Abstract
Purpose
Taxane-based chemotherapy is the primary treatment for premenopausal breast cancer. Although being inconsistent, research suggests that variant alleles alter pharmacokinetics through reduced function of OATP transporters (limiting hepatic uptake), CYP-450 enzymes (hampering drug metabolism), and ABC transporters (decreasing clearance). Reduced function of DNA repair enzymes may hamper effectiveness through dose-limiting toxicities. We investigated whether single-nucleotide polymorphisms (SNPs) were associated with breast cancer recurrence or mortality in premenopausal women diagnosed with breast cancer.
Methods
We conducted a population-based cohort study of premenopausal women diagnosed with non-distant metastatic breast cancer in Denmark during 2007‒2011, when guidelines recommended adjuvant combination chemotherapy (taxanes, anthracyclines, and cyclophosphamide). Using archived formalin-fixed paraffin-embedded primary tumor tissue, we genotyped 26 SNPs using TaqMan assays. Danish health registries provided data on breast cancer recurrence (through September 25, 2017) and death (through December 31, 2019). We fit Cox regression models to calculate crude hazard ratios (HRs) and 95% confidence intervals (CIs) for recurrence and mortality across genotypes.
Results
Among 2,262 women, 249 experienced recurrence (cumulative incidence: 13%) and 259 died (cumulative incidence: 16%) during follow-up (median 7.0 and 10.1 years, respectively). Mortality was increased in variant carriers of GSTP1 rs1138272 (HR: 1.30, 95% CI 0.95–1.78) and CYP3A rs10273424 (HR: 1.33, 95% CI 0.98–1.81). SLCO1B1 rs2306283 (encoding OATP1B1) variant carriers had decreased recurrence (HR: 0.82, 95% CI 0.64–1.07) and mortality (HR: 0.77, 95% CI 0.60–0.98).
Conclusion
Docetaxel effectiveness was influenced by SNPs in GSTP1, CYP3A, and SLCO1B1 in premenopausal women with non-distant metastatic breast cancer, likely related to altered docetaxel pharmacokinetics. These SNPs may help determine individual benefit from taxane-based chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In 2020, more than 2.3 million women were diagnosed with breast cancer worldwide, making female breast cancer the most frequent non-skin malignancy in women [1]. About one-third of breast cancer diagnoses occur in premenopausal women [2]. These women are usually recommended taxane-based chemotherapy as a primary treatment. Advances in breast cancer diagnosis and increasingly effective treatments (including the introduction of taxanes) have enlarged the pool of breast cancer survivors [3,4,5]. Still, mortality measured up to 15 years after premenopausal breast cancer ranges from 11 to 14% in high-income countries [2, 6]. Reasons for variation in individual treatment effectiveness are likely multifactorial. Studies suggest that taxane effectiveness may be up- or down-regulated by inherited single-nucleotide polymorphisms (SNPs) in genes involved in taxane transport and metabolism [7, 8].
The metabolism of taxanes—docetaxel and paclitaxel—occurs primarily in the liver. Taxane metabolites are eliminated through the bile. Solute carrier anion transporters (mainly OATP1B1, encoded by the polymorphic SLCO1B1) transport taxanes into hepatocytes, where they are metabolized by cytochrome P450 (CYP) enzymes [9]. Our study focused only on docetaxel, which is mainly metabolized by CYP3A4 (encoded by CYP3A4) and CYP3A5 (encoded by CYP3A5) into its main metabolites and conjugated by glutathione-S-transferase P1 (encoded by GSTP1). Each of these enzymes is encoded by polymorphic genes. Taxanes are excreted into bile by efflux proteins encoded by the ATP-binding cassette (ABC) transporters. For docetaxel, this is mainly done by proteins encoded by the polymorphic genes ABCB1, ABCC2, ABCG2, and ABCC1 [10]. SNPs in DNA repair genes, e.g., Eph-receptor A (EPHA) and excision repair cross-complementing genes (ERCC), may be associated with taxane toxicities [11], potentially leading to treatment discontinuation and reduced treatment effectiveness.
Research suggests that clinical outcomes (survival, progression-free survival, and tumor response) in cancer patients treated with taxanes may depend on genetic differences in taxane transporters [12, 13] and/or metabolizing enzymes [13, 14]. However, findings are rarely replicated [15, 16] and available studies have several limitations—including small sample size, population stratification, and different treatment schedules. As such, it is not possible to determine the impact of these genetic differences on taxane effectiveness from the existing literature.
We therefore investigated the association of SNPs that may influence taxane metabolism and transport with breast cancer recurrence and mortality in a large population-based cohort of premenopausal women diagnosed with non-distant metastatic breast cancer treated with docetaxel-based adjuvant chemotherapy.
Materials and methods
Setting and design
We conducted this nationwide population-based cohort study in Denmark. Denmark has a free tax-supported health care system [17]. The civil personal registration number, assigned to all residents upon birth or immigration, allows individual-level data linkage across Danish administrative and health registries [17]. In Denmark, all diagnostic surgical and biopsy tissue specimens are stored permanently as primary formalin-fixed paraffin-embedded (FFPE) tissue blocks at local pathology departments and registered in the Danish National Pathology Registry [18]. The Danish Breast Cancer Group (DBCG) is responsible for clinical guidelines on breast cancer diagnosis and treatment in Denmark. The DBCG clinical database records clinical and follow-up data for all Danish patients with invasive breast tumors [19], including data for up to 10 years of active follow-up for recurrence [20]. The DBCG registers breast cancer patients through an electronic reporting system accessible to all Danish pathology departments. This database is supplemented with data from other medical registries (e.g., the Danish National Pathology Registry). Subsequent clinical data from follow-up examinations also are added to the database. Until 2016, women diagnosed with breast cancer in Denmark were followed up first with semi-annual clinical exams for five years and then with annual exams during the following five years. Since 2016, patients have been able to choose among patient-led, nurse-led, or fixed annual follow-up exams. All women are offered mammography, ultrasound screening, and open access to a breast cancer unit for 10 years after a breast cancer diagnosis [21].
Study cohort
We nested our study in the Predictors of Breast Cancer Recurrence (ProBe CaRe) cohort, which is described in greater detail elsewhere [22]. Briefly, the ProBe CaRe cohort includes premenopausal Danish women diagnosed with incident non-distant metastatic breast cancer during 2002–2011. We restricted the cohort to women diagnosed with breast cancer after implementation of docetaxel in combination with cyclophosphamide and sometimes epirubicin as guideline chemotherapy in Denmark (January 01, 2007). The cohort was further restricted to patients who were 18–55 years at diagnosis, who received chemotherapy, and who had FFPE blocks available in the pathology archives. Finally, we excluded women who experienced a recurrence or were lost to follow-up during the first six months after diagnosis. The study flowchart is provided in the Supplementary material (Fig. S1).
Tissue procurement, DNA extraction, and genotyping
Procedures for collection of FFPE tumor blocks, preparation of the tumor tissue, and DNA extraction are described in detail elsewhere [23]. Based on a comprehensive review of the taxane pharmacogenetic literature and underlying biology, we identified 26 candidate SNPs. SNPs were considered candidates if (1) located in genes encoding proteins involved in taxane metabolism or transport, (2) previous studies suggested their biologically plausible role in taxane pharmacokinetics or effectiveness, or (3) they were associated with taxane toxicities (primarily neuropathy). A list of genotyped variants is presented in Table 2. Seven of these SNPs had been genotyped previously, as described elsewhere [23]. The remaining 19 SNPs were genotyped using commercially available TaqMan assays on a StepOne Plus real-time instrument (Applied Biosystems, Thermo Fisher Scientific, Foster City, California, USA) in accordance with the manufacturer’s protocol. For TaqMan assays, 20 ng of purified DNA extracted from FFPE tissues were amplified in 10µL PCR. The PCR were incubated at 60 °C for 30 s and 95 °C for 10 min and then cycled 50 times between 15-s incubations at 95 °C and 60-s incubations at 60 °C. Genotypes were classified based on TaqMan VIC/FAM intensity values using the auto-call feature of QuantStudio Software V1.3. Genotype results were manually inspected, and acceptance was overridden manually if irregular amplification curves were observed. We calculated expected genotype frequencies under Hardy–Weinberg Equilibrium (HWE) and compared them with observed frequencies both visually and by applying a traditional test for HWE. In addition, we compared allele frequencies between the study cohort and benchmarks reported for female European non-Finnish cohorts in the Genome Aggregation Database (gnomAD) [24]. For each SNP, we primarily classified each woman as (1) wildtype when she carried two normal alleles, (2) variant carriers (including both hetero- and homozygotes), or (3) as heterozygote or homozygote variant carriers.
Data collection from Danish health registries
From the DBCG clinical database, we collected information on patient age at diagnosis, tumor characteristics (hormone receptor status, pathological grade, number of positive lymph nodes, and tumor size), cancer treatment (surgery type, intention-to-treat radiotherapy, adjuvant chemotherapy, and endocrine therapy), and dates of recurrences or second primary malignancies. From the Cause of Death Registry, we collected dates and causes of death, and from the Danish National Patient Registry we collected data on comorbid conditions diagnosed up to 10 years before the breast cancer diagnosis [25, 26].
Outcomes
We used breast cancer recurrence and all-cause mortality as outcomes of taxane effectiveness. We adopted the DBCG definition of recurrence, which encompasses locoregional recurrence (tumor growth in the surgical scar, the ipsilateral breast, or regional lymph nodes), distant recurrence, or contralateral breast cancers diagnosed up to 10 years after initial breast cancer treatment [20]. Diagnosis of recurrence is either based on clinical assessment, pathological assessment, imaging, or a combination of these. We examined all-cause mortality, assuming breast cancer to be the most likely underlying or contributing cause of death in our young study cohort. We also examined breast cancer-specific mortality (BCSM) in sensitivity analyses, defined by deaths with breast cancer (ICD-10: C50) as the underlying or contributory cause of death.
Other covariates
Comorbidities were summarized using the Charlson Comorbidity Index [27] and categorized as none, 1–2, or ≥ 3 comorbidities (Supplemental Table S1). We derived cancer stage (categorized as stage I–III according to the TNM staging system [28]). Estrogen receptor (ER) status was a composite variable incorporating both negative and positive ER statuses and receipt of endocrine therapy. Grades 1–3 were assigned to lobular and ductal tumors; other tumors were not graded. Data on treatments included surgical procedure and intention-to-treat radiotherapy. Breast cancers were considered triple negative if tumors were ER–, human epidermal growth factor receptor 2 was negative, and information on progesterone receptor was either negative or missing.
Statistical analyses
We started follow-up six months after the date of breast cancer surgery (date of diagnosis), to approximate the end of chemotherapy treatment. In analyses of recurrence, we censored follow-up upon death, emigration, diagnosis with new primary malignancy, last visit if lost to follow-up exams, end of the DBCG follow-up protocol (maximum 10 years), or end of available data (September 25, 2017). When examining mortality, longer available follow-up time in the Cause of Death registry allowed us to extend the follow-up period. Thus, mortality follow-up continued until the date of death, emigration, or end of data availability on December 31, 2019. We computed cumulative incidences of recurrence and death, considering death as a competing risk when examining recurrence. We used cause-specific Cox regression models to compute unadjusted hazard ratios (HRs) of recurrence and mortality for each SNP.
We also stratified all models by ER status and stage to evaluate effect measure modification by these factors. To account for potential underreporting of recurrence [29], we performed a sensitivity analysis considering recurrences to include BCSM in women not registered with a recurrence. To test the robustness of our mortality model, we restricted an analysis to BCSM. We used SAS 9.4 for all analyses (Cary, NC).
Results
A total of 2,979 women were diagnosed during the 2007–2011 period in the ProBe CaRe cohort. The final study cohort included 2,262 women (Supplemental Fig. S1). Characteristics of the study cohort are presented in Table 1. More than half of the women in the study cohort were aged 45–55 years, 78% had ER+ tumors, 11% had triple-negative tumors, 56% were stage II, and 60% had breast-conserving surgery followed by intention-to-treat radiotherapy. One in ten patients had at least one prevalent comorbidity at the time of breast cancer diagnosis. Overall, 21 SNPs were successfully genotyped with call rates ≥ 95% and five SNPs were excluded because of low call rates (ABCB1 rs10248420, CYP1A1 rs1048943, TRPV1 rs879207, ARHGEF10 rs9657362, and EPHA8 rs209709). Information on call rates is provided in Table 2. For all included SNPs, the observed minor allele frequencies were consistent with those reported for European non-Finnish female populations, and the observed genotype frequencies were similar to the expected frequencies predicted under HWE (Table 2).
During 10 years of follow-up (median: 7.0 years, IQR: 5.8–8.4 years), 249 women in our study cohort experienced a recurrence (cumulative incidence: 13.2%, 95% CI 11.5–15.0%). During 13 years of follow-up (median 10.1, IQR: 8.9–11.5), we observed 259 deaths (cumulative incidence: 16.0%, 95% CI 11.9–11.5%). Of these, 226 deaths were attributed to breast cancer (cumulative incidence: 12.6%, 95% CI 9.5–16.1%). Among the 33 deaths from other causes, 16 women died from other cancers, 11 died from other organ diseases or suicide, and six deaths were from unspecified causes.
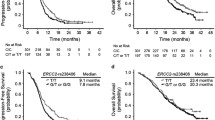
Figures 1 and 2 present SNP frequencies with HRs (of breast cancer recurrence and mortality, respectively). SLCO1B1 rs2306283 was weakly associated with a reduced rate of recurrence (HR: 0.82, 95% CI 0.64–1.07) and mortality (HR: 0.77, 95% CI 0.60–0.98). We also observed minor associations between GSTP1 rs1138272 and recurrence (HR: 1.16, 95% CI 0.84–1.62) and mortality (HR: 1.30, 95% CI 0.95–1.78). In contrast, we observed decreased recurrence (HR: 0.88, 95% CI 0.68–1.15) and mortality (HR: 0.80, 95% CI 0.62–1.03) among CYP1B1 rs1056836 variant carriers. For some SNPs, we observed associations with mortality, but not recurrence. Mortality was decreased in variant carriers of the ABC transporters ABCB1 rs1128503 (HR: 0.79, 95% CI 0.61–1.02), ABCB1 rs2032582 (HR: 0.79, 95% CI 0.61–1.02), and ABCC2 rs12762549 (HR: 0.82, 95% CI 0.63–1.07). In contrast, we observed increased mortality in variant carriers of CYP3A rs10273424 (HR: 1.33, 95% CI: 0.98–1.81). Analysis of SNPs encoding DNA repair genes suggested lower mortality in variant carriers of ERCC1 rs11615 (HR: 0.87, 95% CI 0.68–1.12) and rs3212986 (HR: 0.86, 95% CI 0.67–1.11). We observed similar findings when we distinguished homozygote and heterozygote variant allele carriers.
When we pooled recurrences and BCSM as a single outcome, the HR slightly increased in variant carriers of GSTP1 rs1138272 (HR: 1.23, 95% CI 0.92–1.64). In general, the estimates were similar in the analyses of all-cause mortality and BCSM, although the HR decreased for SLCO1B1 rs2306283 (HR: 0.71, 95% CI 0.55–0.93) (Supplemental Tables S2–S3). Our findings were similar when we stratified by ER status and stage (Supplemental Tables S4–S5).
Discussion
In this cohort of premenopausal women with non-distant metastatic breast cancer, carriers of the SLCO1B1 rs2306283 variant had decreased recurrence and mortality rates compared with wildtypes. In contrast, we found increased mortality rates in GSTP1 rs1138272 variant and CYP3A rs10273424 variant carriers. We did not observe any effect measure modification by ER status and stage.
Reduced function alleles of SLCO1B1 are associated with docetaxel clearance in mice [30] but have not been associated with altered docetaxel clearance in humans [9, 30]. Longer systemic paclitaxel exposure has been observed among breast cancer patients carrying the rs4149056 and rs2306283 variants [31]. In a similar fashion, the apparent increased effectiveness of docetaxel that we observed in women with the rs2306283 variant may be attributable to reduced function of OATP1B1 and associated increased docetaxel plasma concentrations.
Polymorphisms in CYPs most often confer decreased enzyme activity [32, 33]. Theoretically, this would lead to increased docetaxel exposure and higher clinical efficacy. Yet our results suggested increased mortality, which also has been reported for other CYP3A4 SNPs [14]. Currently, we do not have an explanation for these unexpected findings. Because CYP3A rs10273424 is an intronic variant, it could exert a causal effect via modified splicing or linkage disequilibrium. We considered it relevant to include in the current study as it has been associated with lower estrogen levels and increased breast cancer risk in premenopausal women [34].
Our observed decreased risk of recurrence and mortality among carriers of CYP1B1 rs1056836 is consistent with some published research [35]. A recent study of 76 women (51% premenopausal) with triple-negative breast cancer undergoing adjuvant taxane, doxorubicin, and cyclophosphamide therapy found higher risk of recurrence in wildtypes (HR: 2.5, 95% CI 1.10–5.66), compatible with the favorable impact of variants observed in our study [35]. In a study of 58 Indian patients with advanced breast cancer (mixed pre- and postmenopausal), Tulsyan et al. [36] reported an association between CYP3A5 rs776746 and complete or partial response to neo-adjuvant taxane treatment. We did not detect any associations between rs776746 and clinical outcomes in the adjuvant setting. GSTP1 overexpression has been associated with lower breast tumor reduction among patients treated with neo-adjuvant docetaxel or paclitaxel [37]. The mechanisms are yet unclear but could be reduced enzyme activity of GSTP1. Some studies report no associations between GSTP1 polymorphisms and taxane-induced neuropathies [38, 39] and a meta-analysis by Ma et al. [40] found no association between GSTP1 polymorphisms and breast cancer tumor response or overall survival. These studies were likely underpowered. In a Danish trial including 150 women with breast cancer GSTP1 rs1138272 has been associated with docetaxel-induced peripheral neuropathy [41]. Whether and how this relates to our findings of increased recurrence and mortality are unclear, as this theoretically points toward increased the drug exposure.
A meta-analysis by Chen et al. [12], including prospective studies of taxane-treated breast, lung, ovarian, gastric, and head/neck cancer patients, reported better survival in ABCB1 rs1128503 variant carriers, consistent with our findings [12]. Another meta-analysis including case–control studies did not detect such associations in breast cancer patients, but had limited precision [42]. In the study by Chen et al. [12], no overall associations were found for ABCB1 rs1045642, but poor overall survival was found in European populations homozygote for the variant allele, consistent with the increased mortality observed in our study.
In other cancers, the ERCC1 rs11625 wildtype and heterozygotes have been linked with toxicities after oxaliplatin-based chemotherapy [43], and similar to our findings, improved docetaxel effectiveness has been observed in variant carriers [44]. The previous studies were limited by small sample size (fewer than 62 patients), precluding definitive conclusions on the association of ERCC1 SNPs and treatment effectiveness.
Our study has several noteworthy strengths. We examined the association between SNPs and docetaxel effectiveness in a population-based cohort of exclusively premenopausal women, included registry data with high validity and completeness [45], and systematically archived tumor tissue. Tumor tissue was collected at the time of primary breast cancer-directed surgery, thereby avoiding left truncation, selection, and immortal time bias. A key concern when using DNA extracted from FFPE tumors is whether the derived genotypes are representative of the germline, due to potential somatic genetic alterations. Previous studies show high genotype concordance between both FFPE breast tumors and FFPE normal lymph nodes [46] and between FFPE breast tumors and FFPE normal lymph nodes and whole blood [47]. We used tumor-infiltrated tissue, which has been suggested to be susceptible to genotyping error by loss of heterozygosity at certain genetic loci [48]. However, quantitative assessment of the influence of this in studies of CYP2D6 rs3892097 showed minor impact of genotype misclassification when investigating breast cancer survival [47].
In four of the excluded SNPs (ABCB1 rs10248420, CYP1A1 rs1048943, ARHGEF10 rs9657362, and EPHA8 rs209709), genotype clusters overlapped widely, which could indicate poor performance of the assay in FFPE-extracted DNA. Hence, no manual adjustment was performed, and these SNPs were disregarded (along with one SNPs with call rates < 95%). This ensured high-quality genotyping data. We did not exclude SNPs with statistical evidence of departure from HWE. In studies with a large sample size, any deviation from HWE is likely to have minor practical importance [49, 50]. In the current study, congruity between the observed frequencies and those expected under HWE were reasonable, even in the SNPs departing from HWE.
Our study also had several limitations. First, we investigated the influence of single SNPs on taxane metabolism, precluding the evaluation of the synergistic effect of all SNPs. For example, the reduced activity of one ABC transporter might be offset by increased activity of other ABC family members. Second, we lacked detailed information on chemotherapy treatment, and while we know the women in our cohort received a minimum of one treatment cycle, dosing and information on chemotherapy type were not available. Instead, we restricted the cohort to the period when guideline treatment was docetaxel based and dosing was guided by body surface area. Third, we had no information on potential dose capping or early discontinuation, which may have been due to treatment-associated toxicities. Treatment modifications may be differentially distributed across genotypes and may hamper treatment benefits. Fourth, the associations observed in this study pertain to docetaxel administered in combination with cyclophosphamide and sometimes epirubicin, and not docetaxel monotherapy. Fifth, some SNPs were singled out based on findings from earlier studies that used other combinations of taxane-based chemotherapy [15, 35, 51,52,53,54,55,56]. As our study was based on routine clinical care data, our findings warrant confirmation in randomized clinical trials before genotyping can be used to guide taxane effectiveness in routine clinical practice.
Another concern is that despite the high validity and completeness of the DBCG clinical database, information on recurrences was not complete. A previous study reported a positive predictive value of 100% for recurrences in the DBCG, but a completeness of 70% using medical records as a reference standard [29]. We expected misclassification of recurrences to be non-differential across SNPs, and our sensitivity analysis pooling recurrence and BCSM suggested minor differential misclassification of recurrences, as the expanded analysis had little influence on two SNPs.
Conclusion
This study, focusing on premenopausal non-distant metastatic breast cancer patients treated with taxane chemotherapy, demonstrated that some SNPs involved in docetaxel pharmacogenomics may impact breast cancer recurrence and/or mortality, especially SLCO1B1 rs2306283, GSTP1 rs1138272, and CYP3A rs10273424. Findings from this study merit further investigation. They will be used in future work using multiple pathway analysis [23, 57] to capture the net effect of these SNPs. Also, future clinical trials are needed to elucidate whether genomic testing could guide dosing of taxane-based therapy to reduce inter-individual variability in effectiveness.
Change history
25 May 2022
The Given name and Family name of five authors “Cathrine Fonnesbech Hjorth, Timothy Lee Lash, Henrik Toft Sørensen, Thomas Patrick Ahern and Tore Bjerregaard Stage” are corrected.
References
International Agency for Research on Cancer (2020) Latest global cancer data: Cancer burden rises to 19.3 million new cases. World Health Organization, Geneva
Heer E, Harper A, Escandor N et al (2020) Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Glob Health 8:e1027–e1037. https://doi.org/10.1016/S2214-109X(20)30215-1
Peto R, Boreham J, Clarke M et al (2000) UK and USA breast cancer deaths down 25% in year 2000 at ages 20–69 years. Lancet Lond Engl 355:1822. https://doi.org/10.1016/S0140-6736(00)02277-7
Cianfrocca M (2008) Overcoming recurrence risk: extended adjuvant endocrine therapy. Clin Breast Cancer 8:493–500. https://doi.org/10.3816/CBC.2008.n.059
Park J-H, Anderson WF, Gail MH (2015) Improvements in US breast cancer survival and proportion explained by tumor size and estrogen-receptor status. J Clin Oncol Off J Am Soc Clin Oncol 33:2870–2876. https://doi.org/10.1200/JCO.2014.59.9191
Hjorth CF, Damkier P, Ejlertsen B et al (2021) Socioeconomic position and prognosis in premenopausal breast cancer: a population-based cohort study in Denmark. BMC Med. https://doi.org/10.1186/s12916-021-02108-z
Baker SD, Sparreboom A, Verweij J (2006) Clinical pharmacokinetics of docetaxel : recent developments. Clin Pharmacokinet 45:235–252. https://doi.org/10.2165/00003088-200645030-00002
Palmirotta R, Carella C, Silvestris E et al (2018) SNPs in predicting clinical efficacy and toxicity of chemotherapy: walking through the quicksand. Oncotarget 9:25355–25382. https://doi.org/10.18632/oncotarget.25256
Baker SD, Verweij J, Cusatis GA et al (2009) Pharmacogenetic pathway analysis of docetaxel elimination. Clin Pharmacol Ther 85:155–163. https://doi.org/10.1038/clpt.2008.95
Oshiro C, Marsh S, McLeod H et al (2009) Taxane pathway. Pharmacogenet Genomics 19:979–983. https://doi.org/10.1097/FPC.0b013e3283335277
Frederiks CN, Lam SW, Guchelaar HJ, Boven E (2015) Genetic polymorphisms and paclitaxel- or docetaxel-induced toxicities: a systematic review. Cancer Treat Rev 41:935–950. https://doi.org/10.1016/j.ctrv.2015.10.010
Chen Q, Lin W, Yang J et al (2021) Prognostic value of two polymorphisms, rs1045642 and rs1128503, in ABCB1 following taxane-based chemotherapy: a meta-analysis. Asian Pac J Cancer Prev APJCP 22:3–10. https://doi.org/10.31557/APJCP.2021.22.1.3
Kulma I, Boonprasert K, Na-Bangchang K (2019) Polymorphisms of genes encoding drug transporters or cytochrome P450 enzymes and association with clinical response in cancer patients: a systematic review. Cancer Chemother Pharmacol 84:959–975. https://doi.org/10.1007/s00280-019-03932-0
Assis J, Pereira D, Gomes M et al (2013) Influence of CYP3A4 genotypes in the outcome of serous ovarian cancer patients treated with first-line chemotherapy: implication of a CYP3A4 activity profile. Int J Clin Exp Med 6:552–561
Marsh S, Paul J, King CR et al (2007) Pharmacogenetic assessment of toxicity and outcome after platinum plus taxane chemotherapy in ovarian cancer: the Scottish Randomised Trial in Ovarian Cancer. J Clin Oncol Off J Am Soc Clin Oncol 25:4528–4535. https://doi.org/10.1200/JCO.2006.10.4752
Demurtas S, La Verde N, Rota S et al (2021) Single nucleotide polymorphisms to predict taxanes toxicities and effectiveness in cancer patients. Pharmacogenomics J. https://doi.org/10.1038/s41397-021-00227-7
Schmidt M, Pedersen L, Sørensen HT (2014) The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 29:541–549. https://doi.org/10.1007/s10654-014-9930-3
Erichsen R, Lash TL, Hamilton-Dutoit SJ et al (2010) Existing data sources for clinical epidemiology: the Danish National Pathology Registry and Data Bank. Clin Epidemiol 2:51–56
Jensen M-B, Laenkholm A-V, Offersen BV et al (2018) The clinical database and implementation of treatment guidelines by the Danish Breast Cancer Cooperative Group in 2007–2016. Acta Oncol 57:13–18. https://doi.org/10.1080/0284186X.2017.1404638
Christiansen P, Al-Suliman N, Bjerre K et al (2008) Recurrence pattern and prognosis in low-risk breast cancer patients–data from the DBCG 89-A programme. Acta Oncol Stockh Swed 47:691–703. https://doi.org/10.1080/02841860802056594
Saltbæk L, Horsboel TA, Offersen BV et al (2020) Patterns in detection of recurrence among patients treated for breast cancer. Breast Cancer Res Treat 184:365–373. https://doi.org/10.1007/s10549-020-05847-4
Collin LJ, Cronin-Fenton DP, Ahern TP et al (2018) Cohort profile: the predictors of breast cancer recurrence (ProBe CaRE) premenopausal breast cancer cohort study in Denmark. BMJ Open. https://doi.org/10.1136/bmjopen-2018-021805
Ahern TP, Collin LJ, Baurley JW et al (2020) Metabolic pathway analysis and effectiveness of tamoxifen in danish breast cancer patients. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 29:582–590. https://doi.org/10.1158/1055-9965.EPI-19-0833
Karczewski KJ, Francioli LC, Tiao G et al (2020) The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581:434–443. https://doi.org/10.1038/s41586-020-2308-7
Schmidt M, Schmidt SAJ, Sandegaard JL et al (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/CLEP.S91125
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scand J Public Health 39:30–33. https://doi.org/10.1177/1403494811401482
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Amin MB, American Joint Committee on Cancer, American Cancer Society (2017) AJCC cancer staging manual, Eight edition / editor-in-chief, Mahul B. Amin, MD, FCAP ; editors, Stephen B. Edge, MD, FACS [and 16 others] ; Donna M. Gress, RHIT, CTR-Technical editor ; Laura R. Meyer, CAPM-Managing editor. American Joint Committee on Cancer, Springer, Chicago IL
Cronin-Fenton DP, Kjærsgaard A, Ahern TP et al (2017) Validity of Danish Breast Cancer Group (DBCG) registry data used in the predictors of breast cancer recurrence (ProBeCaRe) premenopausal breast cancer cohort study. Acta Oncol 56:1155–1160. https://doi.org/10.1080/0284186X.2017.1327720
de Graan A-JM, Lancaster CS, Obaidat A et al (2012) Influence of polymorphic OATP1B-type carriers on the disposition of docetaxel. Clin Cancer Res Off J Am Assoc Cancer Res 18:4433–4440. https://doi.org/10.1158/1078-0432.CCR-12-0761
Marcath LA, Kidwell KM, Robinson AC et al (2019) Patients carrying CYP2C8*3 have shorter systemic paclitaxel exposure. Pharmacogenomics 20:95–104. https://doi.org/10.2217/pgs-2018-0162
Busti AJ (2015) Genetic Polymorphisms of the CYP3A4 Enzyme and Potential Influence on Drug Efficacy and/or Safety. In: Evid.-Based Med. Consult. https://www.ebmconsult.com/articles/genetic-polymorphisms-cytochrome-p450-cyp3a4-enzyme. Accessed 2 July, 2021
Preissner SC, Hoffmann MF, Preissner R et al (2013) Polymorphic cytochrome P450 enzymes (CYPs) and their role in personalized therapy. PLoS ONE 8:e82562. https://doi.org/10.1371/journal.pone.0082562
Johnson N, Walker K, Gibson LJ et al (2012) CYP3A variation, premenopausal estrone levels, and breast cancer risk. J Natl Cancer Inst 104:657–669. https://doi.org/10.1093/jnci/djs156
Abdul Aziz AA, Md Salleh MS, Yahya MM et al (2021) Genetic association of CYP1B1 4326 C>G polymorphism with disease-free survival in TNBC patients undergoing TAC chemotherapy regimen. Asian Pac J Cancer Prev APJCP 22:1319–1324. https://doi.org/10.31557/APJCP.2021.22.4.1319
Tulsyan S, Chaturvedi P, Singh AK et al (2014) Assessment of clinical outcomes in breast cancer patients treated with taxanes: multi-analytical approach. Gene 543:69–75. https://doi.org/10.1016/j.gene.2014.04.004
Arai T, Miyoshi Y, Kim SJ et al (2008) Association of GSTP1 expression with resistance to docetaxel and paclitaxel in human breast cancers. Eur J Surg Oncol EJSO 34:734–738. https://doi.org/10.1016/j.ejso.2007.07.008
Marsh S, Somlo G, Li X et al (2007) Pharmacogenetic analysis of paclitaxel transport and metabolism genes in breast cancer. Pharmacogenomics J 7:362–365. https://doi.org/10.1038/sj.tpj.6500434
Mir O, Alexandre J, Tran A et al (2009) Relationship between GSTP1 Ile105Val polymorphism and docetaxel-induced peripheral neuropathy: clinical evidence of a role of oxidative stress in taxane toxicity. Ann Oncol 20:736–740. https://doi.org/10.1093/annonc/mdn698
Ma J, Zhu S-L, Liu Y et al (2017) GSTP1 polymorphism predicts treatment outcome and toxicities for breast cancer. Oncotarget 8:72939–72949. https://doi.org/10.18632/oncotarget.18513
Eckhoff L, Knoop A, Jensen MB, Ewertz M (2015) Persistence of docetaxel-induced neuropathy and impact on quality of life among breast cancer survivors. Eur J Cancer Oxf Engl 1990 51:292–300. https://doi.org/10.1016/j.ejca.2014.11.024
Jiang Q, Xu M, Liu Y et al (2018) Influence of the ABCB1 polymorphisms on the response to Taxane-containing chemotherapy: a systematic review and meta-analysis. Cancer Chemother Pharmacol 81:315–323. https://doi.org/10.1007/s00280-017-3496-1
Inada M, Sato M, Morita S et al (2010) Associations between oxaliplatin-induced peripheral neuropathy and polymorphisms of the ERCC1 and GSTP1 genes. Int J Clin Pharmacol Ther 48:729–734. https://doi.org/10.5414/cpp48729
Isla D, Sarries C, Rosell R et al (2004) Single nucleotide polymorphisms and outcome in docetaxel-cisplatin-treated advanced non-small-cell lung cancer. Ann Oncol Off J Eur Soc Med Oncol 15:1194–1203. https://doi.org/10.1093/annonc/mdh319
Schmidt M, Schmidt SAJ, Adelborg K et al (2019) The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol 11:563–591. https://doi.org/10.2147/CLEP.S179083
Ahern TP, Christensen M, Cronin-Fenton DP et al (2010) Concordance of metabolic enzyme genotypes assayed from paraffin-embedded, formalin-fixed breast tumors and normal lymphatic tissue. Clin Epidemiol 2:241–246. https://doi.org/10.2147/CLEP.S13811
Hertz DL, Kidwell KM, Thibert JN et al (2015) Genotyping concordance in DNA extracted from formalin-fixed paraffin embedded (FFPE) breast tumor and whole blood for pharmacogenetic analyses. Mol Oncol 9:1868–1876. https://doi.org/10.1016/j.molonc.2015.07.002
Goetz MP, Sun JX, Suman VJ et al (2014) Loss of heterozygosity at the CYP2D6 locus in breast cancer: implications for germline pharmacogenetic studies. J Natl Cancer Inst 107:dju401. https://doi.org/10.1093/jnci/dju401
Salanti G, Amountza G, Ntzani EE, Ioannidis JPA (2005) Hardy-Weinberg equilibrium in genetic association studies: an empirical evaluation of reporting, deviations, and power. Eur J Hum Genet EJHG 13:840–848. https://doi.org/10.1038/sj.ejhg.5201410
Minelli C, Thompson JR, Abrams KR et al (2008) How should we use information about HWE in the meta-analyses of genetic association studies? Int J Epidemiol 37:136–146. https://doi.org/10.1093/ije/dym234
Dong N, Yu J, Wang C et al (2012) Pharmacogenetic assessment of clinical outcome in patients with metastatic breast cancer treated with docetaxel plus capecitabine. J Cancer Res Clin Oncol 138:1197–1203. https://doi.org/10.1007/s00432-012-1183-5
Li W, Zhang D, Du F et al (2017) ABCB1 3435TT and ABCG2 421CC genotypes were significantly associated with longer progression-free survival in Chinese breast cancer patients. Oncotarget 8:111041–111052. https://doi.org/10.18632/oncotarget.22201
Song Q, Zhou X, Yu J et al (2015) The prognostic values of CYP2B6 genetic polymorphisms and metastatic sites for advanced breast cancer patients treated with docetaxel and thiotepa. Sci Rep 5:16775. https://doi.org/10.1038/srep16775
Wang J, Wang T, Yin G-Y et al (2015) Glutathione S-transferase polymorphisms influence chemotherapy response and treatment outcome in breast cancer. Genet Mol Res GMR 14:11126–11132. https://doi.org/10.4238/2015.September.22.6
Kim H-J, Im S-A, Keam B et al (2015) ABCB1 polymorphism as prognostic factor in breast cancer patients treated with docetaxel and doxorubicin neoadjuvant chemotherapy. Cancer Sci 106:86–93. https://doi.org/10.1111/cas.12560
Zhou X, Qiao G, Wang X et al (2018) CYP1A1 genetic polymorphism is a promising predictor to improve chemotherapy effects in patients with metastatic breast cancer treated with docetaxel plus thiotepa vs. docetaxel plus capecitabine. Cancer Chemother Pharmacol 81:365–372. https://doi.org/10.1007/s00280-017-3500-9
Baurley JW, Kjærsgaard A, Zwick ME et al (2020) Bayesian pathway analysis for complex interactions. Am J Epidemiol 189:1610–1622. https://doi.org/10.1093/aje/kwaa130
Funding
This project received funding from the Danish Cancer Society [R167-A11045-17-S2] to DCF, from Aarhus University to CFH, from the Danish Cancer Research Foundation [PLESNER-FAST-Active.FID1839672] to CFH, and from the Lundbeck Foundation [R167–2013–15861] to DCF. The ProBe CaRe cohort infrastructure was supported by grant R01CA166825 to TLL from the US National Cancer Institute.
Author information
Authors and Affiliations
Contributions
CFH contributed to conceptualization, methodology, formal analysis, investigation, writing of the original draft, visualization, funding acquisition, and project administration. PD contributed to conceptualization, resources, investigation, data curation, supervision, methodology, and writing, reviewing, and editing of the manuscript. TBS contributed to conceptualization, supervision, methodology, and writing, reviewing, and editing of the manuscript. SF contributed to resources, data curation, software, and writing, reviewing, and editing of the manuscript. SHD contributed to data curation, resources, investigation, and writing, reviewing, and editing of the manuscript. MK contributed to conceptualization and writing, reviewing, and editing of the manuscript. BE contributed to resources, supervision, and writing, reviewing, and editing of the manuscript. TLL contributed to conceptualization, supervision, investigation, funding acquisition, and writing, reviewing, and editing of the manuscript. TAP contributed to supervision, investigation, data curation, and writing, reviewing, and editing of the manuscript. HTS contributed to investigation, resources, and writing, reviewing, and editing of the manuscript. DCF contributed to conceptualization, supervision, data curation, methodology, investigation, writing of the original draft, writing, reviewing, and editing of the manuscript, funding acquisition, and project administration.
Corresponding author
Ethics declarations
Competing interest
TBS has received consultancy fees from Pfizer and teaching fees from Orifarm, Eisai, Novartis, and Astellas Pharma. TLL participates in the Amgen Methods Advisory Council, for which he receives consulting fees and travel support. The Department of Clinical Epidemiology, Aarhus University Hospital, receives funding for other studies from EMA and from companies in the form of research grants to (and administered by) Aarhus University. BE has received institutional grants from AstraZeneca, Eli Lilly, MSD, Novartis, Pfizer, Roche, and Samsung Bioepis. None of these disclosures have any relation to the present study.
Consent to participate and publish
The use of registry-based data for scientific studies in Denmark requires no consent from the participants.
Ethical approval
The Danish Data Protection Agency (AU 2016–051-000001, #808), the Regional Ethics Committee (Record no. 1–10-72–4-18), and the Danish Breast Cancer Group (DBCG) (DBCG-2018–01-04) approved the study.
Data availability
The data used for the current study derive from nationwide, population-based administrative and medical registries, linked anonymously using a personalized identifier. The data are available from Statistics Denmark, DBCG and the corresponding author. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the authors upon reasonable request with the permission of Statistics Denmark, DBCG, The Danish Health Authorities, The Danish Data Protection Agency, and The Central Jutland Region Committee on Health Research Ethics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hjorth, C.F., Damkier, P., Stage, T.B. et al. Single-nucleotide polymorphisms and the effectiveness of taxane-based chemotherapy in premenopausal breast cancer: a population-based cohort study in Denmark. Breast Cancer Res Treat 194, 353–363 (2022). https://doi.org/10.1007/s10549-022-06596-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06596-2