Abstract
Purpose
In this study of oestrogen receptor (ER) Low Positive breast cancers (BC) in three large cohorts of BC patients, we assess associations between levels of ER expression and tumour characteristics and prognosis.
Methods
Cases were stratified into patients unlikely to have received adjuvant therapy according to treatment guidelines at time of diagnosis (before 1995), and those who could have received adjuvant therapy (diagnosed in 1995 or later). ER status was divided into < 1%; ≥ 1 < 10%; ≥ 10%. Results were correlated with time of diagnosis, histopathological grade, proliferation status, and molecular subtypes, using Pearson’s Chi-square test. For prognosis, hazard ratios and cumulative incidence of death from BC were used.
Results
Of the 1955 tumours, 65 (3.3%) were ER Low Positive (ER ≥ 1 < 10%). Overall, the highest proportion of ER Low Positive tumours was observed among Luminal B (HER2 +) subtype (9.4%) and grade 3 tumours (4.3%). The risk of death from BC was lower in ER Low Positive and ER ≥ 10% compared to ER-negative cases. Compared to patients diagnosed before 1995, women diagnosed in 1995 or later showed a higher proportion of ER Low Positive BCs, and their tumours were of smaller size, lower grade, and lower proliferative status. There was no significant difference in prognosis compared to those with ER ≥ 10% tumours.
Conclusion
Women with ER Low Positive tumours diagnosed in a time period when adjuvant therapy was available had tumours of smaller size, lower grade, and lower proliferative status, and similar prognosis to those with ER ≥ 10% compared to women diagnosed earlier.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oestrogen receptor (ER) status plays an essential role in clinical decision-making and predicting outcome and treatment response for breast cancer (BC) patients [1]. According to current guidelines [2], patients with ER-positive tumours are considered eligible for endocrine therapy. Patients with ER-negative tumours are more likely to benefit from chemotherapy and generally have a poorer outcome than patients with ER-positive (ER +) tumours [3, 4].
Breast cancer differs from most tumours because of its dependence on female sex hormones for development and growth [5]. Expression of ER by immunohistochemistry (IHC) is seen in more than 70% of BC tumours [6]. The ASCO/CAP and current national BC guidelines state that BC tumours with ≥ 1% positive staining tumour cell nuclei should be interpreted as ER + , and negative if < 1% of tumour cell nuclei express ER [2, 7]. However, the ASCO/CAP Expert Panel states that data on the effect of endocrine therapy for cancers with ER ≥ 1 < 10% are limited. They suggest that samples with ER ≥ 1 < 10% should be reported as ER Low Positive, with a comment mentioning the limited data available on the therapeutic benefit of anti-hormonal treatment for this group of patients [2]. According to the St. Gallen 2019 Consensus Discussion on The Optimal Primary Breast Cancer Treatment, there is a need for better evaluation of ideal cut-off levels for the prescription of endocrine therapy for ER + tumours, particularly for ER Low Positive cases [8,9,10].
In this study we examined expression levels of ER in BC tumours and associations between ER status and time of diagnosis, and tumour characteristics such as histopathological grade, molecular subtypes, proliferation and prognosis, with emphasis on ER Low Positive tumours.
Materials and methods
Study population
This study comprises women from three population-based surveys conducted in Trøndelag County, Norway. Information on breast cancer incidence was obtained from the Cancer Registry of Norway. Date of death, and/or emigration was obtained from the National Population Register and causes of death from the Norwegian Cause of Death Registry. Formalin-fixed, paraffin embedded (FFPE) tumour tissue from the primary tumours and corresponding pathology reports were retrieved from the Department of Pathology at St. Olav’s Hospital, Trondheim University Hospital, Norway (Fig. 1).
Cohort 1: The cohort includes 25,727 women born 1886–1928 [11] invited to attend a population-based survey for the early detection of breast cancer conducted in Nord-Trøndelag County, Norway, between 1956 and 1959. During 47 years of follow-up (1961 to end of 2008), 1379 new BCs were registered among these women. In a previous study 909 of these tumours were classified according to histopathological type and grade and divided into molecular subtypes [12]. For one case ER status was missing, and this case was excluded from the present study, leaving 908 cases. After diagnosis, patients were followed until time of death from BC or death from other causes, or until December 31st, 2015.
Cohort 2: The second cohort comprises 34,221 women born between 1897 and 1977 and derives from the HUNT2 Study conducted between 1995 and 1997 in Nord-Trøndelag County, Norway [13]. From attendance until December 31st, 2009, 728 women were diagnosed with BC. Of these, 157 cases were already included in Cohort 1 and 57 were unavailable for subtyping. The remaining tumours (n = 514) from Cohort 2 were assigned histopathological type and grade and reclassified into molecular subtypes [14]. ER status was available for all 514 cases. After diagnosis, these patients were followed until time of death from BC or death from other causes, or until December 31st, 2015.
Cohort 3: The third cohort includes 22,931 women born at E.C. Dahl’s Foundation, Trondheim, Norway between 1920 and 1966. During 52 years of follow-up (1961 to the end of 2012), a total of 870 women were diagnosed with BC. Among them, 598 were diagnosed at St Olav’s Hospital, and histopathological typing, grading and molecular subtyping were successful for 537 of these cases [15]. ER status was available for 533 of these cases. After diagnosis, patients were followed until time of death from BC or death from other causes, or until December 31st, 2015.
Specimen characteristics
Tissue Microarray (TMA) paraffin blocks were made from the archival tumour tissue using the TissueArrayer Minicore with TMA Designer2 software (Alphelys). Three 1 mm in diameter tissue cylinders from the periphery of the FFPE primary tumours were transferred to TMA recipient blocks. TMA Sections (4 µm) were cut and IHC-staining for ER was carried out within four weeks after sectioning. Between cutting and staining, sections were stored at − 20 °C. Staining intensity was not quantified in this study. Molecular subtypes for all cases in all three cohorts were determined using IHC and in situ hybridization in lieu of gene expression analyses, and have been published previously [12, 14, 15]. The IHC markers including ER are shown in Table 1.
Statistical analyses
For the present study, we divided ER expression into three categories (< 1%; ≥ 1 < 10%; ≥ 10%) and studied associations between ER expression and histopathological grade, molecular subtype, proliferation, and prognosis.
Pearson’s chi square test was used to compare patient and tumour characteristics across categories of ER. In analyses of prognosis, we distinguished between women diagnosed before 1995 and women diagnosed in 1995 or later. This cut-off was used to approximate the gradual implementation of adjuvant treatment in Norway [14, 16]. Cumulative incidence of death from BC was estimated, with death from other causes as competing events. Gray’s test was used to compare equality between cumulative incidence curves. Cox proportional hazard analyses were used to estimate hazard ratios (HR) of BC death with 95% confidence intervals (CI) within each diagnostic period, censoring at time of death from other causes. We adjusted for age, stage, histopathological grade, and for these variables combined. No clear violations of proportionality were found in log-minus-log plots. Statistical analyses were performed using Stata/MP version 17 (StataCorp LP, College Station, Texas, USA).
Results
Patient and tumour characteristics for the 1955 patients included in the present study are shown in Table 2. Mean age at diagnosis was 67.3 years (SD: 12.8) and mean follow-up after diagnosis was 9.9 years (SD: 7.3). By end of follow-up, 545 (27.9%) patients had died from BC and 588 (30.1%) died from other causes. Of the 1955 tumours, 315 (16.1%) were ER < 1%, 65 (3.3%) were ER Low Positive (ER ≥ 1 < 10%) and 1575 (80.6%) were ER ≥ 10%. Of the 545 deaths from BC, 129 (23.7%) cases were ER < 1%, 16 (2.9%) were ER Low Positive and 400 (73.4%) were ER ≥ 10%.
ER categories and molecular subtypes
Of the 1955 tumours included in this study, 1669 (85.4%) were classified as one of the luminal subtypes (Luminal A, Luminal B (HER2-), or Luminal B (HER2 +)). Of these, 1640 were ER positive (ER ≥ 1%). Of the 180 cases of Luminal B (HER2 +), seven (3.9%) cases were ER < 1%, 17 (9.4%) were ER Low Positive and 156 (86.7%) were ER ≥ 10% (p < 0.0001). Among the 937 cases with Luminal A subtype, 10 (1.1%) cases were ER < 1%, 29 (3.1%) were ER Low Positive and 898 (95.8%) were ER ≥ 10%. Of the 552 Luminal B (HER2-) cases 12 (2.2%) cases were ER < 1%, 19 (3.4%) were ER Low Positive and 521 (94.4%) were ER ≥ 10%. Twenty-six cases with ER < 1% were classified as Luminal based on progesterone receptor (PR) positivity (Table 2).
ER categories, histopathological grade, proliferation, and histopathological type
In this study, 287 (14.7%) tumours were grade 1, 1015 (51.9%) were grade 2 and 653 (33.4%) were grade 3. The highest proportion of ER Low Positive (28/653 (4.3%)) was observed among grade 3 tumours (p < 0.0001). Of the 1057 cases with Ki-67 < 15%, 74 (7.0%) were ER < 1%, 31 (2.9%) were ER Low Positive, and 952 (90.1%) were ER ≥ 10%. Of the 898 cases with Ki-67 ≥ 15%, 241 (26.8%) were ER < 1%, 34 (3.8%) were ER Low Positive, and 623 (69.4%) were ER ≥ 10% (p < 0.0001). Similarly, of the 459 cases with ≤ 2 mitoses/10 High power fields (HPF) (p25), 23 (5.0%) were ER < 1%, 9 (2.0%) were ER Low Positive and 427 (93.0%) were ER ≥ 10% (p < 0.0001). Whereas, of the 875 cases with > 13 mitoses/10 HPF (p75), 215 (24.6%) were ER < 1%, 40 (4.5%) were ER Low Positive, and 620 (70.9%) were ER ≥ 10% (p < 0.0001). Of the 65 ER Low Positive cases, 50/1507 (3.3%) were invasive carcinoma NOS, 8/210 (3.8%) were lobular carcinoma, 4/60 (6.6%) were medullary carcinoma, and 1/18 (5.5%) was metaplastic carcinoma (Table2).
Comparisons between women diagnosed before 1995 and women diagnosed in 1995 or later
A total of 774 cases were diagnosed before 1995, and 1181 were diagnosed in 1995 or later. The distribution of cases according to time of diagnosis are shown in Table 3. Of women diagnosed before 1995, 352/774 (45.5%) died from BC during follow-up, as opposed to 193/1181 (16.3%) of those diagnosed in 1995 or later. Among women diagnosed before 1995, 152/774 (19.6%) tumours were ER < 1%, falling to 163/1181 (13.8%) among women diagnosed in 1995 or later. Similarly, 16/774 (2.1%) tumours were ER Low Positive before 1995, rising to 49/1181 (4.2%) in 1995 or later, and 606/774 (78.3%) cases diagnosed before 1995 were ER ≥ 10%, rising to 969/1181 (82.1%) among women diagnosed in 1995 or later. Furthermore, we found that 310/774 (40.1%) of tumours diagnosed before 1995 were ≤ 2 cm in diameter, rising to 725/1181 (61.4%) for tumours diagnosed in 1995 or later (p < 0.0001) (Table 3).
Characteristics of ER low positive tumours
The distribution of tumour characteristics in patients with ER Low tumours are shown in Table 4. There was a total of 65 (3.3%) ER Low Positive tumours in this study. Of these, 16 were diagnosed before 1995, and 49 was diagnosed in 1995 or later. Among the ER Low Positive tumours diagnosed before 1995, 8/16 (50%) died from BC during follow-up, as opposed to 8/49 (16.3%) of those diagnosed in 1995 or later. Among ER Low tumours, the proportion of tumours < 2 cm, rose from 31% in patients diagnosed before 1995 to 57% in those diagnosed in 1995 or later (p < 0.0001).
For all cases, there was a higher proportion of grade 1 tumours (17.2%), and a lower proportion of tumours with grade 3 (29.6%) among women diagnosed in 1995 or later, compared to women diagnosed before 1995 (Grade 1: 10.9%, Grade 3: 39.1% (p < 0.0001)). Among ER Low Positive cases, there was a higher proportion of grade 1 (12.2%) and 2 (53.1%) tumours among women diagnosed in 1995 or later, compared to the women diagnosed before 1995 (grade 1: 0%, grade 2: 31.2%). For grade 3 tumours the proportion of ER low tumours was lower when diagnosed in 1995 or later (p = 0.04) (Table 4).
For all cases, the proportion of Luminal A subtype was higher for women diagnosed in 1995 or later (52.5%) compared to those diagnosed before 1995 (41.0%). The proportion of Luminal B (HER2-) and HER2 subtypes was lower for women diagnosed in 1995 or later (p < 0.0001) (Table 3), compared to those diagnosed before 1995. Among ER Low Positive tumours, the proportion of Luminal A subtype rose from 25% in ER Low tumours diagnosed before 1995, to 51% when diagnosed in 1995 or later. The proportion of Luminal B (HER2 +) tumours was lower among the women diagnosed in 1995 or later (18.4%), than the women diagnosed before 1995 (50%) (p = 0.037) (Table 4).
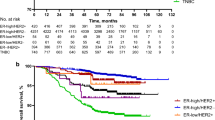
ER categories and prognosis
Cumulative incidence of death by BC according to ER status is shown in Fig. 2. The risk of death from BC for all categories of ER expression was lower for women diagnosed in 1995 or later compared to women diagnosed before 1995 (Table 5). The cumulative risk of death from BC after 5 years, for women diagnosed before 1995, was 47.4% among cases with ER < 1%, 37.5% for cases with ER Low Positive and 20.8% for cases with ER ≥ 10%. Among women diagnosed with breast cancer in 1995 or later the cumulative risk of death from BC was 22.3% after 5 years for ER < 1%, and 8.3% for both the ER Low Positive and ER ≥ 10% group (Table 5). Thus, among patients diagnosed in 1995 or later, there was no clear difference in risk of death from BC between cases with ER Low Positive and ER > 10%.
Cox regression analyses showed that the risk of death was lower among patients with ER ≥ 10%, compared to those with ER < 1%, both among patients diagnosed before 1995, and among patients diagnosed in 1995 or later. The Cox analysis shows a lower relative risk of death from BC among patients with ER ≥ 10% tumours, compared to ER < 1% both before and after 1995. We observed a tendency towards a lower relative risk of death from BC among ER Low Positive, compared to ER < 1%. However, these findings were not statistically significant (Table 5).
Discussion
In this study of 1955 primary BC tumours, we found that 65 (3.3%) tumours fell under the ER Low Positive category. We found the highest proportion of ER Low Positive among Luminal B (HER2 +) tumours (9.4%). Among cases diagnosed before 1995, 2.1% were ER Low Positive rising to 4.2% among cases diagnosed in 1995 or later. We found an association between ER Low Positive and high histopathological grade, high Ki-67 levels and high mitotic count. However, the results did not show a significant association with prognosis.
Breast cancer survival in Norway has increased since the mid-1990s as seen in the present and other studies [17]. This may be ascribed to earlier detection [18, 19] and improved treatment [6, 20]. The reduced risk of death observed between the two time-periods for all categories of ER expression, probably reflects earlier diagnosis with the introduction of mammography screening and the introduction of adjuvant treatment therapies in the mid-1990s. The change in prognosis observed across time for patients with ER Low Positive tumours may also be attributed to adjuvant therapy other than antihormonal treatment in addition to changing tumour characteristics such as smaller tumour size and lower histopathological grade. However, a drawback of the present study was lack of availability of disease-free survival data.
ER status is an important indicator of prognosis and a predictor of the effect of endocrine treatment. ER signalling is a main driver of proliferation in ER Positive BCs, and inhibition of ER signalling has improved survival among ER Positive BC patients [6, 21]. Studies suggest that selection of patients for endocrine therapy may need to be further personalized [9, 22, 23]. While most ER + BCs have high IHC scores, about 2–3% of cases are ER Low Positive [10, 24, 25]. In the present study, 3.3% of the total number of cases were ER Low Positive. While these tumours are classified within the ER + category, their risk profile appears to be more like that of ER-negative breast cancers [24]. A recent study found no benefit of endocrine therapy in the ER < 10% group compared to the ER > 10% group [25]. The lack of benefit of endocrine therapy in patients with low ER expression has recently been shown in a meta-analysis, including more than 16,000 patients [26]. The meta-analysis indicated that primary BC patients with ER 1–9% gained no significant survival benefit from endocrine therapy, but manifested better overall prognosis than patients with cancers expressing ER < 1% [26]. In the present study, among patients diagnosed in 1995 or later, the ER Low Positive patient group had similar survival to those with ER ≥ 10%. The patients included in this study were diagnosed with BC between 1961 and 2012, and the ER > 1% cut-off level for endocrine treatment was first introduced in Norway in 2011 after recommendations from ASCO/CAP [27]. Therefore, the improved prognosis seen among ER Low Positive patients diagnosed in 1995 or later, can most likely not be attributed to endocrine treatment [28]. Among women diagnosed in 1995 or later, we found a greater proportion of ER Low Positive tumours with smaller size, lower grade, and lower proliferation compared to ER Low Positive tumours diagnosed before 1995. Thus, the improved prognosis may be attributed to factors other than endocrine treatment, such as earlier diagnosis due to the introduction of mammography screening and greater BC awareness among women. Determining endocrine treatment for patients with a diagnosis of ER Low Positive BC should be carefully considered in light of the potential risks and benefits of the treatment [24].
In the present study, the proportion of Luminal A tumours was higher among women diagnosed in the time period during which adjuvant treatment and earlier diagnosis became available, a finding previously observed by our group in an analysis of cohorts 1 and 2 [14]. It has been suggested that BC patients with ER Low Positive are more similar to the ER-negative group, and therefore may not profit from endocrine therapy [9]. Thus, it has been suggested that cut-off levels should be further investigated in order to offer BC patients personalized endocrine treatment [22, 29, 30]. In the present study we found that among cases diagnosed in 1995 or later, ER Low Positive cases showed a prognosis similar to that of ER ≥ 10% cases. However, the impact of hormonal therapy could not be assessed in this study, due to lack of individual information on treatment.
Similar to our findings, a recent study showed that ER Low Positive tumours were more frequently grade 3 and had a higher expression of Ki-67, compared to BCs with intermediate or high expression of ER [31]. Furthermore, they found that the expression of immune-related biomarkers in ER Low Positive was similar to that of ER-negative tumours. We observed four cases of medullary carcinoma and one metaplastic carcinoma among the ER Low Positive cases. When determining treatment for patients with ER Low Positive BC, it may be useful to consider including a panel of immune-related biomarkers.
The FFPE tumour tissue included in this study covered a diagnostic timespan of several decades, and preanalytical conditions may have varied over time. Many of the tumours were diagnosed at a time when ER IHC was not done in the diagnostic setting. However, valuable information can be drawn from archival tissue blocks [32, 33]. It has been shown that antigenicity is, for the most part, preserved in paraffin blocks over decades but may decrease in sections stored over time, resulting in weaker staining [33,34,35]. We observed no apparent trend towards a negative result among the older specimens but felt it would be unwise to attempt to quantify staining intensity due to the varying preanalytical conditions over which we had no control.
Other strengths of this study include reliable information on BC incidence and follow-up data that were available from high-quality national registries like the Cancer Registry of Norway, the Cause of Death Registry and the Norwegian Patient register [36, 37] thus enabling comparability within the study population across time.
Using TMA sections enables us to stain hundreds of tumour samples at the same time, under the same conditions. The samples comprise a small amount of the original tumour tissue samples, compared to full-face sections. Thus, some important information from the tumour may be lost. However, it has been shown that IHC for ER carried out on sections from TMAs can provide equivalent information regarding clinical endpoint when compared to IHC on full-face tissue Sections [38, 39]. Immunohistochemistry for ER on full-face tissue sections was not carried out in the present study.
Conclusion
Overall, ER Low Positive BCs exhibited many characteristics similar to ER-negative tumours and were frequently Luminal B (HER2 +). Among women diagnosed in 1995 or later, the proportion of ER Low Positive BCs was higher than among women diagnosed before 1995 and ER Low Positive tumours diagnosed in 1995 or later were of smaller size, lower grade, lower proliferative status, and were more frequently Luminal A Women with ER Low Positive tumours had similar prognosis to patients with ER ≥ 10% when diagnosed in 1995 or later.
Data availability
The datasets generated and/or analysed during this study are not publicly available due to issues of sensitivity and limitations determined in the conditions for approval by the Regional Committee for Medical and Health Research Ethics. However, the data may be made available from the corresponding author on reasonable request.
References
Regan MM, Viale G, Mastropasqua MG, Maiorano E, Golouh R, Carbone A et al (2006) Re-evaluating adjuvant breast cancer trials: assessing hormone receptor status by immunohistochemical versus extraction assays. J Natl Cancer Inst 98(21):1571–1581
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL et al (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38(12):1346–1366
Lippman ME, Allegra JC, Thompson EB, Simon R, Barlock A, Green L et al (1978) The relation between estrogen receptors and response rate to cytotoxic chemotherapy in metastatic breast cancer. N Engl J Med 298(22):1223–1228
Barrios CH, Sampaio C, Vinholes J, Caponero R (2009) What is the role of chemotherapy in estrogen receptor-positive, advanced breast cancer? Ann Oncol 20(7):1157–1162
Clemons M, Goss P (2001) Estrogen and the risk of breast cancer. N Engl J Med 344(4):276–285
Early Breast Cancecr Trialists’ Collaborative G, Davies C, Godwin J, Gray R, Clarke M, Cutter D et al (2011) Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet 378(9793):771–784
Helsedirektoratet NBCGN (2020) Nasjonalt handlingsprogram med retningslinjer for diagnostikk, behandling og oppfølging av pasienter med brystkreft https://www.helsedirektoratet.no/retningslinjer/brystkreft-handlingsprogram: Helsedirektoratet, avdeling spesialisthelsetjenester; [updated 08/2020. IS-2945]. https://www.helsedirektoratet.no/retningslinjer/brystkreft-handlingsprogram.
Balic M, Thomssen C, Würstlein R, Gnant M, Harbeck N (2019) St Gallen/Vienna 2019: a brief summary of the consensus discussion on the optimal primary breast cancer treatment. Breast Care 14(2):103–110
Yu KD, Cai YW, Wu SY, Shui RH, Shao ZM (2021) Estrogen receptor-low breast cancer: biology chaos and treatment paradox. Cancer Commun (Lond) 41(10):968–980
Fei F, Siegal GP, Wei S (2021) Characterization of estrogen receptor-low-positive breast cancer. Breast Cancer Res Treat 188(1):225–235
Kvâle G, Heuch I, Eide GE (1987) A prospective study of reproductive factors and breast cancer: I—parity. Am J Epidemiol 126(5):831–841
Engstrom MJ, Opdahl S, Hagen AI, Romundstad PR, Akslen LA, Haugen OA et al (2013) Molecular subtypes, histopathological grade and survival in a historic cohort of breast cancer patients. Breast Cancer Res Treat 140(3):463–473
Holmen J (2011) The Nord-Trøndelag health study 1995–97 (HUNT 2). Norsk Epidemiologi. https://doi.org/10.5324/nje.v13i1.305
Valla M, Vatten LJ, Engstrom MJ, Haugen OA, Akslen LA, Bjorngaard JH et al (2016) Molecular subtypes of breast cancer: long-term incidence trends and prognostic differences. Cancer Epidemiol Biomarkers Prev 25(12):1625–1634
Sandvei MS, Opdahl S, Valla M, Lagiou P, Vesterfjell EV, Rise TV et al (2021) The association of women’s birth size with risk of molecular breast cancer subtypes: a cohort study. BMC Cancer 21(1):299
Research-based evaluation of The Norwegian Breast Cancer Screening Program [press release] (2015). Oslo, Norway.
Norway CRo (2022) Cancer in Norway 2021—cancer incidence, mortality, survival and prevalence in Norway. Oslo.
Hofvind S, Ursin G, Tretli S, Sebuodegard S, Moller B (2013) Breast cancer mortality in participants of the Norwegian breast cancer screening program. Cancer 119(17):3106–3112
Weedon-Fekjaer H, Romundstad PR, Vatten LJ (2014) Modern mammography screening and breast cancer mortality: population study. BMJ 348:g3701
Early Breast Cancer Trialists’ Collaborative G (1988) Effects of adjuvant tamoxifen and of cytotoxic therapy on mortality in early breast cancer: an overview of 61 randomized trials among 28,896 women. N Engl J Med 319(26):1681–1692
ATAC The (Arimidex TAoiCTG) (2002) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet 359(9324):2131–2139
Scabia V, Ayyanan A, De Martino F, Agnoletto A, Battista L, Laszlo C et al (2022) Estrogen receptor positive breast cancers have patient specific hormone sensitivities and rely on progesterone receptor. Nat Commun 13(1):3127
Schrodi S, Braun M, Andrulat A, Harbeck N, Mahner S, Kiechle M et al (2021) Outcome of breast cancer patients with low hormone receptor positivity: analysis of a 15-year population-based cohort. Ann Oncol 32(11):1410–1424
Fusco N, Ragazzi M, Sajjadi E, Venetis K, Piciotti R, Morganti S et al (2021) Assessment of estrogen receptor low positive status in breast cancer: implications for pathologists and oncologists. Histol Histopathol 36(12):1235–1245
Kim MC, Park MH, Choi JE, Kang SH, Bae YK (2022) Characteristics and prognosis of estrogen receptor low-positive breast cancer. J Breast Cancer 25(4):318–326
Chen T, Zhang N, Moran MS, Su P, Haffty BG, Yang Q (2018) Borderline ER-positive primary breast cancer gains no significant survival benefit from endocrine therapy: a systematic review and meta-analysis. Clin Breast Cancer 18(1):1–8
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S et al (2010) American society of clinical oncology/college of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. Arch Pathol Lab Med 134(6):907–922
Ogawa Y, Moriya T, Kato Y, Oguma M, Ikeda K, Takashima T et al (2004) Immunohistochemical assessment for estrogen receptor and progesterone receptor status in breast cancer: analysis for a cut-off point as the predictor for endocrine therapy. Breast Cancer 11(3):267–275
Iwamoto T, Booser D, Valero V, Murray JL, Koenig K, Esteva FJ et al (2012) Estrogen receptor (ER) mRNA and ER-related gene expression in breast cancers that are 1% to 10% ER-positive by immunohistochemistry. J Clin Oncol 30(7):729–734
Fujii T, Kogawa T, Dong W, Sahin AA, Moulder S, Litton JK et al (2017) Revisiting the definition of estrogen receptor positivity in HER2-negative primary breast cancer. Ann Oncol 28(10):2420–2428
Voorwerk L, Sanders J, Keusters MS, Balduzzi S, Cornelissen S, Duijst M et al (2023) Immune landscape of breast tumors with low and intermediate estrogen receptor expression. NPJ Breast Cancer 9(1):39
Mirlacher M, Kasper M, Storz M, Knecht Y, Durmuller U, Simon R et al (2004) Influence of slide aging on results of translational research studies using immunohistochemistry. Mod Pathol 17(11):1414–1420
Grillo F, Bruzzone M, Pigozzi S, Prosapio S, Migliora P, Fiocca R et al (2017) Immunohistochemistry on old archival paraffin blocks: is there an expiry date? J Clin Pathol 70(11):988–993
Dowsett T, Verghese E, Pollock S, Pollard J, Heads J, Hanby A et al (2014) The value of archival tissue blocks in understanding breast cancer biology. J Clin Pathol 67(3):272–275
Karlsson C, Karlsson MG (2011) Effects of long-term storage on the detection of proteins, DNA, and mRNA in tissue microarray slides. J Histochem Cytochem 59(12):1113–1121
Larsen IK, Smastuen M, Johannesen TB, Langmark F, Parkin DM, Bray F et al (2009) Data quality at the cancer registry of Norway: an overview of comparability, completeness, validity and timeliness. Eur J Cancer 45(7):1218–1231
Bakken IJ, Ellingsen CL, Pedersen AG, Leistad L, Kinge JM, Ebbing M et al (2015) Comparison of data from the cause of death registry and the norwegian patient register. Tidsskr Nor Laegeforen 135(21):1949–1953
Torhorst J, Bucher C, Kononen J, Haas P, Zuber M, Köchli OR et al (2001) Tissue microarrays for rapid linking of molecular changes to clinical endpoints. Am J Pathol 159(6):2249–2256
Rosen DG, Huang X, Deavers MT, Malpica A, Silva EG, Liu J (2004) Validation of tissue microarray technology in ovarian carcinoma. Mod Pathol 17(7):790–797
Acknowledgements
The authors would like to thank the Department of Pathology at St. Olav´s Hospital, Trondheim University Hospital for making the diagnostic archives available for this project and the Cancer Registry of Norway for supplying the corresponding patient data.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). This present study has received funding from the Department of Clinical and Molecular Medicine, Norwegian University of Science and Technology, Trondheim, Norway. Data included in this study received financial support from the Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology and The Research Council of Norway.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by all authors. The first draft of the manuscript was written by Anette H Skjervold. All authors commented on previous versions of the manuscript, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no competing interests.
Ethical approval
This study and publication of its results was granted approval by the Regional Committee for Medical and Health Research Ethics, Central Norway (REK 836-09). The approval includes dispensation from the usual requirement of patient consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Skjervold, A.H., Valla, M. & Bofin, A.M. Oestrogen receptor low positive breast cancer: associations with prognosis. Breast Cancer Res Treat 201, 535–545 (2023). https://doi.org/10.1007/s10549-023-07040-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07040-9