Abstract
Purpose
Immediate lymphatic reconstruction (ILR) at the time of axillary lymph node dissection (ALND) can reduce the incidence of lymphedema in patients with breast cancer. The oncologic safety of ILR is unknown and has not been reported. The purpose of this study was to evaluate if ILR is associated with increased breast cancer recurrence rates.
Methods
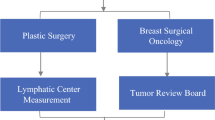
Patients with breast cancer who underwent ALND with ILR from September 2016 to December 2020 were identified from a prospective institutional database. Patient demographics, tumor characteristics, and operative details were recorded. Follow-up included the development of local recurrence as well as distant metastasis. Oncologic outcomes were analyzed.
Results
A total of 137 patients underwent ALND with ILR. At cancer presentation, 122 patients (89%) had clinically node positive primary breast cancer, 10 patients (7.3%) had recurrent breast cancer involving the axillary lymph nodes, 3 patients (2.2%) had recurrent breast cancer involving both the breast and axillary nodes, and 2 patients (1.5%) presented with axillary disease/occult breast cancer. For surgical management, 103 patients (75.2%) underwent a mastectomy, 22 patients (16%) underwent lumpectomy and 12 patients (8.8%) had axillary surgery only. The ALND procedure, yielded a median of 15 lymph nodes pathologically identified (range 3–41).
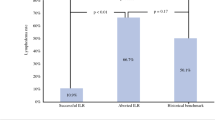
At a median follow-up of 32.9 months (range 6–63 months), 17 patients (12.4%) developed a local (n = 1) or distant recurrence (n = 16), however, no axillary recurrences were identified.
Conclusion
Immediate lymphatic reconstruction in patients with breast cancer undergoing ALND is not associated with short term axillary recurrence and appears oncologically safe.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the personal health information contained within. The data are available from the corresponding author upon request.
Abbreviations
- ILR :
-
Immediate lymphatic reconstruction
- ALND :
-
Axillary lymph node dissection
- SLNB :
-
Sentinel lymph node biopsy
- LVB :
-
Lymphovenous bypass
- ARM :
-
Axillary reverse mapping
- LYMPHA :
-
Lymphatic microsurgical preventative healing approach
- pCR :
-
Pathologic complete response
- NAC :
-
Neoadjuvant chemotherapy
- RCB :
-
Residual cancer burden
References
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515
Gillespie TC, Sayegh HE, Brunelle CL, Daniell KM, Taghian AG (2018) Breast cancer-related lymphedema: risk factors, precautionary measures, and treatments. Gland Surg 7(4):379–403
McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP et al (2008) Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol 26(32):5213–5219
Johnson AR, Fleishman A, Granoff MD, Shillue K, Houlihan MJ, Sharma R et al (2021) Evaluating the impact of immediate lymphatic reconstruction for the surgical prevention of lymphedema. Plast Reconstr Surg 147(3):373e-e381
Fallahian F, Tadisina KK, Xu KY (2022) Efficacy of microsurgical treatment of primary lymphedema. Ann Plast Surg 88(2):195–199
Chang DW, Suami H, Skoracki R (2013) A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast Reconstr Surg 132(5):1305–1314
Boccardo F, Casabona F, de Cian F, Friedman D, Villa G, Bogliolo S et al (2009) Lymphedema microsurgical preventive healing approach: a new technique for primary prevention of arm lymphedema after mastectomy. Ann Surg Oncol 16(3):703–708
Boccardo F, Casabona F, DeCian F, Friedman D, Murelli F, Puglisi M et al (2014) Lymphatic microsurgical preventing healing approach (LYMPHA) for primary surgical prevention of breast cancer-related lymphedema: over 4 years follow-up. Microsurgery 34(6):421–424
Schwarz GS, Grobmyer SR, Djohan RS, Cakmakoglu C, Bernard SL, Radford D et al (2019) Axillary reverse mapping and lymphaticovenous bypass: lymphedema prevention through enhanced lymphatic visualization and restoration of flow. J Surg Oncol 120(2):160–7
Hahamoff M, Gupta N, Munoz D, Lee BT, Clevenger P, Shaw C et al (2019) A lymphedema surveillance program for breast cancer patients reveals the promise of surgical prevention. J Surg Res 244:604–611
Feldman S, Bansil H, Ascherman J, Grant R, Borden B, Henderson P et al (2015) Single institution experience with lymphatic microsurgical preventive healing approach (LYMPHA) for the primary prevention of lymphedema. Ann Surg Oncol 22(10):3296–3301
Ozmen T, Lazaro M, Zhou Y, Vinyard A, Avisar E (2019) Evaluation of simplified lymphatic microsurgical preventing healing approach (S-LYMPHA) for the prevention of breast cancer-related clinical lymphedema after axillary lymph node dissection. Ann Surg 270(6):1156–1160
Coriddi M, Dayan J, Mehrara B (2020) Nomenclature in lymphedema surgery. Plast Reconstr Surg 146(3):385e-e386
Bedrosian I, Babiera GV, Mittendorf EA, Kuerer HM, Pantoja L, Hunt KK et al (2010) A phase I study to assess the feasibility and oncologic safety of axillary reverse mapping in breast cancer patients. Cancer 116(11):2543–8
Liu S, Wang N, Gao P, Liu P, Yang H, Xie F et al (2020) Using the axillary reverse mapping technique to screen breast cancer patients with a high risk of lymphedema. World J Surg Oncol 18(1):118
Schunemann E, Dória MT, Silvestre JBCH, Gasperin P, Cavalcanti TCS, Budel VM (2014) Prospective study evaluating oncological safety of axillary reverse mapping. Ann Surg Oncol 21(7):2197–2202
Gennaro M, Listorti C, Mariani L, Maccauro M, Bianchi G, Capri G et al (2021) Oncological safety of selective axillary dissection after axillary reverse mapping in node-positive breast cancer. Eur J Surg Oncol 47(7):1606–1610
Ochoa D, Korourian S, Boneti C, Adkins L, Badgwell B, Klimberg VS (2014) Axillary reverse mapping: five-year experience. Surgery 156(5):1261–1268
Abdelhamid MI, Bari AA, Farid MI, Nour H (2020) Evaluation of axillary reverse mapping (ARM) in clinically axillary node negative breast cancer patients - randomised controlled trial. Int J Surg 75:174–178
Shaffer K, Cakmakoglu C, Schwarz GS, ElSherif A, Al-Hilli Z, Djohan R et al (2020) Lymphedema prevention surgery: improved operating efficiency over time. Ann Surg Oncol 27(12):4695–4701
Boneti C, Korourian S, Bland K, Cox K, Adkins LL, Henry-Tillman RS et al (2008) Axillary reverse mapping: mapping and preserving arm lymphatics may be important in preventing lymphedema during sentinel lymph node biopsy. J Am Coll Surg 206(5):1038–42 (discussion 1042-4)
Nos C, Kaufmann G, Clough KB, Collignon MA, Zerbib E, Cusumano P et al (2008) Combined axillary reverse mapping (ARM) technique for breast cancer patients requiring axillary dissection. Ann Surg Oncol 15(9):2550–2555
Thompson M, Korourian S, Henry-Tillman R, Adkins L, Mumford S, Westbrook KC et al (2007) Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol 14(6):1890–1895
McBride A, Allen P, Woodward W, Kim M, Kuerer HM, Drinka EK et al (2014) Locoregional recurrence risk for patients with T1,2 breast cancer with 1–3 positive lymph nodes treated with mastectomy and systemic treatment. Int J Radiat Oncol*Biol*Phys 89(2):392–8
Castaneda CA, Rebaza P, Castillo M, Gomez HL, de La Cruz M, Calderon G et al (2018) Critical review of axillary recurrence in early breast cancer. Crit Rev Oncol Hematol 129:146–152
Smidt ML, Janssen CMM, Kuster DM, Bruggink EDM, Strobbe LJA (2005) Axillary recurrence after a negative sentinel node biopsy for breast cancer: incidence and clinical significance. Ann Surg Oncol 12(1):29–33
van der Ploeg IMC, Nieweg OE, van Rijk MC, Valdés Olmos RA, Kroon BBR (2008) Axillary recurrence after a tumour-negative sentinel node biopsy in breast cancer patients: a systematic review and meta-analysis of the literature. Eur J Surg Oncol 34(12):1277–1284
Houvenaeghel G, Classe JM, Garbay JR, Giard S, Cohen M, Faure C et al (2016) Survival impact and predictive factors of axillary recurrence after sentinel biopsy. Eur J Cancer 58:73–82
Wangchinda P, Ithimakin S (2016) Factors that predict recurrence later than 5 years after initial treatment in operable breast cancer. World J Surg Oncol 14(1):223
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P et al (2017) 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. NEJM 377(19):1836–1846
Colleoni M, Sun Z, Price KN, Karlsson P, Forbes JF, Thürlimann B et al (2016) Annual hazard rates of recurrence for breast cancer during 24 years of follow-up: results from the international breast cancer study group trials I to V. J Clin Oncol 34(9):927–935
Colzani E, Johansson AL, Liljegren A, Foukakis T, Clements M, Adolfsson J et al (2014) Time-dependent risk of developing distant metastasis in breast cancer patients according to treatment, age and tumour characteristics. Br J Cancer 110(5):1378–84
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HG, AE, SV, CC and ZAH. The first draft of the manuscript was written by HG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Author Stephanie Valente, DO is a speaker/consultant/advisory board member for Impedimed, Pacira, AxoGen, Merit. The remaining authors have no conflicts of interest. The corresponding author has signed the disclosure form and attached it with the manuscript stating there is no conflict of interest. Separate conflict of interest forms from remaining authors can be uploaded if needed.
Ethical approval
This study received IRB approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guzzo, H.M., Valente, S.A., Schwarz, G.S. et al. Oncologic safety of axillary lymph node dissection with immediate lymphatic reconstruction. Breast Cancer Res Treat 196, 657–664 (2022). https://doi.org/10.1007/s10549-022-06758-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06758-2