Abstract
Background
Guidelines support comparable treatment for women diagnosed with breast cancer during pregnancy (PrBC) and nonpregnant women with limited case-specific modifications to ensure maternal–fetal safety. Experience during pregnancy with modern agents, such as taxanes or granulocyte colony-stimulating factors (GCSF), is limited.
Patients and methods
We retrospectively identified a multi-institutional cohort of PrBC between 1996 and 2020. Propensity score analyses with multiple imputation for missing variables were applied to determine the associations between chemotherapy exposures during pregnancy, with or without taxanes or GCSF, and a compound maternal–fetal outcome including spontaneous preterm birth, preterm premature rupture of membranes, chorioamnionitis, small for gestational age newborns, congenital malformation, or 5-min Apgar score < 7.
Results
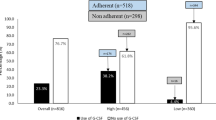
Among 139 PrBC pregnancies, 82 (59.0%) were exposed to chemotherapy, including 26 (31.7%) to taxane and 18 (22.0%) to GCSF. Chemotherapy use, in general, and inclusion of taxane and/or GCSF, specifically, increased over time. Pregnancies resulting in live singleton births (n = 123) and exposed to chemotherapy were as likely to reach term as those that were not (59.5% vs. 63.6%, respectively, punadjusted = 0.85). Among women treated with chemotherapy, propensity score-matched odds ratios (OR) for the composite maternal–fetal outcome were not significantly increased with taxane (OR 1.24, 95% CI 0.27–5.72) or GCSF (OR 2.11, 95% confidence interval (CI) 0.48–9.22) with similar effects in multiple imputation and sensitivity models.
Conclusion
The judicious increased use of taxane chemotherapy and/or growth factor support during pregnancy was not associated with unfavorable short-term maternal–fetal outcomes. While these findings are reassuring, case numbers remain limited and continued surveillance of these patients and progeny is warranted.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Petrek JA (1994) Breast cancer during pregnancy. Cancer 74(1 Suppl):518–527. https://doi.org/10.1002/cncr.2820741341
Johnson RH, Anders CK, Litton JK, Ruddy KJ, Bleyer A (2018) Breast cancer in adolescents and young adults. Pediatr Blood Cancer 65(12):e27397. https://doi.org/10.1002/pbc.27397
Andersson TM, Johansson ALV, Hsieh CC, Cnattingius S, Lambe M (2009) Increasing incidence of pregnancy-associated breast cancer in Sweden. Obstet Gynecol 114(3):568–572. https://doi.org/10.1097/AOG.0b013e3181b19154
Amant F, Lefrere H, Borges VF, Cardonick E, Lambertini M, Loibl S, Peccatori F, Partridge A, Schedin P (2021) The definition of pregnancy-associated breast cancer is outdated and should no longer be used. Lancet Oncol 22(6):753–754. https://doi.org/10.1016/S1470-2045(21)00183-2
Lee GE, Mayer EL, Partridge A (2017) Prognosis of pregnancy-associated breast cancer. Breast Cancer Res Treat 163(3):417–421. https://doi.org/10.1007/s10549-017-4224-6
Stensheim H, Moller B, van Dijk T, Fossa SD (2009) Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort study. J Clin Oncol 27(1):45–51. https://doi.org/10.1200/JCO.2008.17.4110
Amant F, von Minckwitz G, Han SN, Bontenbal M, Ring AE, Giermek J, Wildiers H, Fehm T, Linn SC, Schlehe B, Neven P, Westenend PJ, Muller V, Van Calsteren K, Rack B, Nekljudova V, Harbeck N, Untch M, Witteveen PO, Schwedler K, Thomssen C, Van Calster B, Loibl S (2013) Prognosis of women with primary breast cancer diagnosed during pregnancy: results from an international collaborative study. J Clin Oncol 31(20):2532–2539. https://doi.org/10.1200/jco.2012.45.6335
Amant F, Vandenbroucke T, Verheecke M, Fumagalli M, Halaska MJ, Boere I, Han S, Gziri MM, Peccatori F, Rob L, Lok C, Witteveen P, Voigt JU, Naulaers G, Vallaeys L, Van den Heuvel F, Lagae L, Mertens L, Claes L, Van Calsteren K, International Network on Cancer and Infertility Pregnancy (2015) Pediatric outcome after maternal cancer diagnosed during pregnancy. N Engl J Med 373(19):1824–1834. https://doi.org/10.1056/NEJMoa1508913
Poggio F, Tagliamento M, Pirrone C, Soldato D, Conte B, Molinelli C, Cosso M, Fregatti P, Del Mastro L, Lambertini M (2020) Update on the management of breast cancer during pregnancy. Cancers (Basel). https://doi.org/10.3390/cancers12123616
Loibl S, Han SN, von Minckwitz G, Bontenbal M, Ring A, Giermek J, Fehm T, Van Calsteren K, Linn SC, Schlehe B, Gziri MM, Westenend PJ, Muller V, Heyns L, Rack B, Van Calster B, Harbeck N, Lenhard M, Halaska MJ, Kaufmann M, Nekljudova V, Amant F (2012) Treatment of breast cancer during pregnancy: an observational study. Lancet Oncol 13(9):887–896. https://doi.org/10.1016/S1470-2045(12)70261-9
Loibl S, Schmidt A, Gentilini O, Kaufman B, Kuhl C, Denkert C, von Minckwitz G, Parokonnaya A, Stensheim H, Thomssen C, van Calsteren K, Poortmans P, Berveiller P, Markert UR, Amant F (2015) Breast cancer diagnosed during pregnancy: adapting recent advances in breast cancer care for pregnant patients. JAMA Oncol 1(8):1145–1153. https://doi.org/10.1001/jamaoncol.2015.2413
Meisel JL, Economy KE, Calvillo KZ, Schapira L, Tung NM, Gelber S, Kereakoglow S, Partridge AH, Mayer EL (2013) Contemporary multidisciplinary treatment of pregnancy-associated breast cancer. Springerplus 2(1):297. https://doi.org/10.1186/2193-1801-2-297
Freret TS, Exman P, Mayer EL, Little SE, Economy KE (2020) Birthweight and chemotherapy exposure in women diagnosed with breast cancer during pregnancy. Am J Perinatol. https://doi.org/10.1055/s-0040-1717075
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70(1):41–55. https://doi.org/10.1093/biomet/70.1.41
Li L, Greene T (2013) A weighting analogue to pair matching in propensity score analysis. Int J Biostat 9(2):215–234. https://doi.org/10.1515/ijb-2012-0030
Egbe A, Uppu S, Lee S, Stroustrup A, Ho D, Srivastava S (2015) Congenital malformations in the newborn population: a population study and analysis of the effect of sex and prematurity. Pediatr Neonatol 56(1):25–30. https://doi.org/10.1016/j.pedneo.2014.03.010
de Haan J, Verheecke M, Van Calsteren K, Van Calster B, Shmakov RG, Mhallem Gziri M, Halaska MJ, Fruscio R, Lok CAR, Boere IA, Zola P, Ottevanger PB, de Groot CJM, Peccatori FA, Dahl Steffensen K, Cardonick EH, Polushkina E, Rob L, Ceppi L, Sukhikh GT, Han SN, Amant F, International Network on Cancer and Infertility Pregnancy (2018) Oncological management and obstetric and neonatal outcomes for women diagnosed with cancer during pregnancy: a 20-year international cohort study of 1170 patients. Lancet Oncol 19(3):337–346. https://doi.org/10.1016/S1470-2045(18)30059-7
Zagouri F, Sergentanis TN, Chrysikos D, Dimitrakakis C, Tsigginou A, Zografos CG, Dimopoulos MA, Papadimitriou CA (2013) Taxanes for breast cancer during pregnancy: a systematic review. Clin Breast Cancer 13(1):16–23. https://doi.org/10.1016/j.clbc.2012.09.014
Loibl S, von Minckwitz G, Gwyn K, Ellis P, Blohmer JU, Schlegelberger B, Keller M, Harder S, Theriault RL, Crivellari D, Klingebiel T, Louwen F, Kaufmann M (2006) Breast carcinoma during pregnancy. International recommendations from an expert meeting. Cancer 106(2):237–246. https://doi.org/10.1002/cncr.21610
O’Laughlin ASS, Fleischer L, Akoto S, Cardonick E (2019) Safety of Taxane Chemotherapy in Breast Cancer During Pregnancy [28O]. Obstet Gynecol 133:169–170. https://doi.org/10.1097/01.AOG.0000558888.89911.f0
Cardonick E, Bhat A, Gilmandyar D, Somer R (2012) Maternal and fetal outcomes of taxane chemotherapy in breast and ovarian cancer during pregnancy: case series and review of the literature. Ann Oncol 23(12):3016–3023. https://doi.org/10.1093/annonc/mds170
Mir O, Berveiller P, Goffinet F, Treluyer JM, Serreau R, Goldwasser F, Rouzier R (2010) Taxanes for breast cancer during pregnancy: a systematic review. Ann Oncol 21(2):425–426. https://doi.org/10.1093/annonc/mdp517
Boxer LA, Bolyard AA, Kelley ML, Marrero TM, Phan L, Bond JM, Newburger PE, Dale DC (2015) Use of granulocyte colony-stimulating factor during pregnancy in women with chronic neutropenia. Obstet Gynecol 125(1):197–203. https://doi.org/10.1097/AOG.0000000000000602
Zeidler C, Grote UA, Nickel A, Brand B, Carlsson G, Cortesao E, Dufour C, Duhem C, Notheis G, Papadaki HA, Tamary H, Tjonnfjord GE, Tucci F, Van Droogenbroeck J, Vermylen C, Voglova J, Xicoy B, Welte K (2014) Outcome and management of pregnancies in severe chronic neutropenia patients by the European branch of the severe chronic neutropenia international registry. Haematologica 99(8):1395–1402. https://doi.org/10.3324/haematol.2013.099101
Berends C, Maggen C, Lok CAR, van Gerwen M, Boere IA, Wolters V, Van Calsteren K, Segers H, van den Heuvel-Eibrink MM, Painter RC, Gziri MM, Amant F (2021) Maternal and neonatal outcome after the use of G-CSF for cancer treatment during pregnancy. Cancers (Basel). https://doi.org/10.3390/cancers13061214
Cardonick E, Gilmandyar D, Somer RA (2012) Maternal and neonatal outcomes of dose-dense chemotherapy for breast cancer in pregnancy. Obstet Gynecol 120(6):1267–1272. https://doi.org/10.1097/AOG.0b013e31826c32d9
Cardonick EIF, Torres N (2012) The use of neupogen (Filgrastim) or Neulasta (Pegfilgrastim) during pregnancy when chemotherapy is indicated for maternal cancer treatment. J Cancer Ther 3(2):157–161. https://doi.org/10.4236/jct.2012.32021
Zagouri F, Korakiti AM, Zakopoulou R, Kyriazoglou A, Zografos E, Haidopoulos D, Apostolidou K, Papatheodoridi MA, Dimopoulos MA (2019) Taxanes during pregnancy in cervical cancer: a systematic review and pooled analysis. Cancer Treat Rev 79:101885. https://doi.org/10.1016/j.ctrv.2019.08.001
Andrikopoulou A, Korakiti AM, Apostolidou K, Dimopoulos MA, Zagouri F (2021) Immune checkpoint inhibitor administration during pregnancy: a case series. ESMO Open 6(5):100262. https://doi.org/10.1016/j.esmoop.2021.100262
Acknowledgements
Tal Sella is supported by the Goldfarb Advanced Fellowship in Breast Oncology at Dana-Farber Cancer Institute and is also supported by The American Physicians Fellowship for Medicine in Israel and the Pinchas Borenstein Talpiot Medical Leadership Program, Chaim Sheba Medical Center, Tel-Hashomer, Israel.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization was performed by TS, PE, ELM, and AHP; methodology, formal analysis, and investigation were performed by TS, PE, SR, TSF, NT, and ELM; writing—original draft preparation was carried out by TS and PE; writing—review and editing was performed by all authors; and resources and supervision were performed by ELM.
Corresponding author
Ethics declarations
Conflict of interests
Heather A. Parsons has received funding to the institution from Puma. Nancy U. Lin has received grant/contract funding to the institution from Genentech, Merck, Pfizer, Seattle Genetics, Zion Pharmaceuticals, Olema Pharmaceuticals, and AstraZeneca; consulting fees/honorarium for consulting/ad board participation from Puma, Seattle Genetics, AstraZeneca, Daiichi-Sankyo, Denali Therapeutics, Olema Pharma, Prelude Therapeutics, Aleta BioPharma, Voyager Therapeutics, Affinia Therapeutics, and Pfizer; royalties from UpToDate; and stock and other ownership interests in Artera Inc. Nadine M. Tung has received research funding from AstraZeneca. Erica L. Mayer has received consulting/advising fees from Novartis, Lilly, Gilead, and AstraZeneca. All remaining authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented as a poster at the 2018 San Antonio Breast Cancer Symposium; December 4–8, 2018; San Antonio, Texas.
Rights and permissions
About this article
Cite this article
Sella, T., Exman, P., Ren, S. et al. Outcomes after treatment of breast cancer during pregnancy including taxanes and/or granulocyte colony-stimulating factor use: findings from a multi-institutional retrospective analysis. Breast Cancer Res Treat 194, 597–606 (2022). https://doi.org/10.1007/s10549-022-06621-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06621-4