Abstract
Purpose
We assessed the systemic treatment choices and outcomes in patients diagnosed with human epidermal growth factor receptor-2-positive (HER2 +) advanced breast cancer (ABC), for the first four lines of systemic therapy and by hormone receptor (HR) status.
Methods
We identified 330 patients diagnosed with HER2 + ABC in 2013–2018 in the Southeast of The Netherlands, of whom 64% with HR + /HER2 + and 36% with HR-/HER2 + disease. Overall survival (OS) from start of therapy was calculated using the Kaplan–Meier method.
Results
In real world, 95% of patients with HR + /HER2 + and 74% of patients with HR-/HER2 + disease received systemic therapy. In HR + /HER2 + disease, use of endocrine, chemo- and HER2-targeted therapy was , respectively, 64%, 46% and 60% in first line, and 39%, 64% and 75% in fourth line. In HR-/HER2 + disease, 91–96% of patients received chemotherapy and 77–91% HER2-targeted therapy, irrespective of line of therapy. In patients with HR + /HER2 + disease, median OS was 34.9 months (95%CI:25.8–44.0) for the first line and 12.8 months (95%CI:10.7–14.9) for the fourth line. In HR-/HER2 + disease, median OS was 39.9 months (95%CI:23.9–55.8) for the first line and 15.2 months (95%CI:10.9–19.5) for the fourth line. For patients treated with first-line pertuzumab, trastuzumab plus chemotherapy, median OS was not reached at 56.0 months in HR + /HER2 + disease and 48.4 months (95%CI:32.6–64.3) in HR-/HER2 + disease.
Conclusion
Survival times for later lines of therapy are surprisingly long and justify the use of multiple lines of systemic therapy in well-selected patients with HER2 + ABC. Our real-world evidence adds valuable observations to the accumulating evidence that within HER2 + ABC, the HR status defines two distinct disease subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of treatment options for advanced breast cancer (ABC) has substantially increased over time, especially in patients with human epidermal growth factor receptor-2-positive (HER2 +) disease. Trastuzumab was introduced as the first HER2-targeted therapy, at the end of the nineties of the previous century [1]. During the past two decades, trastuzumab beyond progression (TBP), lapatinib, pertuzumab, T-DM1, neratinib, trastuzumab-deruxtecan, tucatinib and margetuximab were approved by the FDA and/or EMA [2,3,4,5,6,7,8,9,10]. Until recently, international guidelines recommended that patients with HER2 + ABC are treated with first-line pertuzumab, trastuzumab plus taxane and with second-line T-DM1 regardless of hormone receptor (HR) status [8, 9]. Since 2022, the ASCO guidelines recommend trastuzumab-deruxtecan as preferred second line and tucatinib combined with trastuzumab and capecitabine as third-line treatment option [11]. In the Netherlands, pertuzumab was reimbursed per July 30, 2013, and T-DM1 per June 26, 2014. Access to trastuzumab-deruxtecan and tucatinib is expected soon in the Netherlands, as in many other countries worldwide. In selected patients with HR + /HER2 + disease, endocrine therapy added to trastuzumab or as monotherapy remains an option in patients with low disease burden, long disease-free interval, low performance score, cardiac disease, and personal preference to avoid chemotherapy [12, 13].
Several observational studies have shown that patients diagnosed with HR + /HER2 + disease had a better outcome when compared with patients with HR-/HER2 + disease [14,15,16,17]. Recently, we reported that patients with HR-/HER2 + ABC who were diagnosed after the introduction of pertuzumab and T-DM1 had an improved overall survival (OS) as compared with those diagnosed before introduction, whereas survival remained rather similar in patients with HR + /HER2 + ABC [17]. We hypothesized that this might be related to differences in treatment choices in first and subsequent lines of systemic therapy.
To our knowledge, treatment choices per line of therapy and by HR status have not been reported before. Therefore, we studied, in a real-world setting, the delivered systemic therapies per HR status for the first four lines of therapy, and the accompanying patient and tumour characteristics, progression-free survival (PFS) and OS time. These data provide helpful insights for treatment decisions in the future patients, for reimbursement issues and for the design of clinical trials.
Patients and methods
Southeast Netherlands advanced breast cancer (SONABRE) registry
Data for this study were obtained from the SONABRE Registry (NCT-03577197). This observational cohort study includes all patients diagnosed with de novo or recurrent ABC in the Southeast of the Netherlands. Information is collected by specially trained registration clerks from medical files including patient and tumour characteristics, treatment information in the curative and palliative setting, response to systemic therapy, and date and cause of death. The Medical Research Ethics Committee of Maastricht University Medical Centre approved the Registry (15-4-239).
Patients
In this present study, we selected all patients diagnosed with HER2 + ABC in 2013–2018 from nine hospitals, including one academic, five teaching and three non-teaching hospitals. The last follow-up was collected in 2020 and the data lock was on September first, 2020. HER2 positivity was defined as a positive fluorescence in situ hybridization (FISH) result or an immunohistochemistry score of 3 + . HR (oestrogen/progesterone receptor) positivity was defined as positive nuclear staining of ≥ 10% of one or both receptors by immunohistochemistry. To determine the breast cancer subtype, we used information on HR/HER2 status from a metastatic site. If no biopsy of metastatic disease was available, the receptor status was based on the primary tumour or a prior locoregional recurrence.
Endpoints
We first determined the proportion of patients who received at least one line of palliative systemic therapy and compared their characteristics with patients who received best supportive care only.
Next, we assessed the delivered systemic therapies for the first four lines of therapy with the accompanying patient and tumour characteristics at start of each line of systemic therapy for advanced disease. According to national cancer institute (NCI) criteria [18], a new line of therapy was defined as the introduction of a new systemic agent, with the exception of the introduction of endocrine therapy as maintenance therapy, i.e. in the absence of progression of disease. We estimated the upper and lower limit of the proportion of patients starting a second line to fourth line of therapy, the so-called continuation rate. The lower limit of the continuation rate was defined as the proportion of patients who started a second line to fourth line of therapy during follow-up. Then we determined the proportion of patients who had died before starting a specific line of therapy, thus not being able to continue to a next line of therapy. The upper limit of the continuation rate was then calculated as one minus the proportion of patients who died during a specific line. To account for the time-dependent character of the estimation of the continuation rates, competing risk regression was used considering continuation to a new line of therapy and mortality before continuing to a next of line of therapy (i.e. the attrition rate) as the two ‘competing events’. Of note, in a cohort were all patients are followed up until death, the lower and upper limit of the continuation rate will be equal.
The primary endpoints were the PFS and OS per line of systemic therapy. PFS was calculated as the time from the start of the line of systemic therapy until reported progression of disease or death, whichever occurred first. Patients who stopped treatment (e.g. because of toxicity) but did not switch to a new line of therapy in the absence of progression were followed until progression or death whichever occurred first. Conversely, patients who switched to a next line of therapy in the absence of progression were censored at time of switching. OS was defined as the time from the start of the line of palliative systemic therapy to date of death, or when alive censored at the date of last follow-up.
Statistical analysis
Baseline patient and disease characteristics for the first four lines of therapy were compared using the Mantel–Haenszel test for trend. PFS and OS per line of therapy were assessed using the Kaplan–Meier methodology per line of therapy, stratified by HR status. Outcomes of patient subgroups with less than 10 patients were not analysed. The P-values reported were two-sided and considered statistically significant at a value of ≤ 0.05.
Results
We identified 330 patients diagnosed with HER2 + ABC in 2013–2018, of whom 211 (64%) with HR + /HER2 + disease and 119 (36%) with HR-/HER2 + disease (Fig. 1). The median follow-up time of systemically treated patients was 47 months (95% confidence interval (CI) 42–52), during which 160 (55%) patients had died, and 7 (2%) patients were lost to follow-up due to transfer to a non-participating hospital.
Best supportive care only
Ten (5%) patients with HR + /HER2 + and 31 (26%) patients with HR-/HER2 + disease received best supportive care without systemic therapy; they had a median OS of , respectively, 1.0 months (95% CI 0.2–1.9) and 3.0 months (95% CI 2.4–3.7). Patients with HR + /HER2 + disease receiving best supportive care only were older at ABC diagnosis (median 66 vs. 60 years), had a higher rate of WHO performance status 2 + (67% vs 18%) and had a higher rate of central nervous system metastases (30% vs 7%) compared with those who received systemic therapy (Supplementary Table S1). Similarly, patients with HR-/HER2 + disease receiving best supportive care only were older (median 73 vs. 57 years), had more often cardiovascular comorbidity (48% vs 22%), a higher rate of WHO performance status 2 + (68% vs 11%) and a lower rate of soft tissue metastases (26% vs 56%) when compared with those who received systemic therapy (Supplementary Table S1).
Patient characteristics and outcomes per line of therapy
Among patients who started first-line systemic therapy, an estimated (lower–upper limit) 70–80% of patients with HR + /HER2 + disease started a second line, 51–66% a third line, and 33–54% a fourth line of systemic therapy (Supplementary Figure S1 and Supplementary Table S2). Among HR-/HER2 + patients who started first-line therapy, the estimated continuation rates were 61–78% for second line, 30–61% for third line and 14–50% for fourth line. Patient age, comorbidity (any or cardiovascular), WHO performance status, (neo-)adjuvant systemic therapy use and metastatic-free interval at start of systemic therapy were comparable over the four lines of therapy (Table 1). Though, as expected, the number of metastatic sites increased for each subsequent line of therapy, especially in patients with HR + /HER2 + disease.
In patients with HR + /HER2 + disease, 60% of patients were treated with HER2-targeted therapy in first line, which increased to 75% in fourth line (Fig. 2). In patients with HR-/HER2 + disease, HER2-targeted therapy varied between 77 and 91% in the first four lines of therapy. In general, for the total HER2 + population, once a patient received a HER2-targeted therapy, the next line also contained HER2-targeted therapy in the majority of patients (Supplementary Figure S2). In HR + /HER2 + disease, use of endocrine therapy (with or without HER2-targeted therapy, and including endocrine maintenance therapy after chemotherapy) decreased from 64% in first line to 39% in fourth line, whereas the use of chemotherapy increased from 46% in first line to 64% in fourth line (Fig. 2). In HR-/HER2 + disease, 91–96% of patients received chemotherapy-based therapy, irrespective of line of therapy.
Treatment pattern of patients diagnosed with HER2 + ABC, categorized by HR status. ABC advanced breast cancer, CT chemotherapy, ET endocrine therapy, HER2 Human Epidermal growth factor Receptor 2, HER2-TT HER2-targeted therapy, HR hormone receptor. §Proportion of patients with HR + /HER2 + disease treated with endocrine (± HER2-targeted) maintenance therapy per line of therapy: 1st line N = 27 (13%); 2nd line N = 4 (3%); 3rd line N = 0; 4th line N = 2 (4%). *Includes patients (N = 3) treated with endocrine-based therapy with HR + primary breast tumour
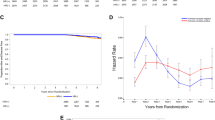
In HR + /HER2 + disease, patients with any first-line systemic therapy (n = 201) had a median first-line PFS of 10.9 months (95% CI 8.6–13.1) and a median OS of 34.9 months (95% CI 25.8–44.0), and with any fourth line of therapy (n = 57), a median fourth-line PFS of 5.6 months (95% CI 3.5–7.6) and a median OS of 12.8 months (95% CI 10.7–14.9) (Fig. 3A and B).
In HR-/HER2 + disease, patients with any first-line systemic therapy (n = 88) had a median first-line PFS of 16.5 months (95% CI 10.6–22.4) and a median OS of 39.9 months (95% CI 23.9–55.8), and with any fourth-line therapy (n = 11) had a median fourth-line PFS of 6.7 months (95% CI 3.1–10.3) and a median OS of 15.2 months (95% CI 10.9–19.5) (Fig. 3C and D).
First-line treatment patterns and outcomes
In patients systemically treated for HR + /HER2 + disease, the two most common first-line therapies were endocrine monotherapy (n = 72, 36%) and pertuzumab, trastuzumab plus chemotherapy (n = 59, 29%) (Fig. 2A, Table 2). Patients treated with first-line endocrine monotherapy had a median first-line PFS of 7.6 months (95% CI 4.9–10.3) and a median OS of 29.5 months (95% CI 19.0–40.1) (Fig. 4). Those treated with first-line pertuzumab, trastuzumab plus chemotherapy had a median first-line PFS of 21.6 months (95% CI 13.1–30.1) and median OS was not reached at 56.0 months. Patients treated with endocrine monotherapy compared with those treated with pertuzumab, trastuzumab plus chemotherapy were older, had more often comorbidity and a worse performance status, a longer metastatic-free interval and more often bone only disease (Table 2).
Progression-free survival (PFS) and overall survival (OS) of the most common first-line treatment regimens*, categorized by HR status. CT chemotherapy, ET endocrine therapy, HER2 Human Epidermal growth factor Receptor 2, HER2-TT HER2-targeted therapy, HR hormone receptor, P pertuzumab, T trastuzumab. *Note, not to be directly compared because of risk of confounding by indication. See also Supplement Table S2 for the outcomes of all types of treatment regimes
Among patients systemically treated for HR-/HER2 + disease, the two most common first-line therapies were pertuzumab, trastuzumab plus chemotherapy (n = 64, 73%) and trastuzumab plus chemotherapy without pertuzumab (n = 14, 16%) (Fig. 2B, Table 2). Patients treated with first-line pertuzumab, trastuzumab plus chemotherapy had a median PFS of 21.7 months (95% CI 11.4–31.9) and a median OS of 48.4 months (95% CI 32.6–64.3) (Fig. 4). Patients treated with first-line trastuzumab plus chemotherapy had a median PFS of 12.8 (95% CI 8.9–16.7) and a median OS of 15.6 (95% CI 0.0–56.5) months, respectively (Fig. 4). Patients treated with trastuzumab plus chemotherapy were older, had a worse performance status and less often de novo metastases when compared with patients treated with pertuzumab, trastuzumab plus chemotherapy (Table 2).
Discussion
Real-world data support daily clinical decision-making and future study designs, in addition to data from randomized controlled trials. It is therefore important to gain insight into the characteristics of patients we treat in real-life, the (number and type of) lines of therapy they receive, and the outcomes of delivered treatment per line of therapy and per HR status. We collected the data of patients diagnosed with HER2 + ABC in the Southeast of The Netherlands in the years 2013–2018, a time frame in which pertuzumab and T-DM1 became available. We showed that in real world, 5% of patients with HR + /HER2 + disease and 26% of patients with HR-/HER2 + disease received best supportive care without systemic therapy. These patients had poor baseline characteristics and a very poor outcome. With the exception of an increase in the number of metastatic sites for later lines of therapy, patient characteristics at start of therapy were largely independent of line of therapy. As a result of patient selection, the proportion of patients continuing to a next line of therapy gradually declined, whereby the majority continued on HER2-targeted therapy once started. This was the case irrespective of the HR status. Chemotherapy use was significantly lower in patients treated for HR + /HER2 + versus HR-/HER2 + ABC, in all lines of therapy. Use of endocrine-based therapy was common in patients with HR + /HER2 + disease. Median survival times for later lines of therapy were surprisingly long, justifying the use of multiple lines of systemic therapy in well-selected patients with HER2 + ABC.
We observed in our study that only a small proportion of patients with HR + /HER2 + ABC received best supportive care only as compared with a much larger proportion of patients with HR-/HER2 + disease. This may indicate that some patients with HR + /HER2 + disease were fit enough for endocrine therapy but not for chemotherapy plus HER2-targeted therapy. In other patients, endocrine therapy without trastuzumab may have been chosen because trastuzumab use would have obstructed reimbursement of pertuzumab use in the next line of therapy [19, 20]. For patients with HR + /HER2 + ABC who are fit enough for chemotherapy, first-line pertuzumab, trastuzumab plus chemotherapy, followed by maintenance endocrine and trastuzumab therapy is nowadays considered the best treatment option [11].
Only few other investigators studied the use of multiple lines of systemic therapy in patients with HER2 + ABC [21,22,23]. Consistent with their observations, we also found that the majority of patients received HER2-targeted therapy in first and subsequent lines of therapy, illustrating the high use of trastuzumab beyond progression. In addition, we showed that in daily practice, 36% of patients with HR + /HER2 + disease received initial endocrine therapy as monotherapy and 15% received endocrine therapy combined with HER2-targeted therapy. This high use of endocrine monotherapy was also observed in two multicentre studies in the United States of America (SystHERs and Flatiron: 59% and 24% in first line) [21,22,23]. A lower number was reported for a European retrospective cross-sectional study, where only 1% of registered patients were treated with endocrine monotherapy, potentially due to patient selection [21]. Noteworthy, we observed that a large proportion of patients with HR + /HER2 + disease received also endocrine therapy during later lines of therapy.
Considering patients treated with any systemic therapy, we observed a median OS of 34.9 months in HR + /HER2 + and a median OS of 39.9 months in HR-/HER2 + disease. When only looking at patients who were treated with first-line pertuzumab, trastuzumab plus chemotherapy, we noted a comparable median PFS (i.e. respectively, 21.6 and 21.7 months), whereas median OS differed (i.e. respectively, not reached at 56 months and 48.4 months). The PFS data confirm that pertuzumab is comparably effective in HR + /HER2 + and HR-/HER2 + disease. The better OS outcome in HR + /HER2 + disease may be the result of different biology and/or by the additional availability of endocrine (maintenance) therapy. It also stresses the impact of patient selection in daily clinical practice. If we select only the fittest patients for the more toxic and more expensive treatments, we offer more cost-effective care. In a time frame where health care costs are continually at the rise and the number of available health care professionals is in decline, we need to consider careful patient selection. Of note, the outcomes of patients selected for pertuzumab in our cohort are in line with the results found in the registration CLEOPATRA trial [10]. We therefore conclude that our patient selection for pertuzumab-based therapy was appropriate.
Preclinical and clinical studies have suggested that the use of dual blockade of the oestrogen receptor (ER) and HER2 receptor for patients with HR + /HER2 + disease prevents relative therapy resistance [24,25,26,27,28]. The use of HER2-targeted therapy in HR + /HER2 + disease is associated with an up-regulation of ER expression and subsequently decreasing HER2 signal activity. Vice versa, the use of endocrine therapy is associated with an increased HER2 signal activity potentially leading to a downregulation of both ER and progesterone receptor (PR) expression. As a result, blocking only one receptor leads to resistance and reduced treatment efficacy. One could argue that patients treated with endocrine therapy alone in second line and beyond missed out on important treatment benefits of adding HER2 blockage. Recently, the MonarcHER phase II trial reported that CDK4/6 inhibitor plus endocrine therapy in combination with trastuzumab was superior to chemotherapy plus trastuzumab in patients who had previously received at least two lines of HER2-targeted therapies for ABC, whereas CDK4/6 inhibitor plus trastuzumab without endocrine therapy was comparable to chemotherapy plus trastuzumab [29]. More studies need to investigate the role of combining dual endocrine targeted and dual HER2-targeted therapy in patients with HR + /HER2 + disease.
The strength of our prospective cohort study lies in the inclusion of all patients diagnosed with HER2 + ABC from a recent five-year inclusion period showing a more current treatment pattern over multiple lines of therapy with a significant follow-up time. We were also able to identify patients not systemically treated. These patients are generally not included in observational studies. The data were manually screened and collected by specially trained registration clerks, which contributed to the high quality of the data. Inherent to the observational character of the study, effectiveness comparison between lines and type of therapy was not possible due to the risk of confounding by indication affecting treatment decisions and prognosis. The reasoning behind chosen treatment options was generally not documented in the medical files. In addition, the evaluation of progressive disease was based on the physician’s assessment which did not always include imaging. Lastly, the number of patients with HR-/HER2 + disease receiving a fourth-line therapy (n = 11) is limited, making it difficult to reliably interpret the results. Yet, it is an important addition to the evolving evidence that HR + /HER2 + and HR-/HER2 + ABC are to be considered as two distinct diseases. These study findings provide important mirror information for the treating physicians, and it is required as model input for the design of new clinical trials and the reimbursement, implementation and evaluation of new systemic drugs.
In conclusion, we studied the real-life treatment choices and outcomes of patients diagnosed in 2013–2018 with HER2-positive ABC. We showed that patients with maintenance of a good performance status received multiple lines of (HER2-targeted) therapies with even in the fourth line, a median overall survival of more than one year, which is a reassuring observation. Endocrine monotherapy use was in line with guideline recommendations and associated with older age and poorer performance status. In patients with HR + /HER2 + disease, endocrine-based therapy was often given over the subsequent lines of therapy. In the future, chemotherapy-free regimens consisting of multiple targeted therapies are expected. The distinction by HR status within the HER2 + ABC subtype will become increasingly important.
Data Availability
Data are available upon request (vcg.tjan.heijnen@mumc.nl).
References
Slamon DJ et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344(11):783–792
von Minckwitz G et al (2009) Trastuzumab beyond progression in human epidermal growth factor receptor 2-positive advanced breast cancer: a german breast group 26/breast international group 03–05 study. J Clin Oncol 27(12):1999–2006
Blackwell KL et al (2012) Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 Study. J Clin Oncol 30(21):2585–2592
Martin M et al (2013) A phase two randomised trial of neratinib monotherapy versus lapatinib plus capecitabine combination therapy in patients with HER2+ advanced breast cancer. Eur J Cancer 49(18):3763–3772
(EMA), E.M.A., Perjeta (pertuzumab) autorisation details. https://www.ema.europa.eu/, 2013.
Verma S et al (2012) Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med 367(19):1783–1791
AGENCY, E.M., Kadcyla (Trastuzumab emtansine). www.ema.europa.eu, 2013.
Modi S et al (2019) Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med 382(7):610–621
Murthy RK et al (2019) Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med 382(7):597–609
Swain SM et al (2020) Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. Lancet Oncol 21(4):519–530
Giordano SH et al (2022) Systemic therapy for advanced human epidermal growth factor receptor 2–positive breast cancer: ASCO guideline update. J Clin Oncol 40(23):2612–2635
Cardoso, F., et al., 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5)†. Annals of Oncology, 2020.
Gennari A et al (2021) ESMO clinical practice guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann Oncol 32(12):1475–1495
Bonotto M et al (2014) Measures of outcome in metastatic breast cancer: insights from a real-world scenario. Oncologist 19(6):608–615
Tripathy D et al (2013) First-line treatment patterns and clinical outcomes in patients with HER2-positive and hormone receptor-positive metastatic breast cancer from registHER. Oncologist 18(5):501–510
Statler AB et al (2019) Real-world treatment patterns and outcomes in HR+/HER2+ metastatic breast cancer patients: a national cancer database analysis. Sci Rep 9(1):18126
Khava Ibragimova IE et al (2021) Survival before and after the introduction of pertuzumab and T-DM1 in HER2-positive advanced breast cancer, a study of the SONABRE Registry. Breast Cancer Res Treatment 188(2):571–581
Giordano SH, Elias AD, Gradishar WJ (2018) NCCN Guidelines Updates: Breast Cancer. J Natl Compr Canc Netw 16(5S):605–610
(FDA), F.a.D.A., PERJETA (pertuzumab) Label. 2012.
(EMA), E.M.A., Perjeta (pertuzumab) authorisation. 2013.
Colomer R et al (2018) Real-world treatment in patients with HER2+ metastatic breast cancer : treatment decisions in HER2+ mBC. Breast Cancer Res Treat 168(1):197–205
Cobleigh M et al (2020) Baseline characteristics, treatment patterns, and outcomes in patients with HER2-positive metastatic breast cancer by hormone receptor status from SystHERs. Clin Cancer Res 26(5):1105–1113
Collins J et al (2021) Abstract PS7-82: A real-world evidence study of treatment patterns among patients with HER2-positive metastatic breast cancer. Cancer Res 81((4_Supplement)):PS7-82
Konecny G et al (2003) Quantitative association between HER-2/neu and steroid hormone receptors in hormone receptor-positive primary breast cancer. J Natl Cancer Inst 95(2):142–153
Vaz-Luis I et al (2012) Impact of hormone receptor status on patterns of recurrence and clinical outcomes among patients with human epidermal growth factor-2-positive breast cancer in the national comprehensive cancer network: a prospective cohort study. Breast Cancer Res 14(5):R129
Wang Y et al (2015) Hormone receptor status predicts the clinical outcome of human epidermal growth factor 2-positive metastatic breast cancer patients receiving trastuzumab therapy: a multicenter retrospective study. Onco Targets Ther 8:3337–3348
Schettini F et al (2016) Hormone receptor/human epidermal growth factor receptor 2-positive breast cancer: where we are now and where we are going. Cancer Treat Rev 46:20–26
Giuliano M, Trivedi MV, Schiff R (2013) Bidirectional crosstalk between the estrogen receptor and human epidermal growth factor receptor 2 signaling pathways in breast cancer: molecular basis and clinical implications. Breast Care (Basel) 8(4):256–262
Tolaney SM et al (2020) Abemaciclib plus trastuzumab with or without fulvestrant versus trastuzumab plus standard-of-care chemotherapy in women with hormone receptor-positive, HER2-positive advanced breast cancer (monarcHER): a randomised, open-label, phase 2 trial. Lancet Oncol 21(6):763–775
Acknowledgements
We thank our SONABRE registrars of the department of Medical Oncology of Maastricht University Medical Centre (MUMC +), Maastricht, the Netherlands.
Funding
This work was supported by the Netherlands Organization for Health Research and Development (ZonMw: 80-82500-98-8003), Novartis BV, Roche, Pfizer, Eli Lilly and Daiichi-Sankyo.
Author information
Authors and Affiliations
Contributions
KIEI, SMEG and VCGT-H contributed to study concepts, study design and data analysis and interpretation. FE, JBH, JT, BEPJV, KNAA, MWD, MJAEP, NAJBP, LvdW, NJAT–D and KIEI contributed to data acquisition. SMEG contributed to quality control of data and algorithms and statistical analysis. . KIEI and SMEG contributed to manuscript preparation. KIEI, SMEG, FE, JBH, JT, BEPJV, KNAA, MWD, MJAEP, NAJBP, LvdW, NJAT – D, IJHV and VCGT-H contributed to manuscript editing and Manuscript review. The International Committee of Medical Journal Editors (ICMJE) criteria for authorship have been met, and we declare that the authors of this manuscript all contributed to the writing of this article.
Corresponding author
Ethics declarations
Conflict of interest
Khava I.E. Ibragimova Financial interests: Grants from Novartis BV, Roche, Pfizer, Eli Lilly, Daiichi-Sankyo. Marissa Meegdes Financial interests: Grants from Novartis BV, Roche, Pfizer, Eli Lilly, Daiichi-Sankyo. Sandra M.E. Geurts Financial interests: Grants from Novartis BV, Roche, Pfizer, Eli Lilly, Daiichi-Sankyo, Gilead, Grants and personal fees from AstraZeneca. Nathalie J.A. Teeuwen-Dedroog Financial interests: Grants from Novartis BV, Roche, Pfizer, Eli Lilly, Daiichi-Sankyo. Ingeborg Vriens Financial interests: Grants from AstraZeneca and Pfizer. Vivianne C.G. Tjan-Heijnen Financial interests: Grants and personal fees from Roche, grants and personal fees from Novartis, grants and personal fees from Pfizer, grants and personal fees from Lilly, grants and personal fees from AstraZeneca, grants from Daiichi-Sankyo and grants from Gilead. All remaining authors have no relevant financial or non-financial interests to disclose. Signed by first author Khava Ibragimova on behalf of all authors.
Ethical approval
The Registry was approved and the need for informed consent waived by the Medical Research Ethics Committee of Maastricht University Medical Center (METC 15-4-239).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ibragimova, K.I.E., Geurts, S.M.E., Meegdes, M. et al. Outcomes for the first four lines of therapy in patients with HER2-positive advanced breast cancer: results from the SONABRE registry. Breast Cancer Res Treat 198, 239–251 (2023). https://doi.org/10.1007/s10549-022-06832-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06832-9