Abstract
Breast cancer diagnosed during pregnancy poses unique challenges. Application of standard treatment algorithms is limited by lack of level I evidence from randomized trials. This study describes contemporary multidisciplinary treatment of pregnancy-associated breast cancer (PABC) in an academic setting and explores early maternal and fetal outcomes. A search of the Dana-Farber/Harvard Cancer Center clinical databases was performed to identify PABC cases. Sociodemographic, disease, pregnancy, and treatment information, as well as data on short-term maternal and fetal outcomes, were collected through retrospective chart review. 74 patients were identified, the majority with early-stage breast cancer. Most (73.5%) underwent surgical resection during pregnancy, including 40% with sentinel lymph node biopsy and 32% with immediate reconstruction. A total of 36 patients received anthracycline-based chemotherapy during pregnancy; of those, almost 20% were on a dose-dense schedule and 8.3% also received paclitaxel. 68 patients delivered liveborn infants; over half were delivered preterm (< 37 weeks), most scheduled to allow further maternal cancer therapy. For the infants with available data, all had normal Apgar scores and over 90% had birth weight >10th percentile. The rate of fetal malformations (4.4%) was not different than expected population rate. Within a multidisciplinary academic setting, PABC treatment followed contemporary algorithms without apparent increase in maternal or fetal adverse outcomes. A considerable number of preterm deliveries were observed, the majority planned to facilitate cancer therapy. Continued attention to maternal and fetal outcomes after PABC is required to determine the benefit of this delivery strategy.
Similar content being viewed by others
Introduction
It is estimated that cancer complicates as many as 1 in 1000 pregnancies, with breast cancer as the most common associated malignancy (Smith et al. 2001). Contemporary management of pregnancy-associated breast cancer (PABC) encourages continuation of pregnancy during treatment. Limitations in published data describing the safety of cancer therapy in pregnancy create challenges and dilemmas in clinical decision-making for providers caring for these patients. Prospective evaluation of the safety of antineoplastic therapy during pregnancy is methodologically difficult; therefore, most published data consist of case and cohort series (Mir et al. 2008; Cardonick et al. 2012a; Loibl et al. 2012). Given the apparent rising incidence of PABC, perhaps due to trends in delaying pregnancy (Andersson et al. 2009; Litton & Theriault 2010), a greater understanding of the pathologic features, treatment options, and maternal and fetal outcomes in PABC is critical.
PABC has been defined as breast cancer diagnosed during pregnancy and up to one year postpartum. Although much PABC research has considered this group as a whole, it is worth considering two distinct subsets – those diagnosed during pregnancy, and those diagnosed in the postpartum period (Borges & Schedin 2011). Physicians caring for a pregnant patient with active breast cancer must select treatment options which maximize benefits to the patient while minimizing risks to the developing fetus. Given the advances in contemporary management of breast cancer, including use of taxanes, “dose dense” schedules, and sentinel lymph node biopsy, it is imperative to understand whether or not these new treatments can be safely administered during pregnancy.
With these considerations, a cohort of breast cancer patients treated during pregnancy was identified at an academic comprehensive cancer center. This study examined the distribution of tumor subtypes, treatment decisions, and maternal and fetal outcomes within the cohort, and evaluated the contemporary management of PABC supported by a multidisciplinary team.
Methods
A retrospective cohort of patients diagnosed with breast cancer during pregnancy was created through a search of the Dana Farber/Harvard Cancer Center (DF/HCC) clinical database. Eligibility criteria included: a history of pathologically confirmed breast cancer diagnosed during pregnancy, at least two follow-up visits for treatment documented within the DF/HCC system (including the Dana-Farber Cancer Institute, Massachusetts General Hospital, Brigham and Women’s Hospital, and Beth Israel Deaconess Medical Center) to identify continuous care, and age > 18 years. Medical oncologists, breast surgeons, and maternal-fetal medicine specialists within the DF/HCC institutions were also queried to identify eligible patients treated in their practices. Comprehensive review of the DF/HCC database was used to gather patient information as well as data on short-term maternal and fetal outcomes. Statistical analysis was exploratory and descriptive in nature. Institutional Review Board approval was obtained prior to initiation of this study.
Results
Patient and disease characteristics
Seventy-four patients with PABC were identified who met inclusion criteria. Detailed demographic and disease characteristics are presented in Table 1. Most patients (62%) received their diagnosis after 2005. The median age at diagnosis was 34 years (range 25–40), with 63 (85.1%) patients aged 30 or older at the time of diagnosis. The timing of presentation varied with 25 (33.8%) patients diagnosed in the first trimester, 30 (40.5%) in the second trimester, and 19 (25.7%) in the third trimester. Sixty-eight of the 74 patients (91.9%) carried their infants to term. One patient miscarried and five pregnancies were electively terminated during the first trimester, prior to initiating cancer therapy.
The majority of patients (83.8%) were diagnosed with early-stage disease; only two had metastatic disease at the time of presentation. All were tested to evaluate tumor hormone receptor and HER2 status; 46 (62.2%) were ER/PR positive, 25 (33.8%) were HER2 positive, and 14 (18.9%) had triple-negative breast cancer. A total of 50 patients (67.6%) had BRCA testing performed, and in this subset, 6 (12.0%) tested positive for either a BRCA 1 or 2 mutation.
Imaging
Most patients (67, 90.5%) underwent imaging to stage their disease while pregnant. A total of 54 (73.0%) underwent breast ultrasound, 30 (44.8%) underwent mammography, and 14 (20.9%) underwent chest or abdominal x-ray. A minority (8, 11.9%) underwent MRI of the breast, abdomen and/or spinal cord, and of this subset, about half received gadolinium. No patients underwent computed tomography while pregnant.
Local therapy
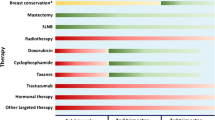
Fifty of 68 patients (73.5%) who carried their pregnancies to term underwent surgery during pregnancy (see Table 2). Of this group, 39 underwent either lumpectomy or mastectomy, and 11 underwent more than one operation, resulting in a total of 37 lumpectomies and 25 mastectomies performed during pregnancy in the overall cohort. A total of 11 (17.7%) surgeries were performed during the first trimester and 35 (56.5%) in the second trimester. Immediate reconstruction was performed after 8 (32%) of the mastectomies during pregnancy. In those having surgery, sentinel lymph node biopsy was performed in 20 patients (40.0%), with 12 procedures employing radiolabeled tracer and 7 using blue dye.
Systemic therapy
Thirty-six of the 68 patients (52.9%) who carried pregnancies to term received chemotherapy (see Table 3); 29 (80.6%) started chemotherapy in the second trimester and 7 (19.4%) started chemotherapy in the third trimester. No chemotherapy was administered in the first trimester. Decisions regarding agent selection and schedule were left to the discretion of the treating physician after consultation with patients, although opinion from multidisciplinary tumor board was considered in many cases as well. All 36 patients received doxorubicin and cyclophosphamide (AC) and 26 (72.2%) completed 4 cycles during pregnancy; of those receiving AC, 29 (80.6%) were treated on an every-3-week basis, and 7 (19.4%) received “dose-dense” AC every two weeks. Of these 7 patients, 4 received pegfilgrastim and 2 received filgrastim during pregnancy. Three patients (8.3%) received 12 cycles of weekly paclitaxel during pregnancy following AC. No patients received trastuzumab or endocrine therapy during pregnancy.
Maternal outcomes
Of the 68 term pregnancies, 1 was complicated by intrauterine growth restriction (< 10th percentile), 1 by gestational hypertension, 3 by gestational diabetes, and 3 by cervical shortening (defined as cervix < 3 cm at 22 weeks gestation). Other complications of pregnancy, such as preeclampsia and placental abruption, were not seen. Complications of chemotherapy, including anemia, neutropenia, and febrile neutropenia, were rare, and not more common with dose-dense therapy. One patient required a blood transfusion for anemia. A total of 13 patients (36.1%) treated with chemotherapy developed treatment-related neutropenia; but most cases were mild, with absolute neutrophil counts (ANC) >1000. One patient developed febrile neutropenia and mycoplasma pneumonia requiring hospitalization.
There were very few additional treatment-related complications; specifically, no pulmonary emboli or prolonged wound infections were seen. One patient with Factor V Leiden had a superficial blood clot. One patient experienced intraoperative preterm contractions at 30 weeks’ gestation; she underwent successful tocolysis and was induced closer to term.
Fetal outcomes
A total of 68 of 74 patients delivered liveborn infants (Table 4). Over half of deliveries (37, 54.4%) were at < 37 weeks and thus were considered preterm. However, the majority of preterm deliveries (26, 70.2%) were planned in order to facilitate maternal therapy, e.g. continuation of chemotherapy. The remaining preterm deliveries (11, 29.7% of all preterm, 16.2% of all deliveries) were due to complications including spontaneous preterm labor or preterm premature rupture of membranes. Detailed birth information was available for 50 infants; missing information was from patients who delivered at outside hospitals. The rate of birth weight <10th percentile was 8.0%. All infants had Apgar scores ≥ 7 at five minutes.
Three patients gave birth to infants born with congenital anomalies. One infant was found to have a cleft palate; the mother had other risk factors including tobacco and opiate use, and there was no chemotherapy exposure during pregnancy (Shaw et al. 1996). One infant had an atrial septal defect noted prior to initiation of chemotherapy at 31 weeks, after completion of fetal cardiac development. One infant was born with multiple abnormalities (ventricular septal defect, club foot, and hypospadias); the VSD and club foot were noted prior to initiating breast cancer therapy at 20 weeks, and hypospadias was additionally seen at delivery.
Discussion
In this cohort of patients with PABC, contemporary therapies for breast cancer including “dose-dense” scheduling, taxane chemotherapy, growth factor support, immediate breast reconstruction, and sentinel lymph node biopsy, were utilized without significant rates of adverse maternal or fetal events. There was a low rate of maternal complications, and the overall rate of fetal abnormalities, 4.4%, was consistent with expected population rates (Parker et al. 2010). This series is one of the most modern cohorts of PABC patients in the current literature, with the majority of patients receiving their diagnosis during or after the year 2005.
Consistent with prior reports, and likely due to the young age of the patients, this PABC cohort was enriched for ER-negative tumors as well as BRCA mutations (Middleton et al. 2003; Elledge et al. 1993). However, patients’ clinicopathologic details did not differ greatly from those noted in other studies of non-pregnant young women diagnosed with breast cancer (Collins et al. 2012).
Almost all patients in the cohort underwent imaging to stage their disease while pregnant. Notably, nearly half of patients underwent mammography and over 10% underwent MRI scanning, with no apparent adverse effect on the fetus. The safety and feasibility of mammography during pregnancy have been reported (Kopans 1998; Yang et al. 2006), and it is unclear why rates of mammography were not higher in this population. The findings from this study support the safety of mammography during pregnancy; and suggest that MRI may have a role in select cases (Taylor et al. 2011).
Reports suggest that mastectomy or lumpectomy can be safely pursued at any point during a pregnancy with minimal risk to the fetus (Rosenkranz & Lucci 2005; Amant et al. 2010). However, first trimester surgery is often deferred, out of concern for higher risks of fetal complications (Moran et al. 2007). In this cohort, nearly one in five patients underwent surgery in the first trimester without apparent complications, suggesting the safety of surgical intervention during this time. Additionally, both sentinel lymph node biopsy and immediate reconstruction were utilized without apparent complication. Overall, very few surgical complications were observed, consistent with previous observations (Dominici et al. 2010). These data support the safety of contemporary surgical treatment paradigms in PABC, as long as practitioners are aware of the unique physiologic changes associated with pregnancy (Hill & Pickinpaugh 2008).
Although chemotherapy administration during the first trimester has been associated with risk of fetal defects, the use of certain chemotherapeutics in the second and third trimesters is generally considered safe without increase in the rates of fetal abnormalities (Loibl et al. 2012; Amant et al. 2010; Cardonick & Iacobucci 2004; Ring et al. 2005). The chemotherapy data presented in this study support the safety of administering traditional as well as more contemporary treatment regimens in this population. Dose-dense scheduling has an important role in modern adjuvant breast cancer treatment, however is not typically offered to women during pregnancy due to concerns regarding potential harm to the fetal bone marrow. A prior study of 10 pregnant patients treated with dose-dense AC found no difference in maternal or neonatal outcomes when compared with every three week dosing (Cardonick et al. 2012b). In this study, in the patients who received AC, including the significant minority who received a “dose-dense” schedule, there were no apparent short-term adverse effects on offspring.
Most prior studies evaluating chemotherapy in PABC have examined AC or FAC, but few studies have examined the safety of taxanes, which play an integral role in adjuvant chemotherapy regimens. In this cohort, 8.3% of patients who received AC also received 12 cycles of weekly paclitaxel during pregnancy without evident undesirable effects. To date, the use of taxanes in PABC has been reported primarily as case reports (Potluri et al. 2006; Nieto et al. 2006). In a recent review of this literature, it was noted that of 42 infants born to 40 patients exposed to taxanes during pregnancy, only one had a malformation possibly related to taxane use (Mir et al. 2010). Further expansion of this data is desired to confirm the safety of taxane-containing chemotherapy regimens after the first trimester.
In non-pregnant women, growth factors may be required during adjuvant chemotherapy, particularly with “dose-dense” schedules. There are few reports in the literature of patients receiving growth factors during pregnancy (Dale et al. 2003). Consistent with the prior publications, 6 patients in this study received growth factor support without apparent adverse effect on the fetus.
Although neither tamoxifen nor trastuzumab has been rigorously studied in pregnant patients, these important systemic agents are traditionally avoided in pregnancy out of concern for teratogenic effects. Case reports have described multiple fetal complications after prenatal exposures to these agents (Gottschalk et al. 2011; Braems et al. 2011; Witzel et al. 2008). Trastuzumab has been associated with oligohydramnios, and a boxed warning for teratogenicity has been issued, contraindicating the use of trastuzumab in pregnancy. As a short-term delay in the initiation of endocrine therapy likely does not adversely affect survival outcomes, particularly in early stage breast cancer, it is feasible to consider delayed initiation of tamoxifen until completion of pregnancy. However, given the growth kinetics of HER2 positive breast cancer, a delay in HER2-directed therapy may be more clinically significant and introduce potential risk of compromise in the care of these patients. Fortunately, current adjuvant regimens for HER2 positive breast cancer can begin with anthracycline-based chemotherapy, facilitating postponement of trastuzumab therapy until after delivery. Analysis of unintentional pregnancies during adjuvant trastuzumab clinical trials is in process (Azim et al. 2012), and an ongoing prospective study (MotHER pregnancy registry) is collecting data on pregnancies complicated by trastuzumab exposure.
In general, increased rates of maternal complications of pregnancy were not observed in this cohort, possibly reflecting early inclusion of a maternal-fetal medicine specialist in the multidisciplinary team. A notable finding was the observation that over half of deliveries occurred at < 37 weeks, and were considered preterm. In contrast, the current expected rate of preterm delivery in the United States is 12.2% (Martin et al. 2011). With the exception of one series suggesting rates of preterm delivery comparable to general population norms (Cardonick et al. 2010), most other published studies have also reported an increased risk of preterm delivery in patients treated with chemotherapy for PABC (Smith et al. 2001; Loibl et al. 2012; Van Calsteren et al. 2010). In this series, the majority of preterm deliveries were planned to facilitate maternal therapy, e.g. to allow continuation of chemotherapy. Only 16.2% experienced unplanned preterm delivery, a figure more consistent with national averages for non-PABC patients.
The question of planned premature delivery deserves examination. Although preterm delivery in this cohort did not appear to result in increased harm to the fetus, recent obstetrical data has suggested even late preterm delivery (34–37 weeks) or near term delivery (37–39 weeks) can be associated with adverse outcomes in the fetus (Hibbard et al. 2010; Shapiro-Mendoza et al. 2008). In addition, a recent evaluation of children exposed to chemotherapy in utero has noted lower cognitive development for those born preterm than for those born full term (Amant et al. 2012). Given the apparent safety of chemotherapy during pregnancy, especially in the third trimester, the risks of late preterm delivery must be carefully considered when planning the timing of delivery. In these situations, a careful discussion is encouraged between the patient, the maternal-fetal medicine specialist, and the medical oncologist so that delivery timing minimizes risks to both mother and fetus.
Strengths of this study include utilization of a large academic comprehensive cancer center, and evaluation of a sizeable number of pregnant breast cancer patients treated with more contemporary treatment regimens than have been previously published. In addition, a systematic approach was used to assemble the cohort rather than solely relying on physician recall or patient self-enrollment, eliminating a source of bias. Finally, the majority of patients were treated for their breast cancer and delivered their infants at the same institution, allowing for data capture for peripartum as well as maternal outcomes.
A limitation of this study is the lack of follow-up data in exposed infants; data is limited to in utero and perinatal outcomes. Obtaining retrospective follow-up data is complicated by loss to follow-up and limitations of self-reported data. However, prospective long-term follow-up studies have generally demonstrated favorable outcomes in exposed offspring (Aviles & Neri 2001; Hahn et al. 2006). Another limitation of this study is sample size; while this cohort is large compared to other published cohorts of PABC, the sample size is small in absolute terms, making it difficult to generate definitive conclusions. In addition, the study was limited to women treated in a large academic tertiary care center, which introduces the possibility of selection bias. Data on socioeconomic status was not available, but it is possible that a higher degree of social and financial support may have impacted not only treatment choices but also patient outcomes.
This retrospective study of PABC demonstrates the feasibility of optimal treatment through multidisciplinary care team management. Continued prospective data collection and case series publication may improve comfort with using contemporary treatment paradigms to care for women in the difficult situation of having been diagnosed with breast cancer while pregnant. When making treatment decisions for these patients, attention to multidisciplinary team management is necessary to appropriately balance perinatal care of mother and infant. Further data collection and investigation will improve understanding of and treatment paradigms for breast cancer diagnosed during pregnancy.
References
Amant F, Deckers S, Van Calsteren K, Loibl S, Halaska M, Brepoels L, Beijnen J, Cardoso F, Gentilini O, Lagae L, et al.: Breast cancer in pregnancy: recommendations of an international consensus meeting. Eur J Cancer 2010, 46(18):3158-3168. 10.1016/j.ejca.2010.09.010
Amant F, Van Calsteren K, Halaska MJ, Gziri MM, Hui W, Lagae L, Willemsen MA, Kapusta L, Van Calster B, Wouters H, et al.: Long-term cognitive and cardiac outcomes after prenatal exposure to chemotherapy in children aged 18 months or older: an observational study. Lancet Oncol 2012, 13(3):256-264. 10.1016/S1470-2045(11)70363-1
Andersson TM, Johansson AL, Hsieh CC, Cnattingius S, Lambe M: Increasing incidence of pregnancy-associated breast cancer in Sweden. Obstet Gynecol 2009, 114(3):568-572. 10.1097/AOG.0b013e3181b19154
Aviles A, Neri N: Hematological malignancies and pregnancy: a final report of 84 children who received chemotherapy in utero. Clin Lymphoma 2001, 2(3):173-177. 10.3816/CLM.2001.n.023
Azim HA Jr, Metzger-Filho O, de Azambuja E, Loibl S, Focant F, Gresko E, Arfi M, Piccart-Gebhart M: Pregnancy occurring during or following adjuvant trastuzumab in patients enrolled in the HERA trial (BIG 01–01). Breast Cancer Res Treat 2012, 133(1):387-391. 10.1007/s10549-012-1996-6
Borges VF, Schedin PJ: Pregnancy-associated breast cancer: an entity needing refinement of the definition. Cancer 2011, 118(13):3226-3228.
Braems G, Denys H, De Wever O, Cocquyt V, Van den Broecke R: Use of tamoxifen before and during pregnancy. Oncologist 2011, 16(11):1547-1551. 10.1634/theoncologist.2011-0121
Cardonick E, Iacobucci A: Use of chemotherapy during human pregnancy. Lancet Oncol 2004, 5(5):283-291. 10.1016/S1470-2045(04)01466-4
Cardonick E, Usmani A, Ghaffar S: Perinatal outcomes of a pregnancy complicated by cancer, including neonatal follow-up after in utero exposure to chemotherapy: results of an international registry. Am J Clin Oncol 2010, 33(3):221-228.
Cardonick E, Bhat A, Gilmandyar D, Somer R: Maternal and fetal outcomes of taxane chemotherapy in breast and ovarian cancer during pregnancy: case series and review of the literature. Ann Oncol 2012a, 23(12):3016-3023. 10.1093/annonc/mds170
Cardonick E, Gilmandyar D, Somer RA: Maternal and neonatal outcomes of dose-dense chemotherapy for breast cancer in pregnancy. Obstet Gynecol 2012b, 120(6):1267-1272.
Collins LC, Marotti JD, Gelber S, Cole K, Ruddy K, Kereakoglow S, Brachtel EF, Schapira L, Come SE, Winer EP, et al.: Pathologic features and molecular phenotype by patient age in a large cohort of young women with breast cancer. Breast Cancer Res Treat 2012, 131(3):1061-1066. 10.1007/s10549-011-1872-9
Dale DC, Cottle TE, Fier CJ, Bolyard AA, Bonilla MA, Boxer LA, Cham B, Freedman MH, Kannourakis G, Kinsey SE, et al.: Severe chronic neutropenia: treatment and follow-up of patients in the severe chronic neutropenia international registry. Am J Hematol 2003, 72(2):82-93. 10.1002/ajh.10255
Dominici LS, Kuerer HM, Babiera G, Hahn KM, Perkins G, Middleton L, Ramirez MM, Yang W, Hortobagyi GN, Theriault RL, et al.: Wound complications from surgery in pregnancy-associated breast cancer (PABC). Breast Dis 2010, 31(1):1-5.
Elledge RM, Ciocca DR, Langone G, McGuire WL: Estrogen receptor, progesterone receptor, and HER-2/neu protein in breast cancers from pregnant patients. Cancer 1993, 71(8):2499-2506. 10.1002/1097-0142(19930415)71:8<2499::AID-CNCR2820710812>3.0.CO;2-S
Gottschalk I, Berg C, Harbeck N, Stressig R, Kozlowski P: Fetal renal insufficiency following trastuzumab treatment for breast cancer in pregnancy: case report und review of the current literature. Breast Care (Basel) 2011, 6(6):475-478. 10.1159/000335202
Hahn KM, Johnson PH, Gordon N, Kuerer H, Middleton L, Ramirez M, Yang W, Perkins G, Hortobagyi GN, Theriault RL: Treatment of pregnant breast cancer patients and outcomes of children exposed to chemotherapy in utero. Cancer 2006, 107(6):1219-1226. 10.1002/cncr.22081
Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, Hoffman M, Kominiarek MA, Reddy U, Bailit J, Branch DW, et al.: Respiratory morbidity in late preterm births. JAMA 2010, 304(4):419-425.
Hill CC, Pickinpaugh J: Physiologic changes in pregnancy. Surg Clin North Am 2008, 88(2):391-401. vii 10.1016/j.suc.2007.12.005
Kopans D: The altered breast: pregnancy, lactation, biopsy, mastectomy, radiation, and implants. In Breast Imaging, 2nd ed. Edited by: Kopans D. Philadelphia: Lippincott-Raven; 1998:445-447.
Litton JK, Theriault RL: Breast cancer and pregnancy: current concepts in diagnosis and treatment. Oncologist 2010, 15(12):1238-1247. 10.1634/theoncologist.2010-0262
Loibl S, Han SN, von Minckwitz G, Bontenbal M, Ring A, Giermek J, Fehm T, Van Calsteren K, Linn SC, Schlehe B, et al.: Treatment of breast cancer during pregnancy: an observational study. Lancet Oncol 2012, 13(9):887-896. 10.1016/S1470-2045(12)70261-9
Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, Wilson EC: Births: final data for 2009. Natl Vital Stat Rep 2011, 60(1):1-70.
Middleton LP, Amin M, Gwyn K, Theriault R, Sahin A: Breast carcinoma in pregnant women: assessment of clinicopathologic and immunohistochemical features. Cancer 2003, 98(5):1055-1060. 10.1002/cncr.11614
Mir O, Berveiller P, Ropert S, Goffinet F, Pons G, Treluyer JM, Goldwasser F: Emerging therapeutic options for breast cancer chemotherapy during pregnancy. Ann Oncol 2008, 19(4):607-613.
Mir O, Berveiller P, Goffinet F, Treluyer JM, Serreau R, Goldwasser F, Rouzier R: Taxanes for breast cancer during pregnancy: a systematic review. Ann Oncol 2010, 21(2):425-426. 10.1093/annonc/mdp517
Moran BJ, Yano H, Al Zahir N, Farquharson M: Conflicting priorities in surgical intervention for cancer in pregnancy. Lancet Oncol 2007, 8(6):536-544. 10.1016/S1470-2045(07)70171-7
Nieto Y, Santisteban M, Aramendia JM, Fernandez-Hidalgo O, Garcia-Manero M, Lopez G: Docetaxel administered during pregnancy for inflammatory breast carcinoma. Clin Breast Cancer 2006, 6(6):533-534. 10.3816/CBC.2006.n.008
Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, et al.: Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol 2010, 88(12):1008-1016. 10.1002/bdra.20735
Potluri V, Lewis D, Burton GV: Chemotherapy with taxanes in breast cancer during pregnancy: case report and review of the literature. Clin Breast Cancer 2006, 7(2):167-170. 10.3816/CBC.2006.n.029
Ring AE, Smith IE, Jones A, Shannon C, Galani E, Ellis PA: Chemotherapy for breast cancer during pregnancy: an 18-year experience from five London teaching hospitals. J Clin Oncol 2005, 23(18):4192-4197. 10.1200/JCO.2005.03.038
Rosenkranz KM, Lucci A: Surgical treatment of pregnancy associated breast cancer. Breast Dis 2005, 23: 87-93.
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J, Declercq E: Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics 2008, 121(2):e223-e232. 10.1542/peds.2006-3629
Shaw GM, Wasserman CR, Lammer EJ, O’Malley CD, Murray JC, Basart AM, Tolarova MM: Orofacial clefts, parental cigarette smoking, and transforming growth factor-alpha gene variants. Am J Hum Genet 1996, 58(3):551-561.
Smith LH, Dalrymple JL, Leiserowitz GS, Danielsen B, Gilbert WM: Obstetrical deliveries associated with maternal malignancy in California, 1992 through 1997. Am J Obstet Gynecol 2001, 184(7):1504-1512. discussion 1512–1503 10.1067/mob.2001.114867
Taylor D, Lazberger J, Ives A, Wylie E, Saunders C: Reducing delay in the diagnosis of pregnancy-associated breast cancer: how imaging can help us. J Med Imaging Radiat Oncol 2011, 55(1):33-42. 10.1111/j.1754-9485.2010.02227.x
Van Calsteren K, Heyns L, De Smet F, Van Eycken L, Gziri MM, Van Gemert W, Halaska M, Vergote I, Ottevanger N, Amant F: Cancer during pregnancy: an analysis of 215 patients emphasizing the obstetrical and the neonatal outcomes. J Clin Oncol 2010, 28(4):683-689. 10.1200/JCO.2009.23.2801
Witzel ID, Muller V, Harps E, Janicke F, Dewit M: Trastuzumab in pregnancy associated with poor fetal outcome. Ann Oncol 2008, 19(1):191-192.
Yang WT, Dryden MJ, Gwyn K, Whitman GJ, Theriault R: Imaging of breast cancer diagnosed and treated with chemotherapy during pregnancy. Radiology 2006, 239(1):52-60. 10.1148/radiol.2391050083
Acknowledgements
Financial support for this study was from institutional funding.
Precis
Treatment of pregnancy associated breast cancer using contemporary algorithms does not appear to increase maternal or fetal adverse outcomes. Multidisciplinary care is of great importance in the management of pregnancy associated breast cancer.
Previous presentations
This manuscript contains original material. A portion of the work described herein was presented in an abstract at the 2011 34th Annual San Antonio Breast Cancer Symposium.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have no financial conflicts or disclosures to report.
Authors’ contributions
JM participated in collection and assembly of data, data analysis and interpretation, and manuscript writing. KE participated in study conception and design, provision of study material or patients, data analysis and interpretation, and manuscript writing. KZC participated in study conception and design, provision of study material or patients, data analysis and interpretation, and manuscript writing. LS participated in provision of study material or patients, data analysis and interpretation, and manuscript writing. NT participated in provision of study material or patients, data analysis and interpretation, and manuscript writing. SG participated in study conception and design, data analysis and interpretation, and manuscript writing. SK participated in collection and assembly of data, and manuscript writing. AP participated in study conception and design, provision of study material or patients, data analysis and interpretation, and manuscript writing. EM participated in study conception and design, provision of study material or patients, collection and assembly of data, data analysis and interpretation, and manuscript writing. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Meisel, J.L., Economy, K.E., Calvillo, K.Z. et al. Contemporary multidisciplinary treatment of pregnancy-associated breast cancer. SpringerPlus 2, 297 (2013). https://doi.org/10.1186/2193-1801-2-297
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2193-1801-2-297