pancreatic cancer and cigarettes, alcohol, coffee and diet. Am J Public Health 79(8):1016–1019
Silverman DT, Brown LM, Hoover RN, Schiffman M, Lillemoe KD, Schoenberg JB et al (1995) Alcohol and pancreatic cancer in blacks and whites in the United States. Cancer Res 55(21):4899–4905
Villeneuve PJ, Johnson KC, Hanley AJ, Mao Y (2000) Alcohol, tobacco and coffee consumption and the risk of pancreatic cancer: results from the Canadian Enhanced Surveillance System case–control project. Canadian Cancer Registries Epidemiology Research Group. Eur J Cancer Prev 9(1):49–58
Partanen TJ, Vainio HU, Ojajarvi IA, Kauppinen TP (1997) Pancreas cancer, tobacco smoking and consumption of alcoholic beverages: a case–control study. Cancer Lett 116(1):27–32
Zatonski WA, Boyle P, Przewozniak K, Maisonneuve P, Drosik K, Walker AM (1993) Cigarette smoking, alcohol, tea and coffee consumption and pancreas cancer risk: a case–control study from Opole, Poland. Int J Cancer 53(4):601–607
Harnack LJ, Anderson KE, Zheng W, Folsom AR, Sellers TA, Kushi LH (1997) Smoking, alcohol, coffee, and tea intake and incidence of cancer of the exocrine pancreas: the Iowa Women’s Health Study. Cancer Epidemiol Biomarkers Prev 6(12):1081–1086
Zheng W, McLaughlin JK, Gridley G, Bjelke E, Schuman LM, Silverman DT et al (1993) A cohort study of smoking, alcohol consumption, and dietary factors for pancreatic cancer (United States). Cancer Causes Control 4(5):477–482
Go VL, Gukovskaya A, Pandol SJ (2005) Alcohol and pancreatic cancer. Alcohol 35(3):205–211
Welsch T, Kleeff J, Seitz HK, Buchler P, Friess H, Buchler MW (2006) Update on pancreatic cancer and alcohol-associated risk. J Gastroenterol Hepatol 21(Suppl 3):S69–S75
Bouchardy C, Clavel F, La Vecchia C, Raymond L, Boyle P (1990) Alcohol, beer and cancer of the pancreas. Int J Cancer 45(5):842–846
Kalapothaki V, Tzonou A, Hsieh CC, Toupadaki N, Karakatsani A, Trichopoulos D (1993) Tobacco, ethanol, coffee, pancreatitis, diabetes mellitus, and cholelithiasis as risk factors for pancreatic carcinoma. Cancer Causes Control 4(4):375–382
Soler M, Chatenoud L, La Vecchia C, Franceschi S, Negri E (1998) Diet, alcohol, coffee and pancreatic cancer: final results from an Italian study. Eur J Cancer Prev 7(6):455–460
Tavani A, Pregnolato A, Negri E, La Vecchia C (1997) Alcohol consumption and risk of pancreatic cancer. Nutr Cancer 27(2):157–161
Clavel F, Benhamou E, Auquier A, Tarayre M, Flamant R (1989) Coffee, alcohol, smoking and cancer of the pancreas: a case–control study. Int J Cancer 43(1):17–21
Durbec JP, Chevillotte G, Bidart JM, Berthezene P, Sarles H (1983) Diet, alcohol, tobacco and risk of cancer of the pancreas: a case–control study. Br J Cancer 47(4):463–470
Cuzick J, Babiker AG (1989) Pancreatic cancer, alcohol, diabetes mellitus and gall-bladder disease. Int J Cancer 43(3):415–421
Gold EB, Gordis L, Diener MD, Seltser R, Boitnott JK, Bynum TE et al (1985) Diet and other risk factors for cancer of the pancreas. Cancer 55(2):460–467
Shibata A, Mack TM, Paganini-Hill A, Ross RK, Henderson BE (1994) A prospective study of pancreatic cancer in the elderly. Int J Cancer 58(1):46–49
Hiatt RA, Klatsky AL, Armstrong MA (1988) Pancreatic cancer, blood glucose and beverage consumption. Int J Cancer 41(6):794–797
Ye W, Lagergren J, Weiderpass E, Nyren O, Adami HO, Ekbom A (2002) Alcohol abuse and the risk of pancreatic cancer. Gut 51(2):236–239
Thygesen LC, Mikkelsen P, Andersen TV, Tonnesen H, Juel K, Becker U et al (2009) Cancer incidence among patients with alcohol use disorders—long-term follow-up. Alcohol Alcohol 44(4):387–391
Jiao L, Silverman DT, Schairer C, Thiebaut AC, Hollenbeck AR, Leitzmann MF et al (2009) Alcohol use and risk of pancreatic cancer: the NIH-AARP Diet and Health Study. Am J Epidemiol 169(9):1043–1051
Genkinger JM, Spiegelman D, Anderson KE, Bergkvist L, Bernstein L, van den Brandt PA et al (2009) Alcohol intake and pancreatic cancer risk: a pooled analysis of fourteen cohort studies. Cancer Epidemiol Biomarkers Prev 18(3):765–776
Rohrmann S, Linseisen J, Vrieling A, Boffetta P, Stolzenberg-Solomon RZ, Lowenfels AB et al (2009) Ethanol intake and the risk of pancreatic cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Causes Control 20(5):785–794
Tramacere I, Scotti L, Jenab M, Bagnardi V, Bellocco R, Rota M et al (2009) Alcohol drinking and pancreatic cancer risk: a meta-analysis of the dose-risk relation. Int J Cancer 126(6):1474–1486
Johansen D, Borgstrom A, Lindkvist B, Manjer J (2009) Different markers of alcohol consumption, smoking and body mass index in relation to risk of pancreatic cancer. A prospective cohort study within the Malmo Preventive Project. Pancreatology 9(5):677–686
Heinen MM, Verhage BA, Ambergen TA, Goldbohm RA, van den Brandt PA (2009) Alcohol consumption and risk of pancreatic cancer in the Netherlands cohort study. Am J Epidemiol 169(10):1233–1242
Allen NE, Beral V, Casabonne D, Kan SW, Reeves GK, Brown A et al (2009) Moderate alcohol intake and cancer incidence in women. J Natl Cancer Inst 101(5):296–305
Chan JM, Wang F, Holly EA (2005) Vegetable and fruit intake and pancreatic cancer in a population-based case–control study in the San Francisco bay area. Cancer Epidemiol Biomarkers Prev 14(9):2093–2097
Eberle CA, Bracci PM, Holly EA (2005) Anthropometric factors and pancreatic cancer in a population-based case–control study in the San Francisco Bay area. Cancer Causes Control 16(10):1235–1244
Holly EA, Eberle CA, Bracci PM (2003) Prior history of allergies and pancreatic cancer in the San Francisco Bay area. Am J Epidemiol 158(5):432–441
Holly EA, Chaliha I, Bracci PM, Gautam M (2004) Signs and symptoms of pancreatic cancer: a population-based case–control study in the San Francisco Bay area. Clin Gastroenterol Hepatol 2(6):510–517
Hoppin JA, Tolbert PE, Holly EA, Brock JW, Korrick SA, Altshul LM et al (2000) Pancreatic cancer and serum organochlorine levels. Cancer Epidemiol Biomarkers Prev 9(2):199–205
Wang F, Gupta S, Holly EA (2006) Diabetes mellitus and pancreatic cancer in a population-based case–control study in the San Francisco Bay Area, California. Cancer Epidemiol Biomarkers Prev 15(8):1458–1463
Slebos RJ, Hoppin JA, Tolbert PE, Holly EA, Brock JW, Zhang RH et al (2000) K-ras and p53 in pancreatic cancer: association with medical history, histopathology, and environmental exposures in a population-based study. Cancer Epidemiol Biomarkers Prev 9(11):1223–1232
Wechsler H, Nelson TF (2001) Binge drinking and the American college student: what’s five drinks? Psychol Addict Behav 15(4):287–291
Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS (2003) Binge drinking among US adults. JAMA 289(1):70–75
Chan JM, Wang F, Holly EA (2007) Whole grains and risk of pancreatic cancer in a large population-based case–control study in the San Francisco Bay Area, California. Am J Epidemiol 166(10):1174–1185
Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC (1992) Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 135(10):1114–1126 discussion 1127–1136
Talamini G, Bassi C, Falconi M, Sartori N, Salvia R, Rigo L et al (1999) Alcohol and smoking as risk factors in chronic pancreatitis and pancreatic cancer. Dig Dis Sci 44(7):1303–1311
Mizuno S, Watanabe S, Nakamura K, Omata M, Oguchi H, Ohashi K et al (1992) A multi-institute case–control study on the risk factors of developing pancreatic cancer. Jpn J Clin Oncol 22(4):286–291
Falk RT, Pickle LW, Fontham ET, Correa P, Fraumeni JF Jr (1988) Life-style risk factors for pancreatic cancer in Louisiana: a case–control study. Am J Epidemiol 128(2):324–336
Lee CT, Chang FY, Lee SD (1996) Risk factors for pancreatic cancer in orientals. J Gastroenterol Hepatol 11(5):491–495
Manousos O, Trichopoulos D, Koutselinis A, Papadimitriou C, Polychronopoulou A, Zavitsanos X (1981) Epidemiologic characteristics and trace elements in pancreatic cancer in Greece. Cancer Detect Prev 4(1–4):439–442
Gullo L, Pezzilli R, Morselli-Labate AM (1995) Coffee and cancer of the pancreas: an Italian multicenter study. The Italian Pancreatic Cancer Study Group. Pancreas 11(3):223–229
Friedman GD, van den Eeden SK (1993) Risk factors for pancreatic cancer: an exploratory study. Int J Epidemiol 22(1):30–37
Lin Y, Tamakoshi A, Kawamura T, Inaba Y, Kikuchi S, Motohashi Y et al (2002) Risk of pancreatic cancer in relation to alcohol drinking, coffee consumption and medical history: findings from the Japan collaborative cohort study for evaluation of cancer risk. Int J Cancer 99(5):742–746
Stevens RJ, Roddam AW, Spencer EA, Pirie KL, Reeves GK, Green J et al (2009) Factors associated with incident and fatal pancreatic cancer in a cohort of middle-aged women. Int J Cancer 124(10):2400–2405
Heuch I, Kvale G, Jacobsen BK, Bjelke E (1983) Use of alcohol, tobacco and coffee, and risk of pancreatic cancer. Br J Cancer 48(5):637–643
Malats N, Porta M, Corominas JM, Pinol JL, Rifa J, Real FX (1997) Ki-ras mutations in exocrine pancreatic cancer: association with clinico-pathological characteristics and with tobacco and alcohol consumption. PANK-ras I Project Investigators. Int J Cancer 70(6):661–667
Crous-Bou M, Porta M, Lopez T, Jariod M, Malats N, Morales E et al (2009) Lifetime history of alcohol consumption and K-ras mutations in pancreatic ductal adenocarcinoma. Environ Mol Mutagen 50(5):421–430
Steer ML, Waxman I, Freedman S (1995) Chronic pancreatitis. N Engl J Med 332(22):1482–1490
Karlson BM, Ekbom A, Josefsson S, McLaughlin JK, Fraumeni JF Jr, Nyren O (1997) The risk of pancreatic cancer following pancreatitis: an association due to confounding? Gastroenterology 113(2):587–592
Bansal P, Sonnenberg A (1995) Pancreatitis is a risk factor for pancreatic cancer. Gastroenterology 109(1):247–251
Ekbom A, McLaughlin JK, Karlsson BM, Nyren O, Gridley G, Adami HO et al (1994) Pancreatitis and pancreatic cancer: a population-based study. J Natl Cancer Inst 86(8):625–627
Lowenfels AB, Maisonneuve P, Cavallini G, Ammann RW, Lankisch PG, Andersen JR et al (1993) Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N Engl J Med 328(20):1433–1437
Wiersema MJ, Hawes RH, Lehman GA, Kochman ML, Sherman S, Kopecky KK (1993) Prospective evaluation of endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in patients with chronic abdominal pain of suspected pancreatic origin. Endoscopy 25(9):555–564
Flowers NT, Naimi TS, Brewer RD, Elder RW, Shults RA, Jiles R (2008) Patterns of alcohol consumption and alcohol-impaired driving in the United States. Alcohol Clin Exp Res 32(4):639–644
Acknowledgments
This work was supported in part by National Cancer Institute grants CA59706, CA108370, CA109767, CA89726 (E. A. Holly, PI), and by the Rombauer Pancreatic Cancer Research Fund. Cancer incidence data collection was supported by the California Department of Public Health, the National Cancer Institute’s Surveillance, Epidemiology and End Results Program contract N01-PC-35136 awarded to the Northern California Cancer Center. The work was also supported by National Institutes of Health grant number 1 KL2 RR024983-01, titled, “North and Central Texas Clinical and Translational Science Initiative” (Milton Packer, M.D., PI) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research, and its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Gupta, S., Wang, F., Holly, E.A. et al. Risk of pancreatic cancer by alcohol dose, duration, and pattern of consumption, including binge drinking: a population-based study. Cancer Causes Control 21, 1047–1059 (2010). https://doi.org/10.1007/s10552-010-9533-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9533-6