Abstract
Purpose
When Core Needle Biopsy (CNB) demonstrates Atypical Ductal Hyperplasia (ADH), Flat Epithelial Atypia (FEA), Intraductal Papilloma (IDP), or Radial Scar/Complex Sclerosing Lesion (RS), excisional biopsy (EB) is often performed to rule out underlying malignancy with upstage rates (UR) ranging between 1 and 20%. The COVID-19 pandemic led to delayed EB for many patients. We sought to evaluate whether this delay was associated with higher UR.
Methods
We performed a retrospective analysis of women who underwent CNB and then EB for ADH, FEA, IDP, or RS between 2017 and 2021 using an IRB-approved repository. UR was evaluated by days between CNB and EB.
Results
473 patients met inclusion. 55 were upstaged to cancer (11.6%). 178 patients had pure ADH on CNB and 37 were upstaged (20.8%). 50 patients had pure FEA and 3 were upstaged (6%). 132 had pure IDP and 7 were upstaged (5.3%). 98 had pure RS and 1 was upstaged (1%). 7/15 (46.7%) had a combination of diagnoses or diagnosis with palpable mass and were upstaged.
Days between CNB and EB were < 60 for 275 patients (58.1%), 60–90 for 108 (22.8%), 91–120 for 43 (9.1%), and > 120 for 47 (9.9%). There was no significant difference in UR (10.9% for < 60, 14.8% for 60–90, 7% for 90–120, and 12.8% for > 120, p = 0.54). UR for ADH was clinically increased after 60 days (27.8 vs. 17.5%), but this did not reach statistical significance (p = 0.1).
Conclusion
Surgical delay was not associated with an increased UR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When Core Needle Biopsy (CNB) demonstrates Atypical Ductal Hyperplasia (ADH), Flat Epithelial Atypia (FEA), Intraductal Papilloma (IDP), or Radial Scar/Complex Sclerosing Lesion (RS), excisional biopsy (EB) is often performed to rule out an associated, underlying malignancy that may have been missed by the biopsy needle. The rate of upstage, or the chance of finding malignancy during EB, varies by type of lesion and size of core biopsy device used. ADH, for example, has the highest UR of up to 56% [1,2,3,4,5,6]. FEA and IDP fall somewhere in the middle, with UR between 0 and 21% [1, 7,8,9,10,11] and 0–33%, respectively [12, 13]. RS tends to have the lowest UR 0–16% [14,15,16,17].
There are data to support that the atypical ductal cells of ADH are non-obligate precursors to malignancy and occupy a position in the multistep sequence of breast carcinogenesis [18]. Many even consider ADH as a precursor of ductal carcinoma in situ (DCIS) [19, 20]. However, EB remains a diagnostic and not preventative procedure because of the probability of adjacent cancer and the unclear association between FEA, IDP, and RS and future cancer development.
Prior to the COVID-19 pandemic, EB was routinely completed within 60 days of the surgical consultation at our tertiary breast center. The pandemic resulted in delays for many of these patients. Because treatment delays are associated with lower overall and disease-specific survival for patients with a breast cancer diagnosis, [21] the delay in diagnosing these malignancies by postponing EB is relevant to patient outcomes. While prior studies have reported individual factors association with upstage for the individual lesions, [3, 13, 22,23,24,25,26,27] few have evaluated the potential association with surgical delay.
Our objective is to look both at ADH and the other lesions associated with upstage to determine whether an increased amount of time between CNB and EB increases the risk for discovering malignancy. We hypothesize that surgical delay will be associated with higher UR for ADH, but not for FEA, RS, or IDP.
Methods
We performed an IRB reviewed and exempted retrospective analysis of women age 18 or older who underwent CNB and then EB between January 1, 2017 and January 1, 2021 for ADH, FEA, IDP, or RS. Patients were identified using an IRB-approved prospective institutional breast disease patient repository stored on REDCap (grant number UL1TR002544). This repository enrolls all patients who meet with one the breast surgeons at our institution. Patients who did not have a diagnosis of ADH, FEA, IDP, or RS, such as those with only unspecified or lobular atypia, and patients whose results were felt to be discordant were excluded. Patient characteristics were collected from the repository or the medical record and included race/ethnicity, personal or family history of cancer, and personal history of a high-risk genetic mutations. Imaging findings that prompted the CNB and pathologies were also evaluated. For CNB, needle gauge and type ranged from a 9-gauge vacuum-assisted device used for stereotactic and MRI guided biopsy to 14-gauge spring-loaded device for ultrasound-guided biopsy. All pathological findings of ADH, FEA, RS, or IDP on CNB-triggered automatic surgical referral, except for microscopic, incidental IDP or RS which is reported to be completely removed by CNB. At our institution, our pathologists report each unequivocal lesion that is present in the CNB specimen. For example, if ADH and FEA are independently identified in a specimen, both are reported. Surgery was performed at one of the three primary or satellite facilities affiliated with our tertiary breast center.
The rate of upstage to malignancy was evaluated and then compared by time between CNB and EB in two ways. First, we tested a dichotomized interval of ≤ 60 vs. > 60 days between CNB and EB because 60 days was felt to be a reasonable time to undergo EB and hypothesized that most patients would range within this period. Second, we evaluated number of days as a categorical variable using < 60, 60 to < 90, 90–120, and > 120. We used > 120 days as a cut-off because we hypothesized greater delays to be unlikely. These increments were similar those previously used in describing the impact of treatment delays for breast cancer patients [21].
Continuous variables were reported using means, standard deviations, medians, and interquartile range. Categorical variables were reported using frequencies and percentages. ANOVA was used to compare the amount of days between CNB and EB, while chi-square test was used to compare the frequency of outcomes. Statistical significance was set at an alpha of 0.05. Data were analyzed using g STATA 17 (StataCorp, College Station, TX).
Results
We identified 501 patients who underwent CNB followed by EB. 28 were excluded for not meeting the inclusion criteria: 15 had a presenting diagnosis of lobular neoplasia (atypical lobular hyperplasia or lobular carcinoma in situ) or other unspecified atypia and 13 had their CNB outside the specified time period. As a result, a total of 473 patients were included for analysis.
Demographics
The mean age was 54.9 years and the median age was 53.4. The mean number of days between CNB and EB was 72.5 and the median was 52. 26 patients (5.5%) had a personal history of breast cancer. 4 (0.8%) had a BRCA 1 or 2 mutation. 76 (16.5%) had a first-degree relative with breast or ovarian cancer (Table 1).
Upstage
55 patients were upstaged to cancer (11.6% of the entire cohort). Patients who upstaged were older (mean age 57.7 vs. 54.9 years, p = 0.04, median 56.2 vs. 53.3), but there were no other significant demographic or patient characteristic differences. There was no difference in UR based on the characteristics on mammography that prompted biopsy (calcifications, architectural distortion, asymmetry, or mass, p = 0.11).
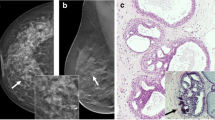
39 of the 55 upstages (70.9%) were to DCIS, 6 (10.9%) to invasive ductal carcinoma (IDC), 3 (5.5%) to invasive lobular carcinoma (ILC), and 1 (1.8%) to pleomorphic lobular carcinoma in situ (pLCIS) (Fig. 1). All patients upstaged to invasive ductal or lobular carcinoma had T1 tumors, and none had clinically or pathologically positive lymph nodes or metastatic disease.
Breakdown by lesion type
178 patients were found to have pure ADH on CNB; 37 of these were upstaged to malignancy (20.8% upstage rate). 50 patients were found to have pure FEA on CNB; 3 were upstaged (6%). 132 patients were found to have pure IDP; 7 were upstaged (5.3%). 98 patients were found to have pure RS and 1 was upstaged to malignancy (1%) (Fig. 2).
15 patients had combination diagnoses (CD) or a diagnosis associated with a palpable mass. 6/14 (42.9%) of patients with CD were upstaged and one patient who had ADH associated with a palpable mass and was upstaged (Table 2).
Timing
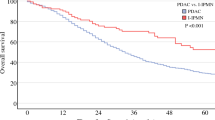
198/473 patients (41.9%) experienced an elapse of 60 or more days between CNB and EB. The pandemic accounted for 28/198 of these delays (14.1%). The time between CNB and SE was less than 60 days for 275 patients (58.1%), between 60 and 89 days for 108 (22.8%), between 90 and 120 days for 43 (9.1%), and more than 120 days for 47 (9.9%). There was no significant difference in the rate of upstage between the groups (10.9% for < 60 days, 14.8% for 60–89 days, 7% for 90–120 days, and 12.8% for > 120 days, p = 0.54). Additionally, when the time period was dichotomized into ≤ 60 vs. > 60 days, there was no difference (p = 0.43, Tables 3 and 4).
Five patients (1.1%) waited more than 1 year between CNB and SE and none were upstaged.
For ADH specifically (including 186 patients with both pure and mixed ADH), 114 (61.3%) underwent SE in 60 days and 72 (38.7%) in greater than 60 days. There was no difference in upstage between groups (18.2% for < 60 days, 29.5% for 60–89, 11.8% for 90–120, and 33.3% for > 120, p = 0.2). As a dichotomized variable, we found that the patients who required greater than 60 days between CNB and SE seemed to have a clinically meaningful difference in the rate of upstage (27.8 vs. 17.5%), but this did not reach statistical significance (p = 0.10).
There was no difference in the type of upstage between the dichotomized or categorical time intervals (Table 5).
Discussion
Although the management of these benign and atypical lesions is controversial, they are often excised to rule out underlying malignancy that is not detected during CNB [3, 4, 28,29,30,31].
It is believed that ADH is a non-obligate precursor to DCIS [19, 20, 30]. If ADH will eventually progress to DCIS, we questioned when this transformation might occur and if delays in excision presented a higher risk of upstage. There are many scenarios that can delay surgery, but none to date have been as widespread as the COVID-19 pandemic. For many institutions around the world, caring for the surge of hospitalized and critically ill patients necessitated the delay of all non-emergent surgery.
The standard practice at our institution was to offer EB for women diagnosed with these lesions on CNB. Often, surgery occurred within 60 days per institutional protocol and patient preference. The COVID-19 pandemic provided an opportunity to assess the impact of longer time between biopsy and surgical excision on upstage rates. Screening mammography was completely stopped for 83 days. Patients who had been diagnosed with these non-malignant diagnoses before the cessation of elective surgery were unable to undergo excision until at least three months later. Luckily, we found that delay in EB was not associated with upstage.
One interesting finding from this study was that women with a combination of diagnoses (CD) had a noticeably high upstage rate. Although the management of CD has yet to be clearly defined, most authors agree that combinations pose a higher risk for upstage. In some studies, concurrent ADH with IDP was associated with a higher rate of upstage, [32] although others found it was not [33]. The presence of additional high-risk lesions with RS, such as atypical neoplasia, have been found to have higher UR [34,35,36]. This was contradicted by other studies which demonstrated that even with the presence of ADH, RS has a low risk of upstage [36, 37]. FEA is often seen in combination with other high-risk lesions and is suggested to be a precursor lesion to both ADH and carcinoma [38, 39]. Srour et al. found a statistically significant increase in UR for FEA with ADH (18.6%) compared to pure FEA alone (3.2%) [40]. This finding is supported by Liu et al. who demonstrated that pure FEA had a zero rate of upstage to malignancy and the presence of concurrent ADH or RS with FEA had an increased UR [7]. Because of the increased UR for CD, a more aggressive management with earlier excision may be required; however, future studies with increased sample sizes are needed to explore which combinations predict UR.
The principal limitation of our study was that it was underpowered to detect small differences in UR for each of the four individual lesions (ADH, FEA, RS, and IDP). This was most evident for ADH, where there was a trend toward increased UR with time (27.8% for > 60 days vs 17.5% for ≤ 60) which the authors considered to be clinically relevant but did not reach statistical significance. To increase power, all lesions were considered together, but because the other three are separate entities with different upstage rates and questionable malignant potential, considering them together decreases generalizability and limits the meaningfulness of the study.
Another important consideration is that when these lesions do upstage, it is often to slow growing malignancies such as DCIS and low-grade IDC which are ER positive [19, 35, 41, 42]. The slow growth would also be expected of the lesions themselves and thus in the limited observation period captured by our study (most patients undergoing surgery within 60 days and only five having a delay of > 1 year), it would be unlikely to truly observe a progression to malignancy. Furthermore, besides possibly ADH, these lesions are not considered to be precancerous and are not removed to prevent cancer development. Thus, increased time is unlikely to be associated with increased upstage. Despite this, because delaying EB is rare, we saw COVID-19-related delays as an opportunity to evaluate its effect on our patients. There are other methods that may have accomplished this more effectively which we did not have the opportunity to pursue such as prospectively following patients that choose to omit surgery and undergo observation. The findings with ADH do raise an interesting clinical question regarding the timing of pression and necessitate further evaluation.
It is our institutional standard to refer all patients with these four lesions found during CNB for surgical discussion unless it is microscopic IDP or RS that was completely removed with CNB. Because we did not capture the potential outcome of patients who chose not to undergo excision, this confounds the question of upstage and timing because those patients would have had the longest observation period. Lastly, we did not include patients who only had a diagnosis of lobular neoplasia, as this does not trigger surgical referral at our institution determined to be discordant by radiologist review.
There are potential sources of bias that occurred in the identification of our cohort. The first is the radiographic findings that lead to biopsy. For the same film, one radiologist may interpret a certain finding as BIRADS 3, while another may classify it as BIRADS 4. Unfortunately, we did not capture BIRADS to parse out these potential differences. This interobserver variation also applies pathologically, where one pathologist may interpret epithelial atypia as ADH, and another as DCIS. By including only those patients who underwent EB, we introduced inclusion bias, where lesions of lower risk for upstage or for malignant transformation may have been managed successfully with observation instead of excision. Finally, the significance of these findings is limited by human error with both data entry and retrospective design.
Additional evaluation of the association between delay of EB on UR of ADH and between combination diagnoses and UR is warranted.
Conclusion
Delay of surgical excision for patients with ADH, FEA, IPD, and RS was not associated with an increased risk for upstage to malignancy. Although not statistically significant, patients with ADH had a clinically relevant difference in upstage rate after 60 days. These patients may not be suitable for surgical delay.
Data availability
The dataset generated during this research is not publically available because this was not approved by our institutional review board due to a dedication to patient confidentiality.
References
Weinfurtner RJ, Patel B, Laronga C, Lee MC, Falcon SL, Mooney BP, Yue B, Drukteinis JS (2015) Magnetic resonance imaging-guided core needle breast biopsies resulting in high-risk histopathologic findings: upstage frequency and lesion characteristics. Clin Breast Cancer 15(3):234–239
Winchester DJ, Bernstein JR, Jeske JM, Nicholson MH, Hahn EA, Goldschmidt RA, Watkin WG, Sener SF, Bilimoria MB, Barrera E Jr et al (2003) Upstaging of atypical ductal hyperplasia after vacuum-assisted 11-gauge stereotactic core needle biopsy. Arch Surg 138(6):619–622 (discussion 622–613)
Deshaies I, Provencher L, Jacob S, Côté G, Robert J, Desbiens C, Poirier B, Hogue JC, Vachon E, Diorio C (2011) Factors associated with upgrading to malignancy at surgery of atypical ductal hyperplasia diagnosed on core biopsy. Breast 20(1):50–55
Liberman L, Dershaw DD, Glassman JR, Abramson AF, Morris EA, LaTrenta LR, Rosen PP (1997) Analysis of cancers not diagnosed at stereotactic core breast biopsy. Radiology 203(1):151–157
Rageth CJ, O’Flynn EA, Comstock C, Kurtz C, Kubik R, Madjar H, Lepori D, Kampmann G, Mundinger A, Baege A et al (2016) First international consensus conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 159(2):203–213
Mesurolle B, Perez JC, Azzumea F, Lemercier E, Xie X, Aldis A, Omeroglu A, Meterissian S (2014) Atypical ductal hyperplasia diagnosed at sonographically guided core needle biopsy: frequency, final surgical outcome, and factors associated with underestimation. AJR Am J Roentgenol 202(6):1389–1394
Liu C, Dingee CK, Warburton R, Pao JS, Kuusk U, Bazzarelli A, Sidhu R, McKevitt EC (2020) Pure flat epithelial atypia identified on core needle biopsy does not require excision. Eur J Surg Oncol 46(2):235–239
Uzoaru I, Morgan BR, Liu ZG, Bellafiore FJ, Gaudier FS, Lo JV, Pakzad K (2012) Flat epithelial atypia with and without atypical ductal hyperplasia: to re-excise or not. results of a 5-year prospective study. Virchows Arch 461(4):419–423
Chivukula M, Bhargava R, Tseng G, Dabbs DJ (2009) Clinicopathologic implications of “flat epithelial atypia” in core needle biopsy specimens of the breast. Am J Clin Pathol 131(6):802–808
Piubello Q, Parisi A, Eccher A, Barbazeni G, Franchini Z, Iannucci A (2009) Flat epithelial atypia on core needle biopsy: which is the right management? Am J Surg Pathol 33(7):1078–1084
Ingegnoli A, d’Aloia C, Frattaruolo A, Pallavera L, Martella E, Crisi G, Zompatori M (2010) Flat epithelial atypia and atypical ductal hyperplasia: carcinoma underestimation rate. Breast J 16(1):55–59
Kupsik M, Perez C, Bargaje A (2019) Upstaging papillary lesions to carcinoma on surgical excision is not impacted by patient race. Breast Dis 38(2):67–72
Li X, Aho M, Newell MS, Clifford K, Patel JG, Jou S, Cohen MA (2020) Papilloma diagnosed on core biopsies has a low upgrade rate. Clin Imaging 60(1):67–74
Martaindale S, Omofoye TS, Teichgraeber DC, Hess KR, Whitman GJ (2020) Imaging follow-up versus surgical excision for radial scars identified on tomosynthesis-guided core needle biopsy. Acad Radiol 27(3):389–394
Phantana-Angkool A, Forster MR, Warren YE, Livasy CA, Sobel AH, Beasley LM, Trufan SJ, Hadzikadic-Gusic L, Sarantou T, Voci AE et al (2019) Rate of radial scars by core biopsy and upgrading to malignancy or high-risk lesions before and after introduction of digital breast tomosynthesis. Breast Cancer Res Treat 173(1):23–29
Brenner RJ, Jackman RJ, Parker SH, Evans WP, Philpotts L, Deutch BM, Lechner MC, Lehrer D, Sylvan P, Hunt R et al (2002) Percutaneous core needle biopsy of radial scars of the breast: when is excision necessary? Am J Roentgenol 179(5):1179–1184
Maganini RO, Klem DA, Huston BJ, Bruner ES, Jacobs HK (2001) Upgrade rate of core biopsy-determined atypical ductal hyperplasia by open excisional biopsy. Am J Surg 182(4):355–358
Hartmann LC, Degnim AC, Santen RJ, Dupont WD, Ghosh K (2015) Atypical hyperplasia of the breast—risk assessment and management options. N Engl J Med 372(1):78–89
Hartmann LC, Radisky DC, Frost MH, Santen RJ, Vierkant RA, Benetti LL, Tarabishy Y, Ghosh K, Visscher DW, Degnim AC (2014) Understanding the premalignant potential of atypical hyperplasia through its natural history: a longitudinal cohort study. Cancer Prev Res (Phila) 7(2):211–217
Larson P, de las Morenas A, Cerda S, Bennett S, Cupples L, Rosenberg C (2006) Quantitative analysis of allele imbalance supports atypical ductal hyperplasia lesions as direct breast cancer precursors. J Pathol 209(3):307–316
Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, Patel SA, Boraas M, Chang EI, Topham NS et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Chae BJ, Lee A, Song BJ, Jung SS (2009) Predictive factors for breast cancer in patients diagnosed atypical ductal hyperplasia at core needle biopsy. World J Surg Oncol 7:77
Dupont WD, Page DL (1985) Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med 312(3):146–151
Liu C, Sidhu R, Ostry A, Warburton R, Pao JS, Dingee C, Kuusk U, McKevitt E (2019) Risk of malignancy in papillary neoplasms of the breast. Breast Cancer Res Treat 178(1):87–94
Matrai C, D’Alfonso TM, Pharmer L, Drotman MB, Simmons RM, Shin SJ (2015) Advocating nonsurgical management of patients with small, incidental radial scars at the time of needle core biopsy: a study of 77 cases. Arch Pathol Lab Med 139(9):1137–1142
Menes TS, Rosenberg R, Balch S, Jaffer S, Kerlikowske K, Miglioretti DL (2014) Upgrade of high-risk breast lesions detected on mammography in the breast cancer surveillance consortium. Am J Surg 207(1):24–31
Nassar A, Conners AL, Celik B, Jenkins SM, Smith CY, Hieken TJ (2015) Radial scar/complex sclerosing lesions: a clinicopathologic correlation study from a single institution. Ann Diagn Pathol 19(1):24–28
McGhan LJ, Pockaj BA, Wasif N, Giurescu ME, McCullough AE, Gray RJ (2012) Atypical ductal hyperplasia on core biopsy: an automatic trigger for excisional biopsy? Ann Surg Oncol 19(10):3264–3269
Kohr JR, Eby PR, Allison KH, DeMartini WB, Gutierrez RL, Peacock S, Lehman CD (2010) Risk of upgrade of atypical ductal hyperplasia after stereotactic breast biopsy: effects of number of foci and complete removal of calcifications. Radiology 255(3):723–730
Karwowski P, Lumley D, Stokes D, Pavlica M, Edsall B, Fu S, Francfort J, Cohen B, Capizzi A, Ma ZW et al (2021) atypical ductal hyperplasia on core needle biopsy: surgical outcomes of 200 consecutive cases from a high-volume breast program. Breast J 27(3):287–290
Raju U, Vertes D (1996) Breast papillomas with atypical ductal hyperplasia: a clinicopathologic study. Hum Pathol 27(11):1231–1238
Lewis JT, Hartmann LC, Vierkant RA, Maloney SD, Shane Pankratz V, Allers TM, Frost MH, Visscher DW (2006) An analysis of breast cancer risk in women with single, multiple, and atypical papilloma. Am J Surg Pathol 30(6):665–672
Miller CL, West JA, Bettini AC, Koerner FC, Gudewicz TM, Freer PE, Coopey SB, Gadd MA, Hughes KS, Smith BL et al (2014) Surgical excision of radial scars diagnosed by core biopsy may help predict future risk of breast cancer. Breast Cancer Res Treat 145(2):331–338
Mooney KL, Bassett LW, Apple SK (2016) Upgrade rates of high-risk breast lesions diagnosed on core needle biopsy: a single-institution experience and literature review. Mod Pathol 29(12):1471–1484
Ha SM, Cha JH, Shin HJ, Chae EY, Choi WJ, Kim HH, Oh HY (2018) Radial scars/complex sclerosing lesions of the breast: radiologic and clinicopathologic correlation. BMC Med Imaging 18(1):39
Rakha E, Beca F, D’Andrea M, Abbas A, Petrou-Nunn W, Shaaban AM, Kandiyil A, Smith S, Menon S, Elsheikh S et al (2019) Outcome of radial scar/complex sclerosing lesion associated with epithelial proliferations with atypia diagnosed on breast core biopsy: results from a multicentric UK-based study. J Clin Pathol 72(12):800–804
Catanzariti F, Avendano D, Cicero G, Garza-Montemayor M, Sofia C, Venanzi Rullo E, Ascenti G, Pinker-Domenig K, Marino MA (2021) High-risk lesions of the breast: concurrent diagnostic tools and management recommendations. Insights Imaging 12(1):63
Rudin AV, Hoskin TL, Fahy A, Farrell AM, Nassar A, Ghosh K, Degnim AC (2017) Flat epithelial atypia on core biopsy and upgrade to cancer: a systematic review and meta-analysis. Ann Surg Oncol 24(12):3549–3558
Srour MK, Donovan C, Chung A, Harit A, Dadmanesh F, Giuliano AE, Amersi F (2020) Flat epithelial atypia on core needle biopsy does not always mandate excisional biopsy. Breast J 26(4):679–684
Niu F, Wang L, Zhang W, Lyu S, Niu Y (2015) Value of CK5/6, CK14, ER and PR detection in differential diagnosis of intraductal proliferative lesions of the breast. Zhonghua Zhong Liu Za Zhi 37(10):749–752
Schnitt SJ (2003) The diagnosis and management of pre-invasive breast disease: flat epithelial atypia–classification, pathologic features and clinical significance. Breast Cancer Res 5(5):263–268
Acknowledgements
We would like to thank Nicole Corriveau for her support with IRB and logistics.
Funding
The authors declare that this research received no funding from any agency in the public, commercial, or non-profit sectors. The authors have no relevant financial or non-financial interests to declare. The REDCap electronic instrument used by our institution for all research was supported by Grant No. UL1TR002544 as indicated in the methods section above.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. Design and material preparation were performed by HM, JC, DL, APC, and SN. Data collection was performed by HM, JC, and EV. Data analysis was performed primarily by APC. The first draft of the manuscript was written by JC with the support of HM and EV. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. The protocol was submitted and reviewed by the institutional review board of Baystate Health prior to initiation and deemed to be exempt under Title IV due to the observational design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Casaubon, J., Niakan, S., Vicks, E. et al. The effect of delay of excisional biopsy on upstage rate for atypical ductal hyperplasia, flat epithelial atypia, intraductal papilloma, and radial scar. Breast Cancer Res Treat 196, 527–534 (2022). https://doi.org/10.1007/s10549-022-06745-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06745-7