Abstract
Purpose
Physical activity is associated with lower breast cancer risk, especially in postmenopausal women. Associations in premenopausal women are less well established.
Methods
We evaluated recreational physical activity and breast cancer risk in the Nurses’ Health Study (NHS) and NHSII (187,278 women; n = 12,785 breast cancers; follow-up: NHS = 1986–2016, NHSII = 1989–2017) by menopausal status and estrogen (ER) and progesterone (PR) receptor status. Physical activity was evaluated as updated cumulative average of metabolic equivalent of task (MET)-h/week. Cox proportional hazards models were used to estimate multivariable hazard ratios (HR) and 95% confidence intervals (CI).
Results
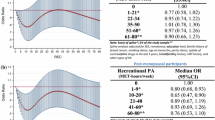
Recreational physical activity was inversely associated with breast cancer risk in pre- and postmenopausal women. Higher activity levels were associated with lower risk of ER+/PR + breast cancer in both pre- and postmenopausal women (e.g., total recreational activity, ≥ 27 vs < 3 MET-h/week, premenopausal HR = 0.83, 95%CI = (0.70–0.99), postmenopausal HR = 0.86 (0.78–0.95); pheterogeneity = 0.97). Results were attenuated with adjustment for current body mass index (BMI) among postmenopausal, but not premenopausal, women (e.g., ≥ 27 vs < 3 MET-h/week, premenopausal HR = 0.83 (0.69–0.98); postmenopausal HR = 0.95 (0.85–1.05); pheterogeneity = 0.99). In analyses of moderate-vigorous activity and breast cancer risk, no heterogeneity by menopausal status was observed (phet ≥ 0.53; e.g., ≥ 27 vs < 3 MET-h/week, ER+/PR+, premenopausal HR = 0.88 (0.69–1.11); postmenopausal HR = 0.71 (0.58–0.88). No associations were observed for ER−/PR− disease.
Conclusions
Recreational physical activity was associated with lower breast cancer risk in both pre- and postmenopausal women, supporting recreational physical activity as an accessible, modifiable exposure associated with reduced breast cancer risk regardless of menopausal status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Higher levels of physical activity are consistently associated with lower risk of breast cancer for postmenopausal women, while associations for premenopausal women remain less clear [1], in large part due to the relatively small number of premenopausal cases with pre-diagnosis activity data in individual prospective cohort studies. The World Cancer Research Fund International (WCRF): Continuous Update Project (CUP) 2018 Expert Report [2] summarized associations between physical activity and breast cancer and reported inverse associations between vigorous activity and both pre- and postmenopausal breast cancer, while total and recreational activity were only significantly associated with postmenopausal disease and with the associations for premenopausal women classified as “limited-suggestive” [1, 2]. In contrast, a more recent study in the UK Biobank reported a 17–23% lower breast cancer risk with higher levels of activity in pre- and postmenopausal women [3]. Inverse associations for pre-/perimenopausal [4] and postmenopausal women are further supported by results from Mendelian randomization studies [5].
Beyond the somewhat conflicting results by menopausal status for breast cancer overall, few studies have evaluated physical activity and breast cancer risk by hormone receptor status in premenopausal women [6]. Differing associations in pre- and postmenopausal women by tumor hormone receptor status may be evident given differences in hormone metabolism and divergent associations between adiposity and breast cancer risk by menopausal status [1, 7]. A meta-analysis including both prospective cohorts and retrospective case–control studies, evaluated 4 studies with estrogen (ER) and progesterone (PR) receptor status and premenopausal breast cancer, and observed inverse associations for both ER+/PR+ and ER−/PR− disease [6]. Analyses by ER/PR status were not included in the recent UK Biobank study [3], and in the WCRF meta-analysis [1] analyses by hormone receptor status were limited to the more common outcome of postmenopausal breast cancer (ER +/PR+ , 6 studies and 5117 cases; ER−/PR−, 5 studies 1236 cases; restricted to prospective studies).
Given the relatively sparse data on physical activity in premenopausal women by hormone receptor subtype, we provide a comprehensive evaluation of recreational physical activity, overall and of moderate-vigorous intensity, and breast cancer risk by menopausal status and hormone receptor status in 187,278 women, including 12,785 breast cancer diagnoses, from two well-characterized cohorts with up to three decades of follow-up. The results of this study provide an update of prior findings from the Nurses’ Health Study (NHS) and NHSII, with more than double the number of cases and more than a decade of further follow-up [8, 9].
Methods
Study population: the Nurses’ Health Study (NHS) and Nurses’ Health Study II (NHSII)
The NHS was initiated in 1976 when 121,700 registered nurses in the United States, ages 30–55, completed and returned a mailed questionnaire [10, 11]. The NHSII was initiated in 1989 with 116,429 female registered nurses ages 25–42 and uses the same protocols. Participants in both cohorts complete mailed biennial questionnaires and provided updated information on lifestyle factors and disease diagnoses, including cancers. The studies were approved by the institutional review boards at Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, and participating registries as required.
Breast cancer case ascertainment
Participants reported disease status on the biennial NHS and NHSII questionnaires. Eligible cases reported no prior cancer diagnosis before baseline and were diagnosed with invasive breast cancer through June 2016 (NHS) or June 2017 (NHSII). A total of 12,785 eligible breast cancer cases were identified. A study physician confirmed cases through medical record review. Invasiveness, hormone receptor status, and tumor characteristics were abstracted from medical records. Vital status was ascertained through June 1, 2016 (NHS) or June 1, 2017 (NHSII) using next of kin reports, death certificates, and the National Death Index. Given the high confirmation rate by medical record for breast cancer in this cohort (99%) [12], we included both medical record and participant-confirmed cases in this study.
Physical activity assessment
Recreational physical activity data was reported approximately every 4 years via self-administered questionnaire beginning in 1986 (NHS) and 1989 (NHSII). In the NHS, updated physical activity was reported in 1988, 1990 (walking only), 1992, 1994, 1996, 1998, 2000, 2004, 2006, 2008, 2010, 2012 and 2014 (2006, 2010: walking, jogging and running only). In the NHSII, physical activity was updated in 1991, 1997, 2001, 2005, 2009, and 2013.
Participants reported time spent (ten categories ranging from: 0 min/week to 11 + h/week), engaging in the following activities: walking or hiking outdoors; jogging (≥ 10 min/mile); running (< 10 min/mile); bicycling; calisthenics/aerobics; aerobic dance/rowing machine; tennis/squash/racquetball; lap swimming; and other aerobic recreation. Participants estimated walking pace (easy, casual (< 2 miles per hour (mph)); normal, average (2–2.9 mph); brisk (3–3.9 mph); very brisk/ striding (≥ 4 mph)). Energy expenditure was estimated by multiplying metabolic equivalent task (MET) values by reported duration for each activity [13] giving MET-h/week (e.g., 3–9 MET-h/week corresponds to approximately 1–3 h/week of walking at a pace of 2.5 mph).
Summary exposures included: total reported recreational physical activity (“total” activity in the current study refers to all recreational activities reported on the participant questionnaires) and moderate-vigorous activity (activities > 3 METs per hour: walking at pace ≥ 3 miles/hour, jogging, or running). Physical activity data was carried forward from the previous questionnaire year only in years when it was not queried (i.e., for 2002, activity reported in 2000 was used).
Covariate assessment
Data on covariates was available from the baseline and/or biennial questionnaires. Age at each questionnaire was calculated using date of birth and questionnaire return date. Age at menarche and height were collected on the baseline questionnaires. Further covariates (date of collection) included: weight at age 18 (NHS: 1980; NHSII: 1989), weight (biennially), oral contraceptive use (OC; NHS: biennially until 1982; NHSII: biennially until 2009), menopausal hormone therapy use (HT; biennially), smoking status (biennially), alcohol consumption (every four years, NHS: from 1980; NHSII: from 1991), parity (NHS: biennially until 1984; NHSII: biennially), age at first birth (NHS: 1976 and biennially until 1982; NHS: 1989 and biennially), age at menopause (biennially), diagnosis of benign breast disease (biennially), and family history of breast cancer (NHS: every 4 years beginning in 1988; NHS2: 1989, and every 4 years beginning in 1997). Body mass index (BMI) at age 18 and current BMI were calculated using self-reported weight and height (BMI = weight in kilograms (kg)/height in meters (m)2).
Statistical analysis
We calculated person-years beginning at date of baseline physical activity questionnaire return and ending at the earliest of date of diagnosis of any cancer (except non-melanoma skin cancer), death, or end of follow-up. We used multivariable Cox proportional hazards models to calculate hazard ratios (HR) using age in months as the time scale and stratified by follow-up year and cohort. Covariates were included in the models as time-varying covariates for variables with updated data throughout follow-up. Physical activity was evaluated using updated cumulative average over follow-up (i.e., average value across follow-up periods, with the average updated with each subsequent physical activity assessment). We used activity categories previously used in the cohorts (MET-h/week: < 3, 3 to < 9, 9 to < 18, 18 to < 27, ≥ 27). The reference category was < 3 MET-h/week; this level of activity corresponds to less than one hour of walking reported at “normal” or “average” pace per week. Tests for trend were evaluated by including category medians as continuous variables in the models. Covariates included in final models were: age at first birth and parity combined, birth index [14], age at menarche, BMI at age 18, menopausal status and age at menopause, oral contraceptive use, hormone therapy use, smoking, alcohol use, family history of breast cancer, and history of benign breast disease. Adjustment for current BMI was assessed in an additional model.
Associations were evaluated in strata of menopausal status and hormone receptor status. Heterogeneity (phet) in associations by hormone receptor status was assessed using a likelihood ratio test (LRT) comparing models assuming the same association between physical activity and breast cancer overall to one allowing different associations by receptor status using a competing risks model [15]. We evaluated heterogeneity in associations with overall, ER+/PR+ , and ER−/PR− disease by menopausal status (premenopausal, postmenopausal) by comparing models with and without an interaction term using the LRT. Within each menopausal group, we also evaluated heterogeneity by BMI category (< 25, ≥ 25 kg/m2). As a sensitivity analysis, we restricted analyses to women reporting a screening mammogram in the preceding two years to evaluate whether our results were impacted by differences in screening between physical activity subgroups (i.e., healthy behavior effect).
P values were considered statistically significant at < 0.05; all statistical tests are two-sided. Analyses were conducted in SAS 9.4 (Cary, NC).
Results
Baseline characteristics were generally similar across physical activity categories in both cohorts (Table 1), though women reporting higher levels of physical activity at baseline were leaner (e.g., mean BMI in NHS, ≥ 27 vs. < 3 MET-h/week: 24.4 vs. 26.2 kg/m2). Average age at baseline was 52 years for NHS participants and 34 years for NHSII participants. A total of 39% of participants in the NHS were premenopausal at first physical activity assessment and 95% were parous, whereas 97% of participants in the NHSII were premenopausal and a lower proportion parous (e.g., parous, < 3 MET-h/week: 77%; ≥ 27: 65%). Median (interquartile range) reported activity at baseline was 7.7 MET-h/week (2.7–19.0) in the NHS and 13.7 MET-h/week (5.2–30.2) in the NHSII. Average activity at the first assessment across categories and ranged from e.g., 1.4 MET-h/week for individuals reporting < 3 MET-h/week of activity to 33.7 MET-h/week for women reporting ≥ 27 MET-h/week of activity in the NHS.
Total reported recreational physical activity was inversely associated with overall breast cancer risk in pre- and postmenopausal women (premenopausal: HR = 0.91, 95%CI = (0.80–1.04); postmenopausal, 0.87 (0.80–0.94)). Recreational physical activity was inversely associated with ER+/PR+ breast cancer risk, with similar associations observed in both pre- and postmenopausal women (≥ 27 vs < 3 MET-h/week, premenopausal HR = 0.83, 95%CI = (0.70–0.99), ptrend = 0.06; postmenopausal HR = 0.86 (0.78–0.95), ptrend < 0.01; pheterogeneity = 0.97) (Table 2). The association in premenopausal women was unchanged with adjustment for current BMI (≥ 27 vs < 3 MET-h/week, 0.83 (0.69–0.98), ptrend = 0.05), while the association in postmenopausal women was attenuated after adjustment (0.95 (0.85–1.05), ptrend = 0.09). We observed limited evidence of heterogeneity in the association between moderate-vigorous activity and ER+/PR+ breast cancer risk by menopausal status (phet ≥ 0.58; e.g., ≥ 27 vs < 3 MET-h/week, premenopausal HR = 0.88 (0.69–1.11); postmenopausal HR = 0.71 (0.58–0.88)). No associations were observed for ER−/PR− breast cancer. Among women reporting a mammogram in the prior 2 years associations with total and moderate-vigorous activity were similar to the overall analyses (Table S1).
We evaluated heterogeneity in associations by BMI separately in pre- (Table 3) and postmenopausal women (Table 4). In premenopausal women, associations comparing highest to lowest activity subgroup were similar in both BMI subgroups (e.g., total activity, ER+/PR+, ≥ 27 vs. < 3 MET-h/week, BMI < 25: 0.84 (0.66–1.08) ptrend = 0.01; ≥ 25: 0.86 (0.67–1.11) ptrend = 0.99) (Table 3). Among postmenopausal women, inverse associations between total activity and ER+/PR+ breast cancer were only observed in women with BMI ≥ 25 kg/m2 (e.g., ≥ 27 vs. < 3 MET-h/week, BMI ≥ 25: 0.80 (0.69–0.92) ptrend < 0.001; < 25: 0.96 (0.80–1.15) ptrend = 0.74) (Table 4). Moderate-vigorous activity results were similar in both strata of BMI among postmenopausal women.
Discussion
Higher levels of recreational physical activity were associated with lower risk of hormone receptor-positive breast cancer in this large prospective study. These findings provide support for a role for physical activity in primary prevention of breast cancer. Inverse associations were observed regardless of menopausal status, though while associations for premenopausal disease were robust to adjustment for BMI, associations for postmenopausal disease were attenuated by BMI adjustment. This study adds to the relatively sparse literature on recreational physical activity and breast cancer in premenopausal women by hormone receptor status, observing similar inverse associations in pre- and postmenopausal women.
Prior studies have reported lower risk of breast cancer with higher levels of total recreational physical activity, with a recent meta-analysis of prospective studies noting an inverse association of similar magnitude in pre- and postmenopausal women (e.g., “high” vs. “low” recreational activity, premenopausal, relative risk (RR) = 0.89 (0.74–1.04); postmenopausal, 0.88 (0.82–0.94)) [1]. A limited number of studies with results by hormone receptor status precluded meta-analyses by hormone receptor status among premenopausal women. A lower risk of ER+/PR+ postmenopausal breast cancer was reported with higher recreational activity (n = 6 studies, 5117 cases, RR = 0.89 (0.82–0.96)), and the association ER−/PR− breast cancer was of the same magnitude (n = 5 studies, 1236 cases, 0.89 (0.76–1.04)) [1]. We observed heterogeneity when examining overall physical activity and breast cancer risk by hormone receptor status only among postmenopausal women; however, in both pre- and postmenopausal women, associations were only observed for ER+/PR+ disease. Heterogeneity by hormone receptor status has largely not been observed in prior studies of physical activity and breast cancer risk [8, 16,17,18,19,20], though associations are more consistently observed for hormone responsive disease. The current study includes more postmenopausal ER+/PR+ cases (n = 5598) than the prior published meta-analysis [1], and a substantial number of ER−/PR− cases (n = 1106), and adds needed data on physical activity and breast cancer in premenopausal women (n = 1729 ER+/PR+, n = 372 ER−/PR−).
Findings from prior studies have suggested vigorous activity may have differential effects on breast cancer risk by menopausal status, with a prior meta-analysis of prospective studies [1] reporting a suggestively stronger inverse association for vigorous activity among premenopausal women, (“high” vs. “low”, premenopausal, 0.79 (0.74–1.04); postmenopausal, 0.90 (0.85–0.95)). A separate meta-analysis [6] on moderate-vigorous activity including both retrospective and prospective studies observed lower risk of ER+/PR+ and ER−/PR− in premenopausal women, as compared to postmenopausal women (e.g., ER+/PR+: premenopausal, 4 studies, RR = 0.60 (0.45–0.81); postmenopausal, 13 studies, 0.79 (0.71–0.89)). We did not observe this pattern for moderate-vigorous activity in the current study, with a somewhat stronger association observed in postmenopausal women (ER+/PR+, ≥ 27 vs. < 3 MET-h/week, 0.71 (0.58–0.88)) and an inverse association observed in premenopausal women (0.88 (0.69–1.11)); associations in the current study were similar when considering all cases (i.e., regardless of ER/PR status).
We observed limited heterogeneity in associations by BMI in the current study, although the inverse association between total recreational activity and risk in the current study was predominantly observed in postmenopausal women with BMI ≥ 25 kg/m2. This is in contrast to a meta-analysis evaluating total activity, which reported a stronger association among postmenopausal normal-weight women [1]. A recent study in the UK Biobank [3] observed no heterogeneity in associations by BMI, with similar associations in strata of BMI and an inverse association among (pre- and postmenopausal) women with BMI ≥ 25 kg/m2. We observed that the associations between moderate-vigorous activity and breast cancer risk were similar in both strata of BMI. This is consistent with a meta-analysis on moderate-vigorous activity which reported similar associations in strata of BMI [6], though this was only observed for postmenopausal women.
Physical activity may influence breast cancer risk through its impact on adiposity, and adiposity-related mechanisms including sex steroid hormone metabolism, and inflammation and immune-related pathways. The associations between adiposity [21, 22] and physical activity [23, 24] and these mechanisms have been described previously with lower levels of adiposity and higher levels of physical activity, for example, associated with lower circulating estradiol, improvements in insulin resistance, and lower concentrations of inflammation marker C-reactive protein, and altered immune response.
We adjusted for current BMI in secondary models given that BMI may be on the causal pathway. BMI adjustment had essentially no impact on the association between physical activity and breast cancer in premenopausal women, but attenuated associations for ER+/PR+ postmenopausal disease (e.g., total activity unadjusted HR, 0.86 (0.78–0.95); adjusted, 0.95 (0.85–1.05)). The associations for postmenopausal breast cancer are in line with the well-established positive association between BMI and postmenopausal breast cancer [1]. In a recent study in the UK Biobank, accelerometer-based physical activity was evaluated, and analyses were adjusted for fat mass measured with bioimpedance [3]. Small changes in the associations between physical activity and breast cancer risk were noted after adjustment for body fatness, in the direction of strengthening associations in premenopausal women (RR per 5 milligravity units of activity, before adjustment, 0.82 (0.69–0.97); after adjustment, 0.79 (0.66–0.95)) and attenuating associations after adjustment in postmenopausal women (before adjustment, 0.79 (0.69–0.90); after adjustment, 0.84 (0.73–0.96)). Notably, BMI is associated with a lower risk of breast cancer in premenopausal women [7], likely explaining why this adjustment did not impact findings for physical activity and pre-menopausal breast cancer. It is plausible that the associations between physical activity and premenopausal breast cancer are underpinned by direct effects of physical activity on intermediate mechanistic pathways, and that associations are independent of adiposity.
Our study has strengths and limitations. The biennial follow-up enabled us to update physical activity and covariate data throughout the study period, and we used a cumulative average measure to represent habitual physical activity across follow-up. A limitation of using the cumulative average physical activity measure, together with time-varying covariates, is the potential conditioning on mediating variables across follow-up (i.e., those variables impacted by past activity as reflected in the cumulative average). Results from age-adjusted models were similar to those from the multivariable models, though with less precise confidence intervals, thus we do not expect this has had a substantial impact on our results. The BMI-adjusted models would be expected to be the most substantially impacted by this issue, and this may have led to an attenuation of the effect of adjustment for BMI. A limitation of the study is the use of self-reported activity, however, this approach has demonstrated reliability and validity [25] and has been associated with other outcomes [26,27,28,29]. The levels of recreational activity reported in the NHS and NHSII are similar to those reported in other prospective cohorts [30]. Further, our results describe associations with recreational, discretionary activity and not occupational or household and caregiving physical activity. Recreational activity may represent activity types that are most amenable to change, and thus with potential for intervention toward cancer prevention. However, lack of data on other activity types precludes an evaluation of total physical activity across domains. The results of this updated study within the NHS and NHSII are in line with earlier findings from these cohorts with shorter follow-up [8, 9]. Finally, while this study adds needed information on physical activity and breast cancer risk in premenopausal women by tumor hormone receptor status, sample size precluded an evaluation of more detailed tumor subtypes.
Higher levels of recreational physical activity were associated with lower risk of both pre- and postmenopausal hormone receptor-positive breast cancer, providing further support for the beneficial role of physical activity for cancer prevention. These results were robust to adjustment for current BMI in premenopausal women, whereas BMI adjustment attenuated the results in postmenopausal women, findings that are consistent with the established associations between adiposity-related mechanisms and postmenopausal breast cancer. These findings support recreational physical activity as a modifiable exposure associated with reduced breast cancer risk regardless of menopausal status.
Data availability
Data used in this study are available by application at nurseshealthstudy.org.
References
Chan DSM, Abar L, Cariolou M, Nanu N, Greenwood DC, Bandera EV, McTiernan A, Norat T (2019) World Cancer Research Fund International: Continuous Update Project-systematic literature review and meta-analysis of observational cohort studies on physical activity, sedentary behavior, adiposity, and weight change and breast cancer risk. Cancer Causes Control CCC 30(11):1183–1200. https://doi.org/10.1007/s10552-019-01223-w
World Cancer Research Fund American Institute for Cancer Research: Food, Nutrition, Physical Activity, and Breast Cancer In: Continuous Update Project Expert Report 2018 (2018)
Guo W, Fensom GK, Reeves GK, Key TJ (2020) Physical activity and breast cancer risk: results from the UK Biobank prospective cohort. Br J Cancer 122(5):726–732. https://doi.org/10.1038/s41416-019-0700-6
Dixon-Suen SC, Lewis SJ, Martin RM, English DR, Boyle T et al (2022) Physical activity, sedentary time and breast cancer risk: a Mendelian randomisation study. Br J Sports Med 56(20):1157–1170. https://doi.org/10.1136/bjsports-2021-105132
Papadimitriou N, Dimou N, Tsilidis KK, Banbury B, Martin RM et al (2020) Physical activity and risks of breast and colorectal cancer: a Mendelian randomisation analysis. Nat Commun 11(1):597. https://doi.org/10.1038/s41467-020-14389-8
Neilson HK, Farris MS, Stone CR, Vaska MM, Brenner DR, Friedenreich CM (2017) Moderate-vigorous recreational physical activity and breast cancer risk, stratified by menopause status: a systematic review and meta-analysis. Menopause 24(3):322–344. https://doi.org/10.1097/GME.0000000000000745
Premenopausal Breast Cancer Collaborative G, Schoemaker MJ, Nichols HB, Wright LB, Brook MN et al (2018) Association of body mass index and age with subsequent breast cancer risk in premenopausal women. JAMA Oncol 4(11):81771. https://doi.org/10.1001/jamaoncol.2018.1771
Eliassen AH, Hankinson SE, Rosner B, Holmes MD, Willett WC (2010) Physical activity and risk of breast cancer among postmenopausal women. Arch Intern Med 170(19):1758–1764. https://doi.org/10.1001/archinternmed.2010.363
Maruti SS, Willett WC, Feskanich D, Rosner B, Colditz GA (2008) A prospective study of age-specific physical activity and premenopausal breast cancer. J Natl Cancer Inst 100(10):728–737. https://doi.org/10.1093/jnci/djn135
Colditz GA, Hankinson SE (2005) The Nurses’ Health Study: lifestyle and health among women. Nat Rev Cancer 5(5):388–396. https://doi.org/10.1038/nrc1608
Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, Chavarro JE (2016) Origin, methods, and evolution of the three nurses’ health studies. Am J Public Health 106(9):1573–1581. https://doi.org/10.2105/AJPH.2016.303338
Fortner RT, Sisti J, Chai B, Collins LC, Rosner B, Hankinson SE, Tamimi RM, Eliassen AH (2019) Parity, breastfeeding, and breast cancer risk by hormone receptor status and molecular phenotype: results from the Nurses’ Health Studies. Breast Cancer Res 21(1):40. https://doi.org/10.1186/s13058-019-1119-y
Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, Paffenbarger RS Jr (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25(1):71–80. https://doi.org/10.1249/00005768-199301000-00011
Rosner B, Colditz GA (1996) Nurses’ health study: log-incidence mathematical model of breast cancer incidence. J Natl Cancer Inst 88(6):359–364. https://doi.org/10.1093/jnci/88.6.359
Wang M, Spiegelman D, Kuchiba A, Lochhead P, Kim S et al (2016) Statistical methods for studying disease subtype heterogeneity. Stat Med 35(5):782–800. https://doi.org/10.1002/sim.6793
Steindorf K, Ritte R, Eomois PP, Lukanova A, Tjonneland A et al (2013) Physical activity and risk of breast cancer overall and by hormone receptor status: the European prospective investigation into cancer and nutrition. Int J Cancer 132(7):1667–1678. https://doi.org/10.1002/ijc.27778
Hildebrand JS, Gapstur SM, Campbell PT, Gaudet MM, Patel AV (2013) Recreational physical activity and leisure-time sitting in relation to postmenopausal breast cancer risk. Cancer Epidemiol Biomark Prev 22(10):1906–1912. https://doi.org/10.1158/1055-9965.EPI-13-0407
Dallal CM, Sullivan-Halley J, Ross RK, Wang Y, Deapen D et al (2007) Long-term recreational physical activity and risk of invasive and in situ breast cancer: the California teachers study. Arch Intern Med 167(4):408–415. https://doi.org/10.1001/archinte.167.4.408
Peters TM, Schatzkin A, Gierach GL, Moore SC, Lacey JV Jr, Wareham NJ, Ekelund U, Hollenbeck AR, Leitzmann MF (2009) Physical activity and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Cancer Epidemiol Biomark Prev 18(1):289–296. https://doi.org/10.1158/1055-9965.EPI-08-0768
Fournier A, Dos Santos G, Guillas G, Bertsch J, Duclos M, Boutron-Ruault MC, Clavel-Chapelon F, Mesrine S (2014) Recent recreational physical activity and breast cancer risk in postmenopausal women in the E3N cohort. Cancer Epidemiol Biomark Prev 23(9):1893–1902. https://doi.org/10.1158/1055-9965.EPI-14-0150
Renehan AG, Zwahlen M, Egger M (2015) Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer 15(8):484–498. https://doi.org/10.1038/nrc3967
de Heredia FP, Gomez-Martinez S, Marcos A (2012) Obesity, inflammation and the immune system. Proc Nutr Soc 71(2):332–338. https://doi.org/10.1017/S0029665112000092
Friedenreich CM, Neilson HK, Farris MS, Courneya KS (2016) Physical activity and cancer outcomes: a precision medicine approach. Clin Cancer Res 22(19):4766–4775. https://doi.org/10.1158/1078-0432.CCR-16-0067
Neilson HK (2009) FRIEDENREICH CM, Brockton NT, Millikan RC: Physical activity and postmenopausal breast cancer: proposed biologic mechanisms and areas for future research. Cancer Epidemiol Biomark Prev 18(1):11–27. https://doi.org/10.1158/1055-9965.EPI-08-0756
Al-Shaar L, Pernar CH, Chomistek AK, Rimm EB, Rood J, Stampfer MJ, Eliassen AH, Barnett JB, Willett WC (2022) Reproducibility, validity, and relative validity of self-report methods for assessing physical activity in epidemiologic studies: findings from the women’s lifestyle validation study. Am J Epidemiol 191(4):696–710. https://doi.org/10.1093/aje/kwab294
Hu FB, Sigal RJ, Rich-Edwards JW, Colditz GA, Solomon CG, Willett WC, Speizer FE, Manson JE (1999) Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. JAMA 282(15):1433–1439. https://doi.org/10.1001/jama.282.15.1433
Chomistek AK, Chiuve SE, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB (2015) Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol 65(1):43–51. https://doi.org/10.1016/j.jacc.2014.10.024
Martinez ME, Giovannucci E, Spiegelman D, Hunter DJ, Willett WC, Colditz GA (1997) Leisure-time physical activity, body size, and colon cancer in women. Nurses’ Health Study Research Group. J Natl Cancer Inst 89(13):948–955. https://doi.org/10.1093/jnci/89.13.948
Hu FB, Stampfer MJ, Colditz GA, Ascherio A, Rexrode KM, Willett WC, Manson JE (2000) Physical activity and risk of stroke in women. JAMA 283(22):2961–2967. https://doi.org/10.1001/jama.283.22.2961
Matthews CE, Moore SC, Arem H, Cook MB, Trabert B et al (2020) Amount and intensity of leisure-time physical activity and lower cancer risk. J Clin Oncol 38(7):686–697. https://doi.org/10.1200/JCO.19.02407
Acknowledgements
We would like to thank the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. The authors assume full responsibility for analyses and interpretation of these data.
Funding
Open access funding provided by Norwegian Institute of Public Health (FHI). This project was supported by the National Institutes of Health (R01 CA50385, U01 CA176726, UM1 CA186107, P01 CA87969) and the Breast Cancer Research Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding sources had no role in the design, analysis, and reporting of the study.
National Institutes of Health,R01 CA50385,A. Heather Eliassen,U01 CA176726,A. Heather Eliassen,UM1 CA186107,A. Heather Eliassen,P01 CA87969,A. Heather Eliassen
Author information
Authors and Affiliations
Contributions
RTF, AHE, RMT, WCW, and MDH are responsible for the conception and design. KDB conducted the statistical analyses. All authors contributed to the study interpretation. AHE, RMT, and WCW obtained funding for data acquisition. RTF wrote the first draft. All authors contributed to the review and revision of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the Institutional Review Board of the Brigham and Women’s Hospital (Boston, MA).
Consent to participate
Participants provided informed consent.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fortner, R.T., Brantley, K.D., Tworoger, S.S. et al. Recreational physical activity and breast cancer risk by menopausal status and tumor hormone receptor status: results from the Nurses’ Health Studies. Breast Cancer Res Treat 206, 77–90 (2024). https://doi.org/10.1007/s10549-023-07238-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07238-x