Abstract
Objective
Metaplastic breast cancer (MpBC) is an aggressive subtype of all breast cancer. We aimed to investigate the clinicopathological features, treatments and prognoses of MpBC patients.
Methods
We collected the data from MpBC patients diagnosed at Tianjin Medical University Cancer Hospital from 2010 to 2017. Kaplan Meier curves and Cox regression model were used to evaluating clinical outcomes and prognostic factors. After removing baseline differences by propensity score matching (PSM), we analyzed the prognosis between MpBC patients and invasive ductal carcinomas of no special type (IDC-NST) patients.
Results
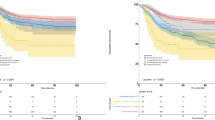
A total of 217 MpBC patients were subsumed. Of all histological subtypes, 45.1% were mixed subtypes, followed by with mesenchymal differentiation (27.2%), pure squamous (15.2%) and pure spindle (12.4%) subtypes. 69.6% of MpBC were triple-negative, 25.3% and 6.5% were HR-positive and HER2-positive. MpBC patients had worse survival compared to IDC-NST patients, with 5-year RFS of 73.8 and 83.6% (HR = 1.177 95%CI (1.171–2.676) P = 0.0068), and 5-year BCSS of 79.0% and 89.7% (HR = 2.187 95%CI (1.357–3.523) P = 0.0013). In the multivariate COX model, AJCC stage, mixed subtype and chemotherapy were independent prognostic factors. Mixed MpBC is more aggressive than pure and with heterologous mesenchymal differentiation subtypes. And whether squamous or spindle MpBC, mixed forms have shorter outcomes than pure forms.
Conclusions
MpBCs are associated with poorer prognoses than IDC-NSTs. They are heterogeneous with different clinicopathological features and clinical outcomes between histological subtypes. Pure and with heterologous mesenchymal differentiation subtypes have more survival benefits than the mixed subtype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
MpBC is a rare subtype that constitutes 0.2–5% of all breast cancer [1]. It has heterogeneity which features the transformation of the neoplastic cells toward epithelial or (and) mesenchymal components. The 5th edition of the WHO classification includes six subtypes: pure squamous cell carcinoma, pure spindle cell carcinoma, metaplastic carcinoma with heterologous mesenchymal differentiation (e.g., chondroid, osseous, rhabdomyoid and neuroglial), fibromatosis-like metaplastic carcinoma, low-grade adenosquamous carcinoma, mixed metaplastic carcinoma [2]. Mixed metaplastic carcinoma is defined as a tumor with different metaplastic components or a mixture of metaplastic and conventional adenocarcinoma components. The cutoff value of the metaplastic component is not indicated in the WHO classification. However, considering that IDC-NST may have a tiny metaplastic component, we defined it as the metaplastic component ≥ 10%, and if the component ≥ 90% is pure MpBC.
Excepted for some low-grade subtypes, MpBCs often have large tumors and high grades and tend to have distant metastases compared to lymph node metastases. The absence of HR and HER2 expression and insensitivity to chemoradiotherapy lead to its poor prognosis. Given its rarity, most studies are limited to small samples and are known little. Many findings have shown that MpBC has shorter survival than IDC-NST [3,4,5,6,7,8], but several have remained different conclusions [9, 10]. Considered without standardized and effective treatments for MpBC, it remains a challenge to treat it. Further exploration of new treatment modalities for MpBC is necessary. We aimed to analyze the clinicopathological features, survival outcomes and treatments of MpBC.
Materials and methods
Population
This study collected 217 cases of MpBC patients treated at Tianjin Medical University Cancer Hospital from 2010 to 2017. In order to compare the differences between MpBC and IDC-NST, we collected IDC-NST patients from our hospital during the same period. The criteria for inclusion were (1) Female, (2) Age ≥ 18 years, (3) Pathologically confirmed MpBC/IDC-NST, (4) No history of other malignancy, (5) Non-IV stage.
Variables
The clinicopathological characteristics used in the analysis included age at diagnosis, Nottingham grade, post-operative TNM stage (if not, use clinical stage), molecular subtype, ER status, PR status, HER2 status, Ki-67 index, P53 status, surgery type, neoadjuvant treatment, chemoradiotherapy. The judgement of TNM stage of breast cancer was followed by the American Joint Committee on Cancer (AJCC) guideline. HER2-positive implied an immunohistochemistry (IHC) score of 3 + or 2 + but with the CEP-17 ratio ≥ 2.0 using fluorescent in situ hybridization (FISH).
Outcomes
Relapse-free Survival (RFS) was the time interval from radical treatment to tumor progression (recurrence or metastasis) or death from this disease. Breast cancer-specific survival (BCSS) was the interval between breast cancer diagnosis and death from this disease or the latest follow-up visit.
Statistical analysis
The clinicopathological characteristics of MpBC and IDC-NST were analyzed for comparison using X2 and Fisher's exact tests. PSM was used to correct objective differences between the MpBC and IDC-NST groups with the caliper value of 0.01. The Kaplan–Meier curve and log-rank test were used to assess and compare clinical outcomes. Univariate and multivariate COX proportional models were used to acquire prognostic factors for MpBC. Graphpad prism (8.0) was used for plotting, PSM was performed using R software (4.2.0), and the rest were analyzed using SPSS (26.0). Every test was two-sided. When P value < 0 0.05, which considered it had statistical significance.
Result
Clinicopathological characteristics of MpBC
A total of 243 MpBC patients were collected; 15 cases of double primary cancer, two cases of stage IV at diagnosis and five cases with less than six months of follow-up were removed; In addition, two cases of adenosquamous carcinomas and four cases fibromatosis-like metaplastic carcinomas were too few to analysis. The remaining 217 patients were subsumed. As shown in Table 1, most patients (58.1%, n = 126) were postmenopausal women, and the median age at diagnosis was 53 years (range 25–87 years). Most tumors had AJCC stage II (63.1%, n = 137), T2 size (62.2%, n = 135) and without lymph node metastases (71.9%, n = 156). The preference for grade 3 (78.3%, n = 170) and high Ki-67 index (≥ 30%) (84.9%, n = 182). Of all the pathological subtypes, 45.1% (n = 98) were mixed subtypes, 27.2% (n = 59) were MpBC with mesenchymal differentiation, 15.2% (n = 33) and 12.4% (n = 27) were pure squamous and pure spindle subtypes. The majority (69.6%, n = 151) were HR-HER2- tumors, 24.0% (n = 52) were HR + HER2- tumors, 5.1% (n = 11) and 1.4% (n = 3) were HR-HER2 + and HR + HER2 + tumors, respectively. Most first preferred surgery, with only 7.4% (n = 16) receiving neoadjuvant treatments. Nearly all (93.5%, n = 203) received chemotherapy after surgery, and 28.1% (n = 61) received radiotherapy. Among the chemotherapy regimens, 39.2% (n = 85) of patients received the anthracyclines followed by taxanes (A–T) regimen, with 31.8% (n = 69) for the combined taxanes and anthracyclines (T+A) regimen, 11.5% (n = 25) for the taxanes or anthracyclines (T/A) regimen and 4.6% (n = 12) for the platinum-containing regimen.
Survival analysis of MpBC
The median follow-up time for patients was 61 months (range 6–146 months). The 5-year RFS and BCSS were 73.8 and 79.0%, and the 10-year RFS and BCSS were 70.4 and 64.9%, respectively (Figs. 1 and 2). 26.3% of patients (n = 57) had recurrences, and 22.1% (n = 48) had died of this disease. The most common sites of metastasis were lung (n = 30), bone (n = 19), pleural effusion or ascites (n = 13), chest wall (n = 11), liver (n = 7) and brain (n = 7). Prognostic factors for MpBC were evaluated using the Cox regression model. In univariate analysis, AJCC stage (P = 0.006), T size 2-5 cm (P = 0.010), lymph node metastases (P = 0.018), mixed subtype (pure vs. mixed P = 0.003; with mesenchymal differentiation vs. mixed P = 0.005) and chemotherapy (P = 0.003) were considered unfavorable for RFS. Age (P = 0.003), AJCC stage (P = 0.002), T size 2–5 cm (P = 0.005), lymph node metastases (P = 0.006), mixed subtype (pure vs. mixed P = 0.003; with mesenchymal differentiation vs. mixed P = 0.005) and chemotherapy (P = 0.002) were associated with BCSS. To eliminate confounding factors, variables with P value < 0.1 were included in the multivariate analysis model. Only AJCC stage (stage 0–I as reference, stage II HR = 2.698 95%CI (1.046–6.956) P = 0.040; stage III HR = 4.294 95%CI (1.463–12.600) P = 0.008), histological subtype (pure vs. mixed HR = 2.626 95%CI (1.253–5.502) P = 0.011; with mesenchymal differentiation vs. mixed HR = 2.136 95%CI (1.043–4.371) P = 0.038) and chemotherapy (HR = 0.271 95%CI (0.126–0.584) P = 0.001) were independent indicators for RFS. AJCC stage (stage 0–I as reference, stage II HR = 5.439 95%CI (1.286–22.999) P = 0.021; stage III HR = 10.080 95%CI (2.153–47.199) P = 0.003), histological subtype (pure vs. mixed HR = 2.731 95%CI (1.183–6.305) P = 0.019) and chemotherapy (HR = 0.260 95%CI (0.117–0.576) P = 0.001) were independent indicators for BCSS (Tables 2 and 3). Unlike common invasive breast cancer, we did not observe the significant association between HR and HER2 status and survival outcomes. In addition, radiotherapy did not improve RFS and BCSS.
Analysis of the prognosis differences between MpBC and IDC-NST
Since baseline imbalance may induce outcome discrepancies, we used the PSM to 1:1 matching, 217 IDC-NST patients were screened in comparison with MpBC patients, and the chosen factors were matched well between the two groups (Table 1). It can be seen that MpBC had inferior survival compared with IDC-NST, with 5-year RFS of 73.8 and 83.6% (HR = 1.177 95%CI (1.171–2.676) P = 0.0068), and 5-year BCSS of 79.0% and 89.7% (HR = 2.187 95%CI (1.357–3.523) P = 0.0013). (Figs. 1 and 2).
Subgroup analysis of MpBC
We drew their survival curves according to the histological subtypes (Fig. 3). Mixed MpBC had a poorer prognosis than MpBC with mesenchymal differentiation and pure MpBC, with 5-years RFS of 60.7, 83.5 and 86.0% (P = 0.0004) and 5-years BCSS of 67.5, 93.9 and 88.7%, respectively (P = 0.0004). The survival outcomes of with mesenchymal differentiation and pure subtypes had no statistical difference. The clinicopathological characteristics of different subtypes were compared using the X2 and Fisher's exact test (Table 4). The mixed subtype preferred higher AJCC stages (P = 0.001), bigger tumors (P = 0.005), more lymph node involvements (P = 0.024), higher Nottingham grade (P = 0.033), higher Ki-67 index (P < 0.001) and more HER2 expression (P = 0.032).
Further dividing mixed MpBC, 53 cases were mixed squamous subtypes and 45 cases were mixed spindle subtypes. For the mixture component, 96 cases were IDC-NST, one case was invasive carcinoma with neuroendocrine differentiation and one case was invasive carcinoma with apocrine differentiation. 95 cases had only one metaplastic component, two cases had squamous and spindle elements, and one case had spindle and osseous elements. We performed subgroup analysis for pure and mixed MpBC. Either squamous or spindle MpBC, mixed forms had worse outcomes than pure forms (Fig. 4). For mixed and pure squamous MpBC, their 5-year RFS were 66.4% and 90.6% (HR = 2.539 95%CI (1.061–6.075) P = 0.0363) and 5-year BCSS were 69.1 and 93.1% (HR = 2.805 95%CI (1.096–7.180) P = 0.0315). For mixed and pure spindle MpBC, their 5-year RFS were 54.5 and 80.8% (HR = 2.492 95%CI (1.136–5.467) P = 0.0227) and 5-year BCSS were 65.7 and 83.5% (HR = 2.449 95%CI (1.034–5.801) P = 0.0418). In contrast, the prognoses of pure squamous and pure spindle subtypes showed no significant differences. The clinicopathological characteristics between pure and mixed subtypes are shown in Table 5. Mixed squamous MpBC had higher AJCC stages (P = 0.034), larger tumors (P = 0.027), higher Nottingham grade (P = 0.026), and higher Ki-67 index (P = 0.009) than the pure subtype. Compared to the pure spindle subtype, mixed had higher AJCC stages (P = 0.036), more lymph node metastases (P = 0.019), more HR expression (P = 0.017) and higher Ki-67 index (P = 0.020).
Treatment strategies of MpBC
MpBC responded poorly to neoadjuvant chemotherapy (NAC). Of all 16 patients who received NAC, only 6.3% (n = 1) patients achieved pathological complete response (pCR) and 56.3% (n = 9) changed treatment regimens due to NC (no significant change) or PD (progressive disease), ultimately 37.5% (n = 6) occurred recurrences or metastases.
93.6% of patients (n = 15) preferred the T+A regimen, and all nine patients had the platinum-containing regimen as the second-line regimen.
For the subgroup analysis of adjuvant therapy, receiving the T+A regimen had more prolonged RFS and BCSS than receiving the T/A regimen (P = 0.003 and P = 0.014). Receiving other regimens (including capecitabine; mesna, doxorubicin, ifosfamide and dacarbazine (MAID) and unknown regimens) had shorter RFS and BCSS compared to receiving the T+A regimen (P = 0.004 and P = 0.002) (Fig. 5). In contrast, receiving A−T or platinum-containing regimens had inferior RFS compared to receiving the T+A regimen but without statistical significance (P = 0.093 and P = 0.052). We did not observe survival differences in BCSS between receiving A–T or platinum-containing regimens and the T+A regimen (P = 0.348 and P = 0.297).
Endocrine and targeted therapy may be required for HR-positive and HER2-positive patients. Of HR-positive patients, more than half (n = 29) used endocrine therapy (using more than 6 months). The K–M curves of the two groups with or without endocrine therapy were shown no statistical differences between these two cohorts (Fig. 6). Of HER2-positive patients, 57.1% (n = 8) were treated with anti-HER2 therapy (using more than twice), and only two without targeted therapy had recurrence and death.
Discussion
MpBC is a heterogeneous subtype of breast cancer that they are highly invasive and more prone to distant metastases except for fibromatosis-like metaplastic carcinoma and low-grade adenosquamous carcinoma [11].
There are controversies about prognoses of other histological subtypes. MpBCs are classified as monophasic (only one metaplastic component) or biphasic (both metaplastic and non-metaplastic components) tumors. The former includes pure SpCC and SqCC, and the latter includes mixed MpBC and MpBC with heterologous mesenchymal differentiation. In monophasic MpBC, Rakha et al. [9] and McCart et al. [12] also indicated that squamous cell carcinoma had more prolonged survival while Tadros et al. [8] reported a worse outcome for it. In biphasic MpBC, we found that patients with mesenchymal differentiation had better RFS and BCSS. Tadros et al. [8], Rakha et al. [9] and Takala et al. [13] also demonstrated this finding. The lack of PI-3 kinase and Ras-Map kinase aberrations and TERT promoter mutations may account for their less aggressive feature [14]. For mixed MpBC, previously, scholars generally agreed that it contains two or more metaplastic components. It revealed that conventional mixed MpBC had a worse outcome [13, 15, 16], and the prognosis was worse with the number of components increasing [12]. After publishing the 5th edition of the WHO classification, metaplastic carcinoma with adenocarcinoma component was also classified as a mixed subtype. In this study, most mixed MpBCs were the mixture of one metaplastic component with invasive ductal carcinoma. The mixed subtypes with either squamous or spindle differentiation had shorter survival outcomes than the pure subtypes. Consistent with our findings, recent research of 39 squamous cell carcinomas showed that invasive carcinoma with squamous differentiation had a worse prognosis and was more aggressive than pure squamous subtype [17]. A similar phenomenon was seen in uterine carcinosarcoma, where Renske et al. found that most metastases (72%) and vascular invasion (70%) were caused by epithelial components rather than mesenchymal components [18]. These phenomena suggest the need for further research into the origin of MpBC. The conversion theory is generally accepted, which asserts that the mesenchymal component is derived from the epithelial component through metaplastic progress. Some studies confirmed that when MpBC with the invasive ductal component, the genetic progression and evolution of its metaplastic component was from its paired invasive ductal carcinoma [14, 19]. The poorer prognosis of mixed MpBC with invasive carcinoma may imply that the epithelial component drives the high proliferation of MpBC. For example, vascular endothelial growth factor [20] and matrix metalloproteinase-7 (MMP-7) [21] were higher expressed in the epithelial component compared to the mesenchymal component, all of which contribute to its invasion and metastasis. In contrast, a study of mixed histological subtypes of invasive breast carcinoma showed no prognostic difference between pure and mixed MpBC [22], possibly due to the small sample sizes and subtype discrepancies included in their cohort. The different conclusions may reflect the different classification criteria and sample sizes of each study, furthermore, it is recommended that pathologists should record the morphology and proportion of each component at diagnosis in order to make subsequent therapeutic options.
The prognostic significance of clinicopathological features has been reported a lot, but there is no consensus on the most useful. Multiple reports, including our study, have found the mixed subtype to be an unfavorable factor [12, 13, 15, 16]. Many authors regarded tumor size was correlated with survival [12, 13, 15, 23, 24]. However, one multi-center research indicated that only lymph node status and lymphovascular invasion influenced prognosis, not tumor size and histological grade [9]. A series of studies with the SEER database proved that age and TNM stage were all independent prognostic factors [25,26,27,28]. Chemotherapy was effective for survival, but there remains controversy in radiotherapy. Multiple research confirmed that radiotherapy could improve OS or BCSS[6, 29, 30], but some considered it of limited benefit. For example, Leyrer et al. showed it decreased the local–regional but not distant recurrence [31]. Haque et al. suggested that mastectomy with radiotherapy was associated with improved OS only in the high-risk (T3–4 or node-positive) but lumpectomy with it both in high or low-risk (T1–2N0) cohorts[32]. Similar to us, a multi-center study showed no association between radiotherapy and outcomes[9]. These biases may be caused by objective differences between Asian and Western cohorts, with only 5.6–28.1% receiving radiotherapy in our and other Asian studies[3] but 37.9–92.9% in Western studies[33]. Besides, it showed that surgery type [34, 35] and race [5, 25] might affect clinical outcomes.
MpBCs are often triple-negative breast cancers, but up to 23 and 5.2% acquired HR and HER2 according to an analysis for SEER [36], which was broadly similar to our results (25.3 and 6.5%). HR-positive breast cancer is usually considered to have a better outcome. However, recent findings, including ours, found that HR-positive status and endocrine therapy might not provide a survival benefit for MpBC patients [25, 27]. Wu et al. [37] observed that HR-positive increased the death risk compared to HR-negative subtypes. In contrast, one research based on NCDB held the opposite view suggesting that endocrine therapy can improve OS [7]. In addition, our study showed HER2 status was not associated with prognosis. Interestingly, one revealed that HER2-positive MpBC might derive more benefits for survival [36], but Lei et al. [38] reported that HER2-positive squamous carcinoma was associated with an inferior prognosis. Rare reports mentioned targeted therapy for MpBC. In our research, none of the eight patients receiving targeted therapy had recurred, while two of the remaining six patients occurred recurrence and death. Anti-HER2 therapy appears to improve the prognoses of HER2-positive patients. But it is not convincing due to the limited sample size. It requires us to expand the sample to prove this conclusion.
MpBC has little response to NAC, with previous studies showing the pCR rate in the range of 0–17% [7, 15, 16, 23, 24, 39]. A recent prospective trial (NCT02276443) showed the pCR rate reaching 23% [40]. In this study, only 6.3% of MpBC patients achieved pCR, which contrasts with high pCR rates in TNBC, 30–40% with T+A regimens and over 50% with platinum-containing regimens [41, 42]. It has been certified that the enrichment of the EMT pathway and the widespread expression of tumor stem cells in MpBC make them resistant to anthracycline and paclitaxel drugs [43, 44]. Besides, the up-regulation of FOXC1 plays an important part in this process [45]. For the adjuvant treatment, the T+A regimen substantially improved the RFS and BCSS of MpBC. Unlike it is reported to be effective for TNBC, the platinum-containing regimen did not have a better outcome than the T+A regimen in our analysis, possibly due to less use and clinician selection bias, with a preference for platinum when large tumors or lymph node metastases. However, it seems to be improved when using the dense dose. A retrospective review reported that weekly paclitaxel and platinum chemotherapy could prolong survival significantly [46].
Because of deriving less benefit from chemoradiotherapy and endocrine therapy, exploring efficient treatments becomes an urgent need. With more researchers finding the prevalence of PI3K mutations in MpBC [12, 47,48,49], inhibitors of the PI3K/AKT/mTOR pathway combined with chemotherapy or targeted therapy have provided effective therapeutic methods [50, 51]. Furthermore, MpBC has been reported that frequent expression of programmed death-ligand 1 (PD-L1) which is similar to TN-IDC [44, 47, 48, 52, 53]. Several clinical trials (NCT02834013, NCT02752685) using anti-PD-1/PD-L1 antibodies in advanced MpBC patients have achieved explicit survival benefits [54, 55]. Other studies have proved that TERT promoter hotspot mutations [56] and the RPL39 A14V mutations [57] occur at high frequency in MpBC, and MYC amplification is highly enriched after metastasis [58]. These may become potential targets for treating MpBC in the future.
This study presented the clinicopathological characteristics, treatment strategies and prognoses of 217 patients with MpBC from our institution over eight years and compared them with IDC-NST. This study has some limitations: Firstly, it may have some selection bias because of its retrospective analysis and limited sample size. Secondly, this research is single-center, and the cases included may have local characteristics and limitations. Finally, some indicators such as Ki-67, P53 and menopausal status can't be matched, so there may still be an imbalance between the two cohorts. However, our study is one of the largest single institutions by far to include relatively comprehensive clinicopathological features of this rare tumor, and it’s representative and credible due to the long follow-up period and wide sample variety.
Conclusion
MpBC is associated with shorter survival than IDC-NST. Different histological subtypes have unique clinicopathological features and survival outcomes. The mixed subtype is more aggressive than pure and with heterologous mesenchymal differentiation subtypes. It provides direction for making therapeutic guidelines in clinical. For the rare MpBC expressed HR and HER2, it seems that anti-HER2 therapy but not endocrine therapy provides benefits in survival. However, it necessary to expand samples to explore this research further.
Data availability
The datasets in this study can be available from the corresponding author upon reasonable request.
References
Reddy TP, Rosato RR, Li X et al (2020) A comprehensive overview of metaplastic breast cancer: clinical features and molecular aberrations. Breast Cancer Res 22:121. https://doi.org/10.1186/s13058-020-01353-z
Cserni G (2020) Histological type and typing of breast carcinomas and the WHO classification changes over time. Pathologica 112:25–41. https://doi.org/10.32074/1591-951X-1-20
Zhang Y, Lv F, Yang Y et al (2015) Clinicopathological features and prognosis of metaplastic breast carcinoma: experience of a major Chinese cancer center. PLoS One 10:e0131409. https://doi.org/10.1371/journal.pone.0131409
El Zein D, Hughes M, Kumar S et al (2017) Metaplastic carcinoma of the breast is more aggressive than triple-negative breast cancer: a study from a single institution and review of literature. Clin Breast Cancer 17:382–391. https://doi.org/10.1016/j.clbc.2017.04.009
Li Y, Zhang N, Zhang H, Yang Q (2019) Comparative prognostic analysis for triple-negative breast cancer with metaplastic and invasive ductal carcinoma. J Clin Pathol 72:418–424. https://doi.org/10.1136/jclinpath-2018-205544
Moreno AC, Lin YH, Bedrosian I et al (2020) Outcomes after treatment of metaplastic versus other breast cancer subtypes. J Cancer 11:1341–1350. https://doi.org/10.7150/jca.40817
Polamraju P, Haque W, Cao K et al (2020) Comparison of outcomes between metaplastic and triple-negative breast cancer patients. The Breast 49:8–16. https://doi.org/10.1016/j.breast.2019.10.003
Tadros AB, Sevilimedu V, Giri DD et al (2021) Survival outcomes for metaplastic breast cancer differ by histologic subtype. Ann Surg Oncol 28:4245–4253. https://doi.org/10.1245/s10434-020-09430-5
Rakha EA, Tan PH, Varga Z et al (2015) Prognostic factors in metaplastic carcinoma of the breast: a multi-institutional study. Br J Cancer 112:283–289. https://doi.org/10.1038/bjc.2014.592
Corso G, Frassoni S, Girardi A et al (2021) Metaplastic breast cancer: prognostic and therapeutic considerations. J Surg Oncol 123:61–70. https://doi.org/10.1002/jso.26248
McMullen ER, Zoumberos NA, Kleer CG (2019) Metaplastic breast carcinoma: update on histopathology and molecular alterations. Arch Pathol Lab Med 143:1492–1496. https://doi.org/10.5858/arpa.2019-0396-RA
McCart Reed AE, Kalaw E, Nones K et al (2019) Phenotypic and molecular dissection of metaplastic breast cancer and the prognostic implications: prognostic features of metaplastic breast cancer. J Pathol 247:214–227. https://doi.org/10.1002/path.5184
Takala S, Heikkilä P, Nevanlinna H et al (2019) Metaplastic carcinoma of the breast: prognosis and response to systemic treatment in metastatic disease. Breast J 25:418–424. https://doi.org/10.1111/tbj.13234
Krings G, Chen Y-Y (2018) Genomic profiling of metaplastic breast carcinomas reveals genetic heterogeneity and relationship to ductal carcinoma. Mod Pathol 31:1661–1674. https://doi.org/10.1038/s41379-018-0081-z
Cimino-Mathews A, Verma S, Figueroa-Magalhaes MC et al (2016) A clinicopathologic analysis of 45 patients with metaplastic breast carcinoma. Am J Clin Pathol 145:365–372. https://doi.org/10.1093/ajcp/aqv097
Han M, Salamat A, Zhu L et al (2019) Metaplastic breast carcinoma: a clinical-pathologic study of 97 cases with subset analysis of response to neoadjuvant chemotherapy. Mod Pathol 32:807–816. https://doi.org/10.1038/s41379-019-0208-x
Pirot F, Chaltiel D, Ben Lakhdar A et al (2020) Squamous cell carcinoma of the breast, are there two entities with distinct prognosis? A series of 39 patients. Breast Cancer Res Treat 180:87–95. https://doi.org/10.1007/s10549-020-05525-5
de Jong RA, Nijman HW, Wijbrandi TF et al (2011) Molecular markers and clinical behavior of uterine carcinosarcomas: focus on the epithelial tumor component. Mod Pathol 24:1368–1379. https://doi.org/10.1038/modpathol.2011.88
Moukarzel LA, Ferrando L, Da Cruz PA et al (2021) The genetic landscape of metaplastic breast cancers and uterine carcinosarcomas. Mol Oncol 15:1024–1039. https://doi.org/10.1002/1878-0261.12813
Emoto M, Iwasaki H, Ishiguro M et al (1999) Angiogenesis in carcinosarcomas of the uterus: differences in the microvessel density and expression of vascular endothelial growth factor between the epithelial and mesenchymal elements. Hum Pathol 30:1232–1241. https://doi.org/10.1016/S0046-8177(99)90043-6
Tanimoto H, Shigemasa K, Sasaki M et al (2000) Differential expression of matrix metalloprotease-7 in each component of uterine carcinosarcoma. Oncol Rep. https://doi.org/10.3892/or.7.6.1209
Rechsteiner A, Dietrich D, Varga Z (2022) Prognostic relevance of mixed histological subtypes in invasive breast carcinoma: a retrospective analysis. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-022-04443-x
Wong W, Brogi E, Reis-Filho JS et al (2021) Poor response to neoadjuvant chemotherapy in metaplastic breast carcinoma. NPJ Breast Cancer 7:96. https://doi.org/10.1038/s41523-021-00302-z
Abada E, Daaboul F, Ebare K et al (2022) Clinicopathologic characteristics and outcome descriptors of metaplastic breast carcinoma. Arch Pathol Lab Med 146:341–350. https://doi.org/10.5858/arpa.2020-0830-OA
Mao J, Hu J, Zhang Y et al (2021) Single hormone receptor-positive metaplastic breast cancer: similar outcome as triple-negative subtype. Front Endocrinol 12:628939. https://doi.org/10.3389/fendo.2021.628939
Hu J, Zhang H, Dong F et al (2021) Metaplastic breast cancer: treatment and prognosis by molecular subtype. Transl Oncol 14:101054. https://doi.org/10.1016/j.tranon.2021.101054
Wang S, Hu J, Zhang Y et al (2021) Presentation and survival by hormonal receptor status in metaplastic breast cancer: a propensity score-matched analysis. The Breast 60:168–176. https://doi.org/10.1016/j.breast.2021.10.004
Zhu K, Chen Y, Guo R et al (2022) Prognostic factor analysis and model construction of triple-negative metaplastic breast carcinoma after surgery. Front Oncol 12:924342. https://doi.org/10.3389/fonc.2022.924342
Ong CT, Campbell BM, Thomas SM et al (2018) Metaplastic breast cancer treatment and outcomes in 2500 patients: a retrospective analysis of a national oncology database. Ann Surg Oncol 25:2249–2260. https://doi.org/10.1245/s10434-018-6533-3
He X, Ji J, Dong R et al (2019) Prognosis in different subtypes of metaplastic breast cancer: a population-based analysis. Breast Cancer Res Treat 173:329–341. https://doi.org/10.1007/s10549-018-5005-6
Leyrer CM, Berriochoa CA, Agrawal S et al (2017) Predictive factors on outcomes in metaplastic breast cancer. Breast Cancer Res Treat 165:499–504. https://doi.org/10.1007/s10549-017-4367-5
Haque W, Verma V, Naik N et al (2018) Metaplastic breast cancer: practice patterns, outcomes, and the role of radiotherapy. Ann Surg Oncol 25:928–936. https://doi.org/10.1245/s10434-017-6316-2
Thomas HR, Hu B, Boyraz B et al (2023) Metaplastic breast cancer: a review. Crit Rev Oncol Hematol 182:103924. https://doi.org/10.1016/j.critrevonc.2023.103924
Zhang J, Yang C, Lei C et al (2021) Survival outcomes after breast-conserving therapy compared with mastectomy for patients with early-stage metaplastic breast cancer: a population-based study of 2412 patients. The Breast 58:10–17. https://doi.org/10.1016/j.breast.2021.03.010
Hu J, Dong F, Zhang Y et al (2021) Triple-negative metaplastic breast cancer: treatment and prognosis by type of surgery. Am J Transl Res 13:11689
Schroeder MC, Rastogi P, Geyer CE et al (2018) Early and locally advanced metaplastic breast cancer: presentation and survival by receptor status in surveillance, epidemiology, and end results (SEER) 2010–2014. Oncologist 23:481–488. https://doi.org/10.1634/theoncologist.2017-0398
Wu S-G, Yang S-P, Zhang W-W et al (2020) The longitudinal risk of mortality between invasive ductal carcinoma and metaplastic breast carcinoma. Sci Rep 10:22070. https://doi.org/10.1038/s41598-020-79166-5
Lei T, Pu T, Wei B et al (2022) Clinicopathologic characteristics of HER2-positive metaplastic squamous cell carcinoma of the breast. J Clin Pathol 75:18–23. https://doi.org/10.1136/jclinpath-2020-206468
Al-Hilli Z, Choong G, Keeney MG et al (2019) Metaplastic breast cancer has a poor response to neoadjuvant systemic therapy. Breast Cancer Res Treat 176:709–716. https://doi.org/10.1007/s10549-019-05264-2
Yam C, Abuhadra N, Sun R et al (2022) Molecular characterization and prospective evaluation of pathologic response and outcomes with neoadjuvant therapy in metaplastic triple-negative breast cancer. Clin Cancer Res 28:2878–2889. https://doi.org/10.1158/1078-0432.CCR-21-3100
Cortazar P, Zhang L, Untch M et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. The Lancet 384:164–172. https://doi.org/10.1016/S0140-6736(13)62422-8
Poggio F, Bruzzone M, Ceppi M et al (2018) Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: a systematic review and meta-analysis. Ann Oncol 29:1497–1508. https://doi.org/10.1093/annonc/mdy127
Oon ML, Thike AA, Tan SY, Tan PH (2015) Cancer stem cell and epithelial–mesenchymal transition markers predict worse outcome in metaplastic carcinoma of the breast. Breast Cancer Res Treat 150:31–41. https://doi.org/10.1007/s10549-015-3299-1
González-Martínez S, Pérez-Mies B, Pizarro D et al (2021) Epithelial mesenchymal transition and immune response in metaplastic breast carcinoma. IJMS 22:7398. https://doi.org/10.3390/ijms22147398
Kumar U, Hu Y, Masrour N et al (2021) MicroRNA-495/TGF-β/FOXC1 axis regulates multidrug resistance in metaplastic breast cancer cells. Biochem Pharmacol 192:114692. https://doi.org/10.1016/j.bcp.2021.114692
Harper NW, Hodges KB, Stewart RL et al (2019) Adjuvant treatment of triple-negative metaplastic breast cancer with weekly paclitaxel and platinum chemotherapy: retrospective case review from a single institution. Clin Breast Cancer 19:e495–e500. https://doi.org/10.1016/j.clbc.2019.05.009
Joneja U, Vranic S, Swensen J et al (2017) Comprehensive profiling of metaplastic breast carcinomas reveals frequent overexpression of programmed death-ligand 1. J Clin Pathol 70:255–259. https://doi.org/10.1136/jclinpath-2016-203874
Tray N, Taff J, Singh B et al (2019) Metaplastic breast cancers: genomic profiling, mutational burden and tumor-infiltrating lymphocytes. The Breast 44:29–32. https://doi.org/10.1016/j.breast.2018.12.010
González-Martínez S, Pérez-Mies B, Carretero-Barrio I et al (2020) Molecular features of metaplastic breast carcinoma: an infrequent subtype of triple negative breast carcinoma. Cancers 12:1832. https://doi.org/10.3390/cancers12071832
Basho RK, Yam C, Gilcrease M et al (2018) Comparative effectiveness of an mTOR-based systemic therapy regimen in advanced, metaplastic and nonmetaplastic triple-negative breast cancer. Oncologist 23:1300–1309. https://doi.org/10.1634/theoncologist.2017-0498
Coussy F, El Botty R, Lavigne M et al (2020) Combination of PI3K and MEK inhibitors yields durable remission in PDX models of PIK3CA-mutated metaplastic breast cancers. J Hematol Oncol 13:13. https://doi.org/10.1186/s13045-020-0846-y
Kalaw E, Lim M, Kutasovic JR et al (2020) Metaplastic breast cancers frequently express immune checkpoint markers FOXP3 and PD-L1. Br J Cancer 123:1665–1672. https://doi.org/10.1038/s41416-020-01065-3
Grabenstetter A, Jungbluth AA, Frosina D et al (2021) PD-L1 expression in metaplastic breast carcinoma using the PD-L1 SP142 assay and concordance among PD-L1 immunohistochemical assays. Am J Surg Pathol 45:1274–1281. https://doi.org/10.1097/PAS.0000000000001760
Adams S (2017) Dramatic response of metaplastic breast cancer to chemo-immunotherapy. NPJ Breast Cancer 3:8. https://doi.org/10.1038/s41523-017-0011-0
Adams S, Othus M, Patel SP et al (2022) A multicenter phase II trial of ipilimumab and nivolumab in unresectable or metastatic metaplastic breast cancer: cohort 36 of dual anti–CTLA-4 and anti–PD-1 blockade in rare tumors (DART, SWOG S1609). Clin Cancer Res 28:271–278. https://doi.org/10.1158/1078-0432.CCR-21-2182
da Silva EM, Selenica P, Vahdatinia M et al (2021) TERT promoter hotspot mutations and gene amplification in metaplastic breast cancer. NPJ Breast Cancer 7:43. https://doi.org/10.1038/s41523-021-00250-8
Dave B, Gonzalez DD, Liu Z-B et al (2017) Role of RPL39 in metaplastic breast cancer. JNCI J Natl Cancer Inst 109:292. https://doi.org/10.1093/jnci/djw292
Stradella A, Gargallo P, Cejuela M et al (2022) Genomic characterization and tumor evolution in paired samples of metaplastic breast carcinoma. Mod Pathol. https://doi.org/10.1038/s41379-022-01017-7
Funding
This study was supported by the Tianjin Science and Technology Committee (18ZXXYSY00070).
Author information
Authors and Affiliations
Contributions
Conceived and designed of the study: YS. Performed patients’ follow-ups, screened and analyzed the data and wrote this manuscript: JH. Contributed data: RL. Provided critical reviews and suggestions on revision: WZ, YJ and ZT. All authors read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest are disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, J., Lang, R., Zhao, W. et al. The mixed subtype has a worse prognosis than other histological subtypes: a retrospective analysis of 217 patients with metaplastic breast cancer. Breast Cancer Res Treat 200, 23–36 (2023). https://doi.org/10.1007/s10549-023-06945-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06945-9