Abstract
Purpose
Results of the associations between weight change after breast cancer diagnosis and prognosis were inconsistent. The modification effects of menopausal status and endocrine therapy on the associations remain poorly understood.
Methods
A total of 2016 breast cancer patients were recruited between October 2008 and January 2018 and followed up until December 31, 2019 in Guangzhou. Multivariate Cox models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (95% CIs) for progression-free survival (PFS) in association with weight change after diagnosis.
Results
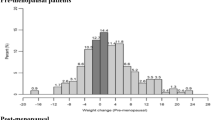
Weight loss at 2 years (HR = 1.34, 95% CI 0.87–2.06) or more than 2 years (HR = 1.95, 95% CI 1.22–3.10) after diagnosis increased risk of breast cancer progression. The adverse effect of weight loss was significantly more pronounced in post-menopausal than pre-menopausal women, particularly for weight loss at 2 years after diagnosis, with the HRs and 95% CIs of 2.41 (1.25–4.63) and 0.90 (0.49–1.64), respectively. Weight gain tended to reduce the risk of disease progression among patients with endocrine therapy but not for those with non-endocrine therapy; the significant interaction between weight gain at 2 years after diagnosis and endocrine therapy was observed (Pinteraction = 0.042).
Conclusion
Our finding suggested that weight loss was detrimental to breast cancer prognosis, particularly for post-menopausal women, while weight gain may be a potential beneficial indicator for the patients with endocrine therapy but not for those with non-endocrine therapy.
Similar content being viewed by others
Data availability
Enquiries about data availability should be directed to the authors.
Consent for publication
Not applicable.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hazard ratio
- PFS:
-
Progression-free survival
- PR:
-
Progesterone receptor
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132. https://doi.org/10.3322/caac.21338
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70:7–30. https://doi.org/10.3322/caac.21590
Chan D, Vieira AR, Aune D, Bandera EV, Greenwood DC, Mctiernan A, Navarro RD, Thune I, Vieira R, Norat T (2014) Body mass index and survival in women with breast cancer—systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol 25:1901–1914. https://doi.org/10.1093/annonc/mdu042
Colleoni M, Giobbie-Hurder A (2010) Benefits and adverse effects of endocrine therapy. Ann Oncol 21(Suppl 7):i107–i111. https://doi.org/10.1093/annonc/mdq281
De Ruysscher D, Niedermann G, Burnet NG, Siva S, Lee A, Hegi-Johnson F (2019) Radiotherapy toxicity. Nat Rev Dis Primers 5:13. https://doi.org/10.1038/s41572-019-0064-5
Nurgali K, Jagoe RT, Abalo R (2018) Editorial: adverse effects of cancer chemotherapy: anything new to improve tolerance and reduce sequelae? Front Pharmacol 9:245. https://doi.org/10.3389/fphar.2018.00245
Bradshaw PT, Ibrahim JG, Stevens J, Cleveland R, Abrahamson PE, Satia JA, Teitelbaum SL, Neugut AI, Gammon MD (2012) Postdiagnosis change in bodyweight and survival after breast cancer diagnosis. Epidemiology 23:320–327. https://doi.org/10.1097/EDE.0b013e31824596a1
Nichols HB, Trentham-Dietz A, Egan KM, Titus-Ernstoff L, Holmes MD, Bersch AJ, Holick CN, Hampton JM, Stampfer MJ, Willett WC et al (2009) Body mass index before and after breast cancer diagnosis: associations with all-cause, breast cancer, and cardiovascular disease mortality. Cancer Epidemiol Biomark Prev 18:1403–1409. https://doi.org/10.1158/1055-9965.EPI-08-1094
Jung AY, Hüsing A, Behrens S, Krzykalla J, Obi N, Becher H, Chang-Claude J (2021) Postdiagnosis weight change is associated with poorer survival in breast cancer survivors: a prospective population-based patient cohort study. Int J Cancer 148:18–27. https://doi.org/10.1002/ijc.33181
Chen X, Lu W, Zheng W, Gu K, Chen Z, Zheng Y, Shu XO (2010) Obesity and weight change in relation to breast cancer survival. Breast Cancer Res Treat 122:823–833. https://doi.org/10.1007/s10549-009-0708-3
Cespedes Feliciano EM, Kroenke CH, Bradshaw PT, Chen WY, Prado CM, Weltzien EK, Castillo AL, Caan BJ (2017) Postdiagnosis weight change and survival following a diagnosis of early-stage breast cancer. Cancer Epidemiol Biomark Prev 26:44–50. https://doi.org/10.1158/1055-9965.EPI-16-0150
Caan BJ, Kwan ML, Shu XO, Pierce JP, Patterson RE, Nechuta SJ, Poole EM, Kroenke CH, Weltzien EK, Flatt SW et al (2012) Weight change and survival after breast cancer in the after breast cancer pooling project. Cancer Epidemiol Biomark Prev 21:1260–1271. https://doi.org/10.1158/1055-9965.EPI-12-0306
Caan BJ, Kwan ML, Hartzell G, Castillo A, Slattery ML, Sternfeld B, Weltzien E (2008) Pre-diagnosis body mass index, post-diagnosis weight change, and prognosis among women with early stage breast cancer. Cancer Causes Control 19:1319–1328. https://doi.org/10.1007/s10552-008-9203-0
Goodwin PJ, Segal RJ, Vallis M, Ligibel JA, Pond GR, Robidoux A, Findlay B, Gralow JR, Mukherjee SD, Levine M et al (2020) The LISA randomized trial of a weight loss intervention in postmenopausal breast cancer. NPJ Breast Cancer 6:6. https://doi.org/10.1038/s41523-020-0149-z
Sedjo RL, Flatt SW, Byers T, Colditz GA, Demark-Wahnefried W, Ganz PA, Wolin KY, Elias A, Krontiras H, Liu J et al (2016) Impact of a behavioral weight loss intervention on comorbidities in overweight and obese breast cancer survivors. Support Care Cancer 24:3285–3293. https://doi.org/10.1007/s00520-016-3141-2
Caan BJ, Emond JA, Natarajan L, Castillo A, Gunderson EP, Habel L, Jones L, Newman VA, Rock CL, Slattery ML et al (2006) Post-diagnosis weight gain and breast cancer recurrence in women with early stage breast cancer. Breast Cancer Res Treat 99:47–57. https://doi.org/10.1007/s10549-006-9179-y
Kroenke CH, Chen WY, Rosner B, Holmes MD (2005) Weight, weight gain, and survival after breast cancer diagnosis. J Clin Oncol 23:1370–1378. https://doi.org/10.1200/JCO.2005.01.079
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D, Million WSC (2007) Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ 335:1134–1139. https://doi.org/10.1136/bmj.39367.495995.AE
James FR, Wootton S, Jackson A, Wiseman M, Copson ER, Cutress RI (2015) Obesity in breast cancer—what is the risk factor? Eur J Cancer 51:705–720. https://doi.org/10.1016/j.ejca.2015.01.057
Dowsett M, Folkerd E (2015) Reduced progesterone levels explain the reduced risk of breast cancer in obese premenopausal women: a new hypothesis. Breast Cancer Res Treat 149:1–4. https://doi.org/10.1007/s10549-014-3211-4
Perez EA (2007) Safety profiles of tamoxifen and the aromatase inhibitors in adjuvant therapy of hormone-responsive early breast cancer. Ann Oncol 18(Suppl 8):i26–i35. https://doi.org/10.1093/annonc/mdm263
Cleary MP, Grossmann ME (2009) Minireview: obesity and breast cancer: the estrogen connection. Endocrinology 150:2537–2542. https://doi.org/10.1210/en.2009-0070
Liao Y, Ren J, Zhang W, Zhang Z, Lin Y, Su F, Jia W, Tang L, Ren Z (2017) Polymorphisms in homologous recombination repair genes and the risk and survival of breast cancer. J Gene Med 19:e2988. https://doi.org/10.1002/jgm.2988
He JR, Tang LY, Yu DD, Su FX, Song EW, Lin Y, Wang SM, Lai GC, Chen WQ, Ren ZF (2011) Epstein–Barr virus and breast cancer: serological study in a high-incidence area of nasopharyngeal carcinoma. Cancer Lett 309:128–136. https://doi.org/10.1016/j.canlet.2011.05.012
Schvartsman G, Gutierrez-Barrera AM, Song J, Ueno NT, Peterson SK, Arun B (2017) Association between weight gain during adjuvant chemotherapy for early-stage breast cancer and survival outcomes. Cancer Med 6:2515–2522. https://doi.org/10.1002/cam4.1207
Michaud M, Balardy L, Moulis G, Gaudin C, Peyrot C, Vellas B, Cesari M, Nourhashemi F (2013) Proinflammatory cytokines, aging, and age-related diseases. J Am Med Dir Assoc 14:877–882. https://doi.org/10.1016/j.jamda.2013.05.009
Qureshi R, Picon-Ruiz M, Aurrekoetxea-Rodriguez I, Nunes De Paiva V, D’Amico M, Yoon H, Radhakrishnan R, Morata-Tarifa C, Ince T, Lippman ME et al (2020) The major pre- and postmenopausal estrogens play opposing roles in obesity-driven mammary inflammation and breast cancer development. Cell Metab 31:1154–1172. https://doi.org/10.1016/j.cmet.2020.05.008
Mantovani A, Marchesi F, Porta C, Sica A, Allavena P (2007) Inflammation and cancer: breast cancer as a prototype. Breast 16(Suppl 2):S27–S33. https://doi.org/10.1016/j.breast.2007.07.013
Morley JE, Thomas DR, Wilson MM (2006) Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr 83:735–743. https://doi.org/10.1093/ajcn/83.4.735
van Londen GJ, Perera S, Vujevich K, Rastogi P, Lembersky B, Brufsky A, Vogel V, Greenspan SL (2011) The impact of an aromatase inhibitor on body composition and gonadal hormone levels in women with breast cancer. Breast Cancer Res Treat 125:441–446. https://doi.org/10.1007/s10549-010-1223-2
Francini G, Petrioli R, Montagnani A, Cadirni A, Campagna S, Francini E, Gonnelli S (2006) Exemestane after tamoxifen as adjuvant hormonal therapy in postmenopausal women with breast cancer: effects on body composition and lipids. Br J Cancer 95:153–158. https://doi.org/10.1038/sj.bjc.6603258
Iwase T, Wang X, Shrimanker TV, Kolonin MG, Ueno NT (2021) Body composition and breast cancer risk and treatment: mechanisms and impact. Breast Cancer Res Treat 186:273–283. https://doi.org/10.1007/s10549-020-06092-5
Caan BJ, Cespedes Feliciano EM, Kroenke CH (2018) The importance of body composition in explaining the overweight paradox in cancer—counterpoint. Cancer Res 78:1906–1912. https://doi.org/10.1158/0008-5472.CAN-17-3287
Cespedes Feliciano EM, Kroenke CH, Caan BJ (2018) The obesity paradox in cancer: how important is muscle? Annu Rev Nutr 38:357–379. https://doi.org/10.1146/annurev-nutr-082117-051723
Li X, Yang J, Peng L, Sahin AA, Huo L, Ward KC, O’Regan R, Torres MA, Meisel JL (2017) Triple-negative breast cancer has worse overall survival and cause-specific survival than non-triple-negative breast cancer. Breast Cancer Res Treat 161:279–287. https://doi.org/10.1007/s10549-016-4059-6
Nyrop KA, Deal AM, Lee JT, Muss HB, Choi SK, Dixon S, Wheless A, Carey LA, Shachar SS (2017) Weight changes in postmenopausal breast cancer survivors over 2 years of endocrine therapy: a retrospective chart review. Breast Cancer Res Treat 162:375–388. https://doi.org/10.1007/s10549-017-4106-y
Chinese Anti-Cancer Association Committee of Breast Cancer Society (2011) Chinese Anti-Cancer Association (CSCA) diagnosis and treatment guidelines for breast cancer (version 2011). China Oncol 19:448–474. https://doi.org/10.3969/j.issn.1007-3639.2009.06.012
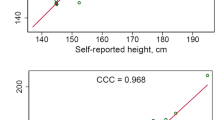
Spencer EA, Appleby PN, Davey GK, Key TJ (2002) Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr 5:561–565. https://doi.org/10.1079/PHN2001322
Qin B, Llanos A, Lin Y, Szamreta EA, Plascak JJ, Oh H, Pawlish K, Ambrosone CB, Demissie K, Hong CC et al (2018) Validity of self-reported weight, height, and body mass index among African American breast cancer survivors. J Cancer Surviv 12:460–468. https://doi.org/10.1007/s11764-018-0685-9
Acknowledgements
We sincerely thank the patients who participated in this study, the staff who conducted the baseline and the follow-up data collection, and the medical staff in the breast departments of the First Affiliated Hospital, the Second Affiliated Hospital, and the Cancer Center of Sun Yat-Sen University.
Funding
The results reported herein correspond to specific aims of Grants (or other source of support) 81773515 and 81973115 from the National Natural Science Foundation of China, and 2019B030316002 from the Science and Technology Planning Project of Guangdong Province, China.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The study was approved by the Ethics Committee of School of Public Health, Sun Yat-sen University.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, YX., Liang, ZZ., Li, Yq. et al. Association between weight change and breast cancer prognosis. Breast Cancer Res Treat 193, 677–684 (2022). https://doi.org/10.1007/s10549-022-06592-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06592-6