Abstract
Aim of the study
The study aims to evaluate the performance of selected, high-volume, highly specialized, Italian Breast Centers at the time of COVID-19 pandemic (year 2020), compared to pre-pandemic time (year 2019), highlighting differences in terms of clinical presentation of breast cancer (BC) and therapeutic strategies.
Methods
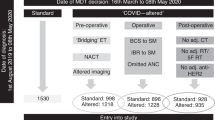
Patients’ data were provided by the Senonetwork data warehouse Senonet. In order to examine changes in the surgical and oncological management of BC patients during different phases of COVID-19 pandemic, we took advantage of a selection quality indicators (QIs). We performed the analyses in two time-frames, from July to September (Jul-Sep) (2019 versus 2020) and from October to December (Oct-Dec) (2019 versus 2020).
Results
Our analysis did not show any statistically significant difference in terms of diagnosis, surgical, oncological and radiation therapy procedures between the two trimesters 2019 and 2020. Nevertheless, we observed statistically significant differences, favoring 2020, when analyzing time-to surgery and time-to radiotherapy. On the other hand, we observed a significant reduction of neoadjuvant chemotherapy and we did not recollect any data on a major use of neoadjuvant endocrine therapy.
Conclusions
In Italian Breast Centers, partners of Senonetwork, we could not observe any treatment delay or change in standard clinical practice for BC care during the 2020 pandemic year, compared to 2019 pre-pandemic year. This finding is in contrast with the globally reported decrease in the performance of the Italian Breast Centers due to the COVID-19 pandemic, and has to be linked to the sharp selection of Senonetwork Breast Centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is a common disease affecting one in eight Western women and is potentially lethal. For the majority of patients with early stage BC, surgery remains the primary treatment and standard guidelines recommend to limit delay from diagnosis to start of treatment, because time-to-surgery, varying from greater than 30–60 days from diagnosis in different studies, has been reported to adversely affect BC prognosis [1,2,3]. The impact of COVID-19 pandemic on BC oncological surgery worldwide was considerable, and was determined not only by the reduction in surgical procedures, but also by postponement of screening procedures, clinical visits, exams and chemotherapy administration [4]. Early in the COVID-19 pandemic course, both US and European medical societies provided expert opinion regarding how best to manage and prioritize BC patients, issuing recommendations based on individual patient disease risk and hospital resources. For example, surgery delay in clinical stage I, postmenopausal, hormone receptors positive (HR +), HER2 negative tumors, considering neo-adjuvant endocrine therapy, or chemotherapy scheduling modification (switching, when appropriate, from weekly dosing to 2- or 3-weekly dosing) in order to reduce accesses to hospital, was proposed [5].
Aiming to accommodate the many changes brought about by COVID-19, BC care multidisciplinary Italian associations (composed of oncology, surgery, radiotherapy and radiology experts) collaborated to address recommended treatment strategies. These recommendations had three main goals: (1) to continue safe and effective oncological care for all new and known patients; (2) to decrease the risk of infection for patients and staff; and (3) to ensure the availability of protective materials, staff, and intensive care unit capacity for critically ill patients with COVID-19. Moreover, in line with efforts to prioritize care for COVID-19, national screening programs, including that for BC, were halted from March 2020 to approximately the end of April 2020, with differences in timing and implementational modalities varying across different Italian Regions.
Senonetwork Italia, a non-profit organization devoted to support the quality of multidisciplinary BC care, promoted a national survey to evaluate the impact of COVID-19 pandemic on clinical care of women with BC among Italian Breast Centers [6]. The survey showed how the majority of Italian Breast Centers were operating within hospitals involved in the treatment of COVID-19 patients [6]. Routine activities underwent a major decrease (more than 50%) especially in radiology, surgery, medical oncology and radiotherapy (in 38%, 22%, 11% and 5% of Breast Centers, respectively); in 38% of Breast Centers, the number of weekly procedures was reduced to 38% or more [6]. In addition, a decreased availability of operating room time was reported by the majority of Breast Centers (78%), equally distributed among low- and high-volume centers [6].
The present work aims to evaluate selected, high-volume, highly specialized, Italian Breast Centers performance and clinical presentation of BC at the time of COVID-19 pandemic (year 2020), compared to pre-pandemic time (year 2019), taking advantage of the Senonet electronic database, a data warehouse conceived to perform quality assessment and improvement of BC care in Italian Centers.
Patients and methods
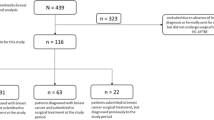
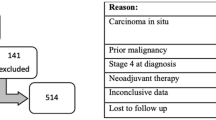
Patients’ selection and quality indicators
Patients’ data were provided by the Senonetwork data warehouse Senonet, which collects data sent by all Centers adhering to the project; Italian Centers involved in the analyses are listed in Table 1. Of note, in order to be part of Senonetwork, Italian Centers should count at least 150 BC cases per year, treated by a dedicated multidisciplinary team of a minimum of one breast surgeon, breast radiologist, breast radiation oncologist, breast medical oncologist and breast pathologist, as per European guidelines [7]. Each single Center provided anonymized patients clinic-pathological data to Senonet, which is protected and managed by a team of dedicated statisticians.
In order to monitor the quality of breast care, Senonet provided a set of benchmark quality indicators (QIs) [8], a selection of which was used in the present work to examine changes in the surgical and oncological management of patients with BC during the different phases of COVID-19 pandemic. The complete list of the Senonet QIs is shown in Table 2.
With the aim of analyzing specific differences in BC care between the pandemic year 2020 and the pre-pandemic year 2019, highlighting the specific effect of the different COVID-19 waves in Italy, we performed the analyses in two time-frames, considering the third and the fourth trimester of each year, from July to September (Jul–Sep) (2019 versus 2020) and from October to December (Oct–Dec) (2019 versus 2020). The choice of the study periods was based on specific epidemiological data for COVID-19 pandemic waves in Italy during 2019 and 2020 [9, 10].
Statistical methods
Quantitative and qualitative variables were described using medians and frequencies/percentages, respectively, as a total and in the four periods. For all the variables, proportion of missing cases was separately documented as proportions and not included in the calculation of distributions.
Differences in the indicators, all defined as proportions, were tested using the chi-squared test for trend in proportions; statistical significance was set at the 0.05 level. For each indicator, the denominator includes only eligible cases with information available; patients from Centers with more than 25% of missing information were removed from the denominator and the number of units involved in the calculation were documented for each indicator. All the analyses were performed using R version 4.0.5.
Results
A total of 6287 invasive lesions were analyzed, median age was 62, most of the patients underwent breast conserving surgery (BCS) (67.4%) and less than a quarter of patients performed neo-adjuvant chemotherapy (12.3%). Most of the patients presented with 1 to 2 cm lesions (pT1c) (38.8%) and had node-negative disease (pN0) (64.3%). The great majority of patients had estrogen and progesterone receptor (ER and PgR) positive disease (88.6% and 77.5%, respectively) and were HER2 negative (score 0–1 + or 2 + and FISH negative; 74.7% and 12.4%, respectively); median Ki-67 was 15%, with around half of the population presenting with Ki-67 < 15% and the other half with Ki-67 ≥ 15% (53.2% and 46.8%, respectively). Patients’ characteristics are depicted in Table 3, together with their subdivision into trimesters from both 2019 and 2020. No statistically significant differences were observed across the different time-frames in terms of disease stage at presentation, considering both the size of the primary tumor and the extent of lymph nodes involvement (data not shown). Analyzing differences in terms of pathological characteristics among the time-frames under investigation, we could observe a statistically significant major ER and PgR positive expression in 2020 compared to 2019 (ER + Trend Test p-value = 0.006; PgR + Trend Test p-value = 0.006), and higher number of HER2 + cases (HER2 Trend Test p-value = 0.038), while no significant differences in terms of Ki-67 percentage (Ki-67 Trend Test p-value = 0.999) were observed. Indeed, when looking at BC biological subtypes, triple negative (TN) BC was less prevalent in 2020 compared to 2019, while luminal-A like subtype seemed more prevalent in 2020 compared to 2019 (TNBC Trend Test p-value = 0.002; luminal-A like Trend Test p-value = < 0.001); no statistically significant differences were observed in the differential prevalence of luminal-B like/luminal-B HER2 + and HER2 enriched-like subtypes between 2019 and 2020 (data not shown). We further analyzed specific differences in terms of diagnosis and surgical treatment timing. Nearly all the surgically treated invasive BC cases had a proper radiological (Birads 5) and/or cytological (C5) confirmed pre-surgical diagnosis, across the two years-time considered (Trend Test p-value = 0.836), and a similar proportion of patients underwent a magnetic resonance imaging (MRI) before surgery (Trend Test p-value = 0.529) (Fig. 1A, B). Interestingly, in 2020 the time-to-surgery appeared to be shorter than in 2019, with surgery being performed more frequently in ≤ 30 days from clinical indication or in ≤ 42 days from the first test positive for invasive BC (Trend Test p-value = < 0.001 for both QIs) (Fig. 1C, D). Considering surgical indication, there were no statistically significant differences in terms of choice of adequate surgical procedure, with the great majority of patients, across all the time-frames in both 2019 and 2020, undergoing a single surgical procedure for both in situ and invasive lesions (Fig. 2A, B). Nevertheless, we observed a higher preference for BCS for treatment of invasive lesions ≤ 3 cm in 2020 compared to 2019, while no differences were seen in the rate of choice of BCS for non-invasive lesions ≤ 2 cm across the two years considered (Fig. 2C, D). Taking into account the management of the axilla, a statistically significant trend was observed, with more pN0 patients in 2020 treated with sentinel lymph node biopsy (SLNB), without axillary dissection (Trend Test p-value = < 0.001) (Fig. 2E). Lastly, we sought to analyze possible differences, between the considered time-frames in 2019 and 2020, also in non-surgical procedures, such as radiotherapy and oncological treatments. No statistically significant difference was observed in terms of radiotherapy indication, both after BCS (Trend Test p-value = 0.11) and after mastectomy in pN2a cases (Trend Test p-value = 0.7), while, in accordance to what was observed for time-to-surgery, we observed a better outcome in 2020 compared to 2019 in terms of time-to-radiotherapy, when the latter was clinically indicated (Trend Test p-value = < 0.001) (Fig. 3A–C). When analyzing oncological treatment indication, we could not find any statistically significant difference in terms of adjuvant treatments decision between the two years-time considered (Trend Test p-value = 0.478, 0.392 and 0.162 for endocrine therapy in hormone receptor positive case, chemotherapy for high risk hormone receptor negative cases and trastuzumab for HER2 + cases, respectively) (Fig. 3D–F). On the other hand, we observed a statistically significant reduction in neoadjuvant chemotherapy indication in 2020 compared to 2019 (Trend Test p-value = < 0.001).
Discussion
The present study, conducted among Senonetwork Italian Breast Centers, focused on the management of BC care during 2020 COVID-19 pandemic. Comparing patients’ clinic-pathological characteristics, diagnosis, surgical and medical treatment variables between 2019 and 2020 time-frames, we sought to investigate if, in this selected, high-volume network of Breast Centers, any change in standard practice occurred due to the onset of the pandemic. To do so, we took advantage of data collected in Senonet, the Senonetwok data warehouse, and used a set of QIs, configured to monitor quality and commitment of Breast Centers in BC care, to describe changes in specific BC treatment areas.
Our analysis did not show any statistically significant difference in terms of diagnosis, surgical, oncological and radiation therapy procedures when comparing the two trimesters of the years considered. Nevertheless, we observed statistically significant differences, favoring the 2020 pandemic year, when analyzing time-to surgery and time-to radiotherapy (when indicated). This could be explained by an improvement in treatment strategies and even more strict collaboration between different Breast Centers. Indeed, since the first onset of the pandemic, Italian Breast Centers’ activities have been promptly reorganized, in response to the need of balancing the emergency of COVID-19 patients with the urgency of continuum of care for oncological patients, bearing in mind the potential exposure to SARS-CoV-2 infection of these frail patients. As cited before, many international guidelines recommended postponing surgery in low to medium risk BC patients, favoring neoadjuvant approaches, with many studies reporting a five-fold increment in the choice for neoadjuvant endocrine therapy in HR positive, HER2 negative tumors [11, 12]. In our dataset, we observed a significant reduction in the use of neoadjuvant chemotherapy and we did not recollect any data on a major use of neoadjuvant endocrine therapy. This might be due to the fact that our high-volume, highly selected, Breast Centers were restructured to serve as BC care hubs for other low volume Hospitals and were organized to be able to perform upfront surgery (mainly BCS, as encouraged by International Guidelines) to the majority of ≤ 3 cm, HR positive, HER2 negative patients.
Moreover, a major implement of SLNB, without axillary lymph node dissection (ALND), was observed in our case series in 2020 compared to 2019. This might be explained by the elevated number of small, cN0 tumors selected for upfront surgery, as previously explained, but it might also reflect the gradual paradigm shift that the surgical management of the axilla have been encompassing through the last years, due to the wide acceptance of Z0011 trial findings on the possibility of omitting ALND in selected low-risk tumors [13].
Regarding radiation therapy, moderate-hypofractionated schedules were strongly recommended during the COVID-19 pandemic, reducing treatment duration and patients’ risk exposure [14], and in case of clinical indication for a boost, a further dose to the tumor bed, was preferably a simultaneous integrated one [15]. These management indications, together with the possibility of addressing BC patients to dedicated Breast Centers hubs for adjuvant radiotherapy and the lowering of indications for palliative radiation treatments, might explain the shorter time-to radiotherapy observed in our case series in 2020 compared to 2019.
Immediate breast reconstruction was offered also during COVID-19 pandemic in order to maintain therapeutic standards, nevertheless some degree of variation in the clinical protocol was adopted by many centers to face the pandemic outbreak [16].
In conclusion, even if we globally observed a decrease in the performance of the Italian Breast Centers due to the COVID-19 pandemic, with major issues regarding an adequate and prompt access to treatment [6], in our study, providing data from a highly selected network of high-volume Breast Centers, we could not notice any treatment delay or radical change in standard clinical practice. These findings probably reflect the Senonetwork selection of Breast Centers fulfilling high-standard requirements of multidisciplinary organization and the capability of this network of Brest Centers to cooperate, joining forces also to serve as surgical and radiation therapy hubs for the nearest territorial area.
Due to the persistence of pandemic waves after 2020 and the unceasing need for COVID-19 inpatient care, which might lead to an increased number of women with advanced BC at diagnosis in the future, we still need to accurately monitor the performance of Italian Breast Centers through the years and take in place appropriate actions to prevent disfunction in the health care of oncologic patients.
Data availability
Enquiries about data availability should be directed to the authors.
References
Tjoe JA, Heslin K, Perez Moreno AC, Thomas S, Kram JJF (2022) Factors associated with breast cancer surgery delay within a coordinated multihospital community health system: when does surgical delay impact outcome? Clin Breast Cancer 22(1):e91–e100
Rosselli Del Turco M, Ponti A, Bick U, Biganzoli L, Cserni G, Cutuli B et al (2010) Quality indicators in breast cancer care. Eur J Cancer 46(13):2344–2356
Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330
Glasbey J, Ademuyiwa A, Adisa A, AlAmeer E, Arnaud AP, Ayasra F et al (2021) Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol 22(11):1507–1517
Dietz JR, Moran MS, Isakoff SJ, Kurtzman SH, Willey SC, Burstein HJ et al (2020) Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat 181(3):487–497
Fortunato L, d’Amati G, Taffurelli M, Tinterri C, Marotti L, Cataliotti L (2021) Severe Impact of Covid-19 pandemic on breast cancer care in Italy: a senonetwork national survey. Clin Breast Cancer 21(3):e165–e167
Wilson ARM, Marotti L, Bianchi S, Biganzoli L, Claassen S, Decker T et al (2013) The requirements of a specialist breast centre. Eur J Cancer 49(17):3579–3587
Biganzoli L, Marotti L, Hart CD, Cataliotti L, Cutuli B, Kühn T et al (2017) Quality indicators in breast cancer care: An update from the EUSOMA working group. Eur J Cancer 86:59–81
Fochesato A, Simoni G, Reali F, Giordano G, Domenici E, Marchetti L (2021) A retrospective analysis of the COVID-19 pandemic evolution in Italy. Biology 10(4):311
Dorrucci M, Minelli G, Boros S, Manno V, Prati S, Battaglini M et al (2021) Excess mortality in Italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Front Public Health 16(9):669209
Wilke LG, Nguyen TT, Yang Q, Hanlon BM, Wagner KA, Strickland P et al (2021) Analysis of the Impact of the COVID-19 pandemic on the multidisciplinary management of breast cancer: review from the American society of breast surgeons COVID-19 and mastery registries. Ann Surg Oncol 28(10):5535–5543
Dave RV, Kim B, Courtney A, O’Connell R, Rattay T, Taxiarchi VP et al (2021) Breast cancer management pathways during the COVID-19 pandemic: outcomes from the UK ‘Alert Level 4’ phase of the B-MaP-C study. Br J Cancer 124(11):1785–1794
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR et al (2017) Effect of axillary dissection vs no axillary dissection on 10-Year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318(10):918
Coles CE, Aristei C, Bliss J, Boersma L, Brunt AM, Chatterjee S et al (2020) International guidelines on radiation therapy for breast cancer during the COVID-19 pandemic. Clin Oncol 32(5):279–281
Lancia A, Bonzano E, Bottero M, Camici M, Catellani F, Ingrosso G (2020) Radiotherapy in the era of COVID-19. Expert Rev Anticancer Ther 20(8):625–627
Lisa A, Battistini A, Giannasi S, Veronesi A, Bandi V, Maione L et al (2020) Breast reconstruction in a coronavirus disease 2019 hub. Plast Reconstr Surg—Glob Open 8(7):e3043
Acknowledgements
Francesca Pellini (Azienda Ospedaliera Universitaria Integrata, Verona, Italy), Simona Grossi (Breast Centre Ortona - ASL2 Abruzzo, Italy), Marina Bortul (Breast Unit Trieste, Azienda Sanitaria Universitaria Giuliano Isontina, Trieste, Italy), Alfredo Tafà AUSL di Bologna (IRCCS Scienze Neurologiche, Ospedale Bellaria, Italy), Giovanni Tazzioli (Breast Unit Azienda Ospedaliero-Universitaria Policlinico di Modena, Italy), Matteo Ghilli (Centro Senologico Multidisciplinare, AOUP, Pisa, Italy), Tiziana Mastropietro (Centro di Senologia, Azienda Ospedaliera San Giovanni Addolorata, Rome, Italy), Francesco Caruso (Breast Centre Humanitas Catania, Misterbianco, Catania, Italy), Andrea Bonetti (Breast Centre Azienda ULSS9 Scaligera, Ospedale Mater Sautis Legnago, Verona, Italy), Angelica Della Valle (Breast Surgery Department, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy), Alessandra Huscher (Fondazione Poliambulanza, Brescia, Italy), Corrado Tinterri (Breast Unit, Humanitas Research Hospital, IRCCS, Rozzano, Milan, Italy), Armando Santoro (UO of Medical Oncology, Department of Oncology and Hematology, Humanitas Research Hospital, IRCCS, Rozzano, Milan, Italy; Department of Biomedical Sciences, Humanitas University, Pieve Emanuele, Milan, Italy), Marco Klinger (Reconstructive and Aesthetic Plastic Surgery School, Department of Medical Biotechnology and Translational Medicine BIOMETRA - Plastic Surgery Unit, University of Milan, Humanitas Research Hospital, IRCCS, Rozzano, Milan, Italy), Mario Taffurelli (IRCCS Azienda Ospedaliero-Universitaria di Bologna, Policlinico di S. Orsola, Bologna, Italy), Fabio Corsi (Breast Unit, Department of Surgery, Istituti Clinici Scientifici Maugeri IRCCS, Pavia, Italy; Department of Biomedical and Clinical Sciences “Luigi Sacco”, Università di Milano, Milan, Italy), Paolo Veronesi (IRCCS Istituto Europeo di Oncologia, Milan; Università degli Studi di Milano, Dipartimento di Oncologia ed Ematologia, Milan, Italy), Bettina Ballardini (Breast Division, Multimedica Breast Unit, Multimedica IRCCS, Milan, Italy), Laura Biganzoli (Oncologia Medica Sandro Pitigliani, Nuovo Ospedale di Prato, Prato, Italy), Maggiorino Barbero (Breast Unit, Ospedale Cardinal Massaia, Asti, Italy), Romano Polato (Ospedale Centrale di Bolzano, Azienda Sanitaria dell'Alto Adige, Comprensorio Sanitario di Bolzano, Italy) Sonia Santicchia (Ospedale Infermi di Rimini-Sant'Arcangelo di Romagna, Italy)
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of Senonetwork Working group are listed in the acknowledgement section.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Losurdo, A., Lisa, A.V.E., Tomatis, M. et al. Highly specialized Breast Centers did not experience delay of care during COVID-19 pandemic in Italy: the Senonetwork experience. Breast Cancer Res Treat 196, 87–95 (2022). https://doi.org/10.1007/s10549-022-06694-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06694-1