Abstract
Purpose
Breast-contour preservation (BCP) is possible for most women treated for early-stage breast cancer. BCP can be defined as primary breast-conserving treatment (BCT), neoadjuvant chemotherapy (NAC) followed by BCT and immediate postmastectomy breast reconstruction (IBR). This study provides insight in current BCP strategies in Denmark and the Netherlands and aims to identify opportunities for improvement within both countries.
Methods
A total of 92,881 patients with early-stage breast cancer who were operated in Denmark and the Netherlands between 2012 and 2017 were selected from the Danish Breast Cancer Group and the Dutch National Breast Cancer Audit databases. BCP procedures and predictive factors were analyzed within and between both countries.
Results
BCP was achieved in 76.7% (n = 16,355) of the Danish and in 74.5% (n = 53,328) of the Dutch patients. While BCP rate did not change significantly over time in Denmark (p = 0.250), a significant increase in BCP rate from 69.5% in 2012 to 78.5% in 2017 (p < 0.001) was observed in the Netherlands. In both countries, variation in BCP rates between hospitals decreased over time. NAC followed by BCT and postmastectomy IBR was substantially more often used in the Netherlands compared to Denmark, specifically in patients younger than 50 years.
Conclusions
In more than 75% of all Danish and Dutch patients, surgically treated for early-stage breast cancer, the breast-contour was preserved. The different use of BCP strategies within Denmark and the Netherlands and the differences observed between hospitals in both countries emphasize the need for more (inter)national consensus on treatment modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since several landmark studies in the 1980s confirmed comparable survival outcomes for early-stage breast cancer after breast-conserving treatment (BCT) and mastectomy [1,2,3], BCT has become the preferred standard of care. BCT is defined as breast-conserving surgery (BCS) followed by radiation therapy. Besides the surgical shift towards BCS, attention for outcomes such as the patients’ quality of life has increased in the last decade.
Loss of the breast mound may lead to a decreased self-image and quality of life [4]. Nowadays, preservation of the breast mound is possible for most early-stage breast cancer patients. This has been achieved by primary BCS for smaller tumors, and by the introduction of oncoplastic surgery techniques for large tumors [5]. Furthermore, neoadjuvant chemotherapy (NAC) is increasingly being used to downsize the tumor allowing for BCT [6]. In addition to this, immediate breast reconstruction (IBR) leads to restoration of the breast mound if mastectomy is indicated. Furthermore, IBR compared to delayed breast reconstruction reduces additional operations and hospitalizations [7], leading to reduced patient burden and healthcare costs [8].
National registries have demonstrated that overall, the proportion of breast cancer patients undergoing BCT (either primary or after NAC) or mastectomy followed by IBR, is currently over 70% in the USA and some European countries [9,10,11,12,13]. It is also known that there is a large variation between hospitals in the use of different treatment modalities [14, 15].
A previous study reported on breast-contour preservation (BCP) as a new comprehensive parameter for evaluating breast cancer treatment on a national level [16]. This new parameter aims to reflect the combined efforts of nonsurgical and surgical treatments to achieve preservation of the breast mound and is defined as either primary BCS, BCS after NAC or mastectomy followed by IBR. Because not all patients are primarily eligible for BCS, increasing the rate of BCP using either NAC or mastectomy followed by IBR is therefore of major importance. Despite that European, Danish and Dutch guidelines empathize the importance of BCP by highlighting the separate treatment strategies leading to BCP [17,18,19], previous literature focusing on all different strategies is sparse and nonexisting when comparing countries within Europe.
An international evaluation of BCP rates could provide valuable insight into daily practice and could identify possibilities to improve BCP strategies. The Netherlands and Denmark are both high-income countries and have well-maintained population-based breast cancer registries with similar medical care systems that provide equal access to healthcare for all patients, making them suitable for evaluation. The aims of the current study were to investigate the prevalence of BCP among women with early-stage breast cancer in Denmark and the Netherlands and to identify opportunities for improvement. This information can be used to increase the use of BCP procedures and reduce variation between hospitals in BCP rate in patients with early-stage breast cancer.
Methods
Data sources
Anonymized patient data regarding the demographic, clinicopathological, and treatment characteristics was obtained from the Danish Breast Cancer Group (DBCG) and the National Breast Cancer Organization Netherlands (NABON) Breast Cancer Audit (NBCA) from Denmark and the Netherlands, respectively. The scientific committee of the NBCA and the DBCG Board, and the Danish Clinical Quality Program– National Clinical Registries (RKKP) approved this study.
The DBCG was established in 1977 and prospectively collects data on patient-, tumor, and treatment-related characteristics, and follow-up of all female patients diagnosed with primary breast cancer in Denmark [20]. The NBCA was established in 2011 and prospectively collects data on patient-, tumor-, and treatment-related characteristics of all surgically treated patients diagnosed with primary invasive breast cancer or ductal carcinoma in situ (DCIS) in the Netherlands [9]. A more detailed description of the organization and data collection of both the DBCG and NBCA was published previously [9, 21].
Study population
All female patients with primary invasive early-stage breast cancer who were operated between January 1st, 2012 and December 31st, 2017 and were registered in the DBCG or NBCA database were selected for this study. Early-stage breast cancer was defined as T1-2 N0-1 without distant metastasis. Patients diagnosed with locally advanced breast cancer were excluded. Patients diagnosed with only DCIS were not included as these patients are not registered in the database for the clinical quality program in Denmark, and therefore completeness of data is uncertain.
Definitions and outcomes
In both countries, rarely reported histological subtypes such as mucinous, medullary, papillary, and tubular subtype were categorized as ‘other.' In Denmark, differentiation grade was determined for ductal and lobular breast cancer, but not for other subtypes according to the modified version of the Bloom-Richardson scoring system by Ellis et al. [22]. In the Netherlands, differentiation grade was categorized for all histological subtypes according to the modified version by Lakhani et al. [23]. In both registers, tumor size and lymph node status was categorized according to the 7th edition of the American Joint Committee on Cancer’s Cancer Staging Manuel [24]. For the current study, breast cancer specimens with ≥ 10% positively stained cells for estrogen receptor (ER) by immunohistochemistry were considered positive. Progesterone status is not registered in the DBCG database for the clinical quality program in Denmark and could therefore not be included in the current study. Human epidermal growth factor receptor 2 (HER2) expression was tested using an immunohistochemistry test or gene amplification in a fluorescence in situ hybridization test according to standard criteria [25].
Surgical treatment was categorized as BCS or mastectomy at definitive treatment. The primary outcome of this study was preservation of the breast contour. A definition of BCP was met if the patient underwent one of the following treatments: (1) primary BCS, (2) NAC followed by BCS, or (3) mastectomy (either primary or after NAC) followed by IBR. IBR was defined as breast reconstruction at the same procedure as mastectomy. Patients were categorized as not having received BCP if they had undergone mastectomy without IBR. While in the DBCG database, surgical procedures up to 1 month following primary surgery are included, no time limit exists for inclusion of secondary procedures in the NBCA database for the primary breast tumor.
Hospital surgical volume was defined as the average number of included patients operated per hospital per year and was categorized in low (< 150 patients), intermediate (150–299 patients), and high (≥ 300 patients) volume hospital. The average number of patients was for hospitals that were not active the whole period, only accounted for the years the hospitals actually treated patients.
Statistical analysis
Analyses were stratified into two patient populations: (1) patients registered in the DBCG database and (2) patients registered in the NBCA database. Missing characteristics were categorized as a separate characteristic. Patient-, tumor-, and hospital-related characteristics were compared between patients who underwent mastectomy alone and those who underwent a BCP procedure, using χ2-tests for categorical variables. Patients with unknown characteristics were included in the descriptive statistics. Descriptive statistics were used to report on the overall BCP rate in both populations. To describe the BCP rate between hospitals and over time, hospital mean and 95% control limits (CLs) are presented in three funnel plots for year of operation 2013, 2015, and 2017 [26, 27]. Univariable and multivariable logistic regression analyses were used to estimate the odds ratio (OR) with 95% confidence intervals (CIs) for BCP, applying the Wald test for statistics significance. Patients with unknown characteristics were not included in univariable and multivariable analyses. All tests were two-sided and a p value of < 0.05 was considered statistically significant. Analyses were performed using SPSS ® (version 24, IBM, Armonk, New York, USA).
Data availability
Data can be made available upon reasonable request to the NBCA and the DBCG Board, and the Danish Clinical Registries.
Results
In total, 92,881 patients met the inclusion criteria, of whom 21,288 (22.9%) had been registered in Denmark and 71,593 (77.1%) in the Netherlands. The mean age (standard deviation) at diagnosis was 61.7 (12.5) years for patients in Denmark and 61.1 (12.3) years for patients in the Netherlands. In both countries, most of the patients were diagnosed with stage T1 (≤ 20 mm) breast cancer without lymph node involvement and with a ductal subtype which was estrogen positive and HER2 negative (Table 1).
In Denmark (n = 12 hospitals), there were 1 low-volume, 7 intermediate-volume, and 4 high-volume hospitals, whereas in the Netherlands (n = 82 hospitals), there were 50 low-volume, 28 intermediate-volume and 4 high-volume hospitals.
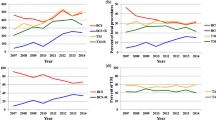
Between 2012 and 2017, 16,355 (76.7%) patients from Denmark and 53,328 (74.5%) patients from the Netherlands underwent BCP (Fig. 1). While the overall BCP rate was stable over time in Denmark (75.8% to 76.8%, p = 0.250), BCP rate increased significantly from 69.5% in 2012 to 78.5% in 2017 in the Netherlands (p < 0.001).
The BCP strategies changed significantly over time within both countries (p < 0.001). While the primary BCS rate decreased from 72.4% in 2012 to 68.7% in 2017 in Denmark, primary BCS rate only slightly decreased from 59.9 to 59.6% in the Netherlands (Fig. 1). The NAC followed by BCS rate increased from 1.3 to 5.7% in Denmark between 2012 and 2017 and from 3.1 to 9.6% in the Netherlands. The mastectomy followed by IBR rate slightly increased from 2.0% in 2012 to 2.4% in 2017 in Denmark and increased from 6.5 to 9.2% in the Netherlands (Fig. 1). The average mastectomy followed by IBR rate was different between both countries in both the lymph node positive patient group (1.5% in Denmark vs 9.3% in the Netherlands,) as in the lymph node negative patient group (2.4% vs 8.5%, respectively). In both countries, the majority of IBRs were implant- or tissue expander (TE)-based reconstructions (94.0 vs. 89.4%).
Baseline characteristics associated with BCP within both countries are listed in Table 2. While the year of diagnosis was not associated with BCP in Denmark, patients operated in more recent years compared to year 2012 were more likely to undergo a BCP procedure in the Netherlands, with increasing ORs (Table 2).
The overall BCP rate was significantly different between age groups (Table 1). After adjusting for confounders, in both countries, patients between 50 and 59 years old were more likely to undergo BCP compared to patients of 60 to 69 years of age (OR 1.13, 95% CIs 1.02–1.26 and OR 1.31, 95% CIs 1.25–1.39, respectively). In the Netherlands, patients younger than 40 years and between 40 to 49 years of age were also more likely to undergo BCP compared to those who were 60 to 69 years old (OR 1.20, 95% CIs 1.08–1.34 and OR 1.20, 95% CIs 1.12–1.28, respectively). Whereas, in Denmark, patients younger than 40 years and between 40 and 49 years of age (OR 0.64, 95% CIs 0.53–0.77 and OR 0.84, 95% CIs 0.74–0.94, respectively) were less likely to undergo BCP compared to those who were 60 to 69 years old (Table 2).
Among other predictive characteristics, patients diagnosed with a T2 tumor (OR 0.28, 95% CIs 0.26–0.30 and OR 0.40, 95% CIs 0.38–0.41, respectively) compared to T1 tumor and lymph node involvement (OR 0.51, 95% CIs 0.48–0.55 and OR 0.53, 95% CIs 0.51–0.56, respectively) were less likely to undergo BCP within both Denmark and the Netherlands.
In both Denmark and the Netherlands, NAC followed by BCS (6.1% and 18.2%, respectively) and mastectomy followed by IBR (10.1% and 32.9%, respectively) was most commonly performed in patients younger than 40 years (Fig. 2). Both treatment modalities were less commonly performed as age increased and were almost never performed in patients older than 80 years (Fig. 2).
Although in general the variation in BCP rates between hospitals was smaller in Denmark compared to the Netherlands, a decrease in variation in BCP rates was observed between hospitals within both Denmark and the Netherlands over time (Fig. 3).
In both countries, patients were more likely to undergo BCP if they underwent surgery at a high-volume hospital (OR 1.55, 95% CIs 1.44–1.67 and OR 1.09, 95% CIs 1.02–1.17, respectively) compared to an intermediate-volume hospital. In the Netherlands, patients treated at a low-volume hospital were less likely to preserve their breast contour compared to patients in an intermediate-volume hospital (OR 0.66, 95% CIs 0.64–0.69).
Discussion
In this large population-based study of patients with early-stage breast cancer, insight into BCP strategies is provided and it is shown that BCP was achieved in more than 75% of patients in both Denmark and the Netherlands, albeit using different treatment strategies. While in Denmark BCP was predominantly achieved by using primary BCS, the use of NAC followed by BCS and mastectomy followed by IBR played a substantial role in the Netherlands, specifically in patients younger than 50 years. We observed a stable high overall BCP rate between 2012 and 2017 in Denmark and a significant increase over time in the Netherlands. Current findings demonstrated considerable variation in the use of BCP strategies between hospitals within both countries and between countries. These results therefore suggest that more (inter)national consensus on the indication for different breast cancer treatment modalities is warranted, specifically on indications for NAC and mastectomy followed by IBR.
Van Bommel et al. first described BCP as a new comprehensive parameter for evaluating quality of breast cancer treatment in patients with early-stage as well as more advanced stages of breast cancer [16]. They reported an increase in the overall BCP rate from 63% in 2011 to 71% in 2015 which was translated as a quality of care improvement [16]. This observed trend continued in the Netherlands up to 2017 as is shown in the current study, although the different strategies used in Denmark made an interesting perspective.
The current study observed differences in BCP strategies per age group and over time between Denmark and the Netherlands. The rate of patients undergoing NAC followed by BCS more than tripled in both countries over time. However, in Denmark, less patients younger than 50 years, underwent NAC followed by BCS (6.3 vs. 16.7%, respectively) or mastectomy followed by IBR (6.7 vs. 22.2%, respectively) compared to the Netherlands. In reviewing literature, several studies from around the world have reported an increasing use of NAC, specifically in patients younger than 70 years and in patients with more advanced tumors [6, 28, 29]. The difference in use of NAC followed by BCS between both countries may partly be explained by the moment of introducing NAC in the national guidelines. While in the Netherlands NAC was introduced as a downstaging procedure in the breast cancer guideline in 2012 [14, 30], Danish guidelines incorporated NAC as a downstaging procedure in the second half of 2016 and has been increasingly used thereafter [19].
Breast cancer with lymph node involvement requires radiotherapy, which limits the use of IBR as radiotherapy is frequently mentioned as a contraindication for implant-based IBR [31, 32]. Interestingly, different IBR rates among patients who underwent mastectomy were found between both countries, both in patients with a positive and negative lymph node. It is unlikely that the type of IBR technique explains the observed differences, since the majority of IBRs were implant- or TE based in both countries. This together with the relative low increase in IBR rates in Denmark suggests potential room for improvement in Denmark. Internationally, there has been an increasing use of IBR in most high-income countries in the last decade. The mean IBR rate of 25.5% among patients who underwent mastectomy in the Netherlands is within the range of other high-income countries, such as United Kingdom (up to 23% in 2016) [33], USA (up to 43% in 2014) [34], and Australia (up to 18% in 2013) [35]. Nonetheless, previous research has shown substantial variation in postmastectomy IBR rates between hospitals in the Netherlands and other countries, unexplained by patient and tumor characteristics [15, 36, 37]. The different use of IBR between hospitals emphasizes the need for more international consensus on the indications for IBR. Future cross-country studies could focus on hospital organizational factors as some of these are associated with the use of IBR [38, 39]. Unfortunately, these factors could not be accounted for in the current study.
Overall, a smaller proportion of patients underwent a mastectomy (with or without IBR) in Denmark compared to the Netherlands (25.5% vs. 34.2%, respectively). This finding suggest room for improvement in the Netherlands in performing more BCS instead of mastectomy, since previous studies showed comparable survival outcomes when comparing patients who underwent BCT and mastectomy [2, 40].
Different grading systems were used in both countries. Hereby, relatively more Dutch patients with an unknown differentiation grade were excluded from the logistic regression model compared to Danish patients. Nonetheless, the impact is most likely limited as subsequent analysis showed the same findings when including these patients (data not shown).
The current study highlights an interesting difference in hospital volume. While in Denmark only 3.3% of patients were operated at a low-volume hospital, this was 40% in the Netherlands. Despite that previous studies found minimal differences in survival between intermediate- and high-volume hospitals [41, 42], no literature exists on the relationship between hospital volume and ‘soft’ outcomes such as BCP. In the current study, a significant association between hospital volume and BCP rate was found. Although it is beyond the scope of the current study, current findings suggest that BCP might be increased in the Netherlands by centralizing breast cancer care. This hypothesis requires additional future analyses on the relationship between hospital volume and BCP.
A decrease of variation in BCP rates between hospitals was observed over time, specifically in the Netherlands. A potential contributor to this trend in the Netherlands might be the continuous feedback hospitals received on their BCP rate provided by the NBCA. Several other improvements in health care have been accomplished by monitoring the quality of cancer care and providing benchmark feedback to hospitals [43, 44].
The current study has several limitations. First, there might have been unaccounted confounders in the current analyses (e.g., comorbidities, social-economic status, smoking status). Unfortunately, these confounders are not registered in both databases. Second, there might be subtle differences in interpretation of definitions between those who register patients which might explain part of the treatment choices. Thirdly, only surgical procedures performed within 1 month after primary surgery were included in the DBCG database. Although most secondary surgery is performed within a short time period after primary surgery, secondary mastectomies or reconstructive efforts without oncologic purpose do occur after a longer time period, specifically in patients younger than 50 years with for instance a genetic predisposition. A previous study using the DBCG database reported a higher mastectomy rate after BCS in Denmark between 2008 and 2012 (data not shown) when including procedures up to 3 months after primary surgery [45]. Consensus regarding the inclusion period among national registries could improve future cross-country comparison. Lastly, the current study could unfortunately not account for whether patients in different hospitals had access to high skilled physicians who offered the entire field of breast reconstruction procedures. Strengths of the current study are the real-world population-based databases and high number of patients. To the best of the authors’ knowledge, there have been no previous cross-country population-based analyses, evaluating the comprehensive breast cancer treatment for early-stage breast cancer. Therefore, current findings can be used for comparison and benchmarking in future studies.
Abbreviations
- BCP:
-
Breast-contour preservation
- BCT:
-
Breast-conserving treatment
- NAC:
-
Neoadjuvant chemotherapy
- IBR:
-
Immediate postmastectomy breast reconstruction
- DBCG:
-
Danish Breast Cancer Cooperative Group
- NABON:
-
National Breast Cancer Organization Netherlands
- NBCA:
-
NABON Breast Cancer Audit
- DCIS:
-
Ductal carcinoma in situ
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- OR:
-
Odds ratio
- CIs:
-
Confidence intervals
References
Veronesi U, Saccozzi R, Del Vecchio M, Banfi A, Clemente C, De Lena M, Gallus G, Greco M, Luini A, Marubini E et al (1981) Comparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breast. N Engl J Med 305(1):6–11
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E (2002) Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347(16):1227–1232
Fisher B, Bauer M, Margolese R, Poisson R, Pilch Y, Redmond C, Fisher E, Wolmark N, Deutsch M, Montague E (1985) Five-year results of a randomized clinical trial comparing total mastectomy and segmental mastectomy with or without radiation in the treatment of breast cancer. N Engl J Med 312(11):665–673
Ng SK, Hare RM, Kuang RJ, Smith KM, Brown BJ, Hunter-Smith DJ (2016) Breast reconstruction post mastectomy: patient satisfaction and decision making. Ann Plast Surg 76(6):640–644
Clough KB, Benyahi D, Nos C, Charles C, Sarfati I (2015) Oncoplastic surgery: pushing the limits of breast-conserving surgery. Breast J 21(2):140–146
Spronk PER, Volders JH, van den Tol P, Smorenburg CH, Vrancken Peeters MTFD (2019) Breast conserving therapy after neoadjuvant chemotherapy; data from the Dutch Breast Cancer Audit. Eur J Surg Oncol 45(2):110–117
Jagsi R, Li Y, Morrow M, Janz N, Alderman A, Graff J, Hamilton A, Katz S, Hawley S (2015) Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg 261(6):1198–1206
Teo I, Reece GP, Christie IC, Guindani M, Markey MK, Heinberg LJ, Crosby MA, Fingeret MC (2016) Body image and quality of life of breast cancer patients: influence of timing and stage of breast reconstruction. Psychooncology 25(9):1106–1112
van Bommel AC, Spronk PE, Vrancken Peeters MT, Jager A, Lobbes M, Maduro JH, Mureau MA, Schreuder K, Smorenburg CH, Verloop J et al (2016) Clinical auditing as an instrument for quality improvement in breast cancer care in the Netherlands: The national NABON Breast Cancer Audit. J Surg Oncol
Liederbach E, Sisco M, Wang C, Pesce C, Sharpe S, Winchester DJ, Yao K (2015) Wait times for breast surgical operations, 2003–2011: a report from the National Cancer Data Base. Ann Surg Oncol 22(3):899–907
Hofvind S, Schlichting E, Ursin G, Sebuødegård S, Kåresen R (2013) Breast cancer surgery in Norway 1986–2009. Tidsskr Nor Laegeforen 133(15):1582–1586
Garcia-Etienne CA, Tomatis M, Heil J, Friedrichs K, Kreienberg R, Denk A, Kiechle M, Lorenz-Salehi F, Kimmig R, Emons G et al (2012) Mastectomy trends for early-stage breast cancer: a report from the EUSOMA multi-institutional European database. Eur J Cancer 48(13):1947–1956
Kvalitetsindikatorrapport for Brystkræft. https://dbcg.dk/PDF%2520Filer/aarsrapport_2017_final.pdf
Spronk PER, van Bommel ACM, Siesling S, Wouters MWJM, Vrancken Peeters MTFD, Smorenburg CH (2017) Variation in use of neoadjuvant chemotherapy in patients with stage III breast cancer: results of the Dutch national Breast Cancer Audit. Breast 36:34–38
van Bommel AC, Mureau MA, Schreuder K, van Dalen T, Vrancken Peeters MT, Schrieks M, Maduro JH, Siesling S (2017) Large variation between hospitals in immediate breast reconstruction rates after mastectomy for breast cancer in the Netherlands. J Plast Reconstr Aesthet Surg 70(2):215–221
van Bommel A, Spronk P, Mureau M, Siesling S, Smorenburg C, Tollenaar R, Vrancken Peeters MJ, van Dalen T (2019) Breast-contour-preserving procedure as a multidisciplinary parameter of esthetic outcome in breast cancer treatment in The Netherlands. Ann Surg Oncol. https://doi.org/10.1245/s10434-019-07265-3
Biganzoli L, Marotti L, Hart CD, Cataliotti L, Cutuli B, Kühn T, Mansel RE, Ponti A, Poortmans P, Regitnig P et al (2017) Quality indicators in breast cancer care: an update from the EUSOMA working group. Eur J Cancer 86:59–81
Dutch National Breast Cancer Guideline. https://www.oncoline.nl/borstkanker
DBCG. Retningslinier / Vejledninger. https://dbcg.dk/PDF%2520Filer/Kap7_Neoadj_KT_ved_brystkraeft_mhp_down-sizing_og_down-staging_04.10.2016.pdf
Christiansen P, Ejlertsen B, Jensen MB, Mouridsen H (2016) Danish Breast Cancer Cooperative Group. Clin Epidemiol 8:445–449
Jensen MB, Laenkholm AV, Offersen BV, Christiansen P, Kroman N, Mouridsen HT, Ejlertsen B (2018) The clinical database and implementation of treatment guidelines by the Danish Breast Cancer Cooperative Group in 2007–2016. Acta Oncol 57(1):13–18
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19(5):403–410
Lakhani SR, Cancer IAfRo, Organization WH (2012) WHO classification of tumours of the breast/edited by Sunil R. Lakhani.. [et al.]. International Agency for Research on Cancer, Lyon
Stephen Edge DRB, Compton CC, Fritz AG, Greene F, Trotti A (2010) AJCC cancer staging handbook, 7th edn. Springer, New York
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31(31):3997–4013
Manktelow BN, Seaton SE, Evans TA (2016) Funnel plot control limits to identify poorly performing healthcare providers when there is uncertainty in the value of the benchmark. Stat Methods Med Res 25(6):2670–2684
Seaton SE, Manktelow BN (2012) The probability of being identified as an outlier with commonly used funnel plot control limits for the standardised mortality ratio. BMC Med Res Methodol 12:98
Mougalian SS, Soulos PR, Killelea BK, Lannin DR, Abu-Khalaf MM, DiGiovanna MP, Sanft TB, Pusztai L, Gross CP, Chagpar AB (2015) Use of neoadjuvant chemotherapy for patients with stage I to III breast cancer in the United States. Cancer 121(15):2544–2552
Graham PJ, Brar MS, Foster T, McCall M, Bouchard-Fortier A, Temple W, Quan ML (2015) Neoadjuvant chemotherapy for breast cancer, is practice changing? A population-based review of current surgical trends. Ann Surg Oncol 22(10):3376–3382
Breast Cancer Guideline https://www.oncoline.nl/uploaded/docs/mammacarcinoom/Dutch%2520Breast%2520Cancer%2520Guideline%25202012.pdf
Mureau MAM, Group BRGW (2018) Dutch breast reconstruction guideline. J Plast Reconstr Aesthet Surg 71(3):290–304
van Bommel ACM, Schreuder K, Veenstra RK, de Ligt KM, Vrancken Peeters MTFD, Maduro JH, Siesling S, Mureau MAM (2018) Discrepancies between surgical oncologists and plastic surgeons in patient information provision and personal opinions towards immediate breast reconstruction. Ann Plast Surg 81(4):383–388
Jeevan R, Mennie JC, Mohanna PN, O'Donoghue JM, Rainsbury RM, Cromwell DA (2016) National trends and regional variation in immediate breast reconstruction rates. Br J Surg 103(9):1147–1156
Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM (2017) Breast reconstruction after mastectomy: a ten-year analysis of trends and immediate postoperative outcomes. Breast 32:7–12
Flitcroft K, Brennan M, Costa D, Spillane A (2016) Documenting patterns of breast reconstruction in Australia: the national picture. Breast 30:47–53
Mylvaganam S, Conroy E, Williamson PR, Barnes NLP, Cutress RI, Gardiner MD, Jain A, Skillman JM, Thrush S, Whisker LJ et al (2017) Variation in the provision and practice of implant-based breast reconstruction in the UK: results from the iBRA national practice questionnaire. Breast 35:182–190
Brennan ME, Spillane AJ (2013) Uptake and predictors of post-mastectomy reconstruction in women with breast malignancy–systematic review. Eur J Surg Oncol 39(6):527–541
de Ligt KM, van Bommel ACM, Schreuder K, Maduro JH, Vrancken Peeters MTFD, Mureau MAM, Siesling S, Group NBCAW (2018) The effect of being informed on receiving immediate breast reconstruction in breast cancer patients. Eur J Surg Oncol 44(5):717–724
Schreuder K, van Bommel ACM, de Ligt KM, Maduro JH, Vrancken Peeters MTFD, Mureau MAM, Siesling S (2017) Hospital organizational factors affect the use of immediate breast reconstruction after mastectomy for breast cancer in the Netherlands. Breast 34:96–102
Litière S, Werutsky G, Fentiman IS, Rutgers E, Christiaens MR, Van Limbergen E, Baaijens MH, Bogaerts J, Bartelink H (2012) Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol 13(4):412–419
Siesling S, Tjan-Heijnen VC, de Roos M, Snel Y, van Dalen T, Wouters MW, Struikmans H, van der Hoeven JJ, Maduro JH, Visser O (2014) Impact of hospital volume on breast cancer outcome: a population-based study in the Netherlands. Breast Cancer Res Treat 147(1):177–184
Gooiker GA, van Gijn W, Post PN, van de Velde CJ, Tollenaar RA, Wouters MW (2010) A systematic review and meta-analysis of the volume-outcome relationship in the surgical treatment of breast cancer. Are breast cancer patients better of with a high volume provider? Eur J Surg Oncol 36(Suppl 1):S27–S35
Van Leersum NJ, Snijders HS, Henneman D, Kolfschoten NE, Gooiker GA, ten Berge MG, Eddes EH, Wouters MW, Tollenaar RA, Bemelman WA et al (2013) The Dutch surgical colorectal audit. Eur J Surg Oncol 39(10):1063–1070
Jaarrapportage 2017. https://dica.nl/jaarrapportage-2017
Christiansen P, Carstensen SL, Ejlertsen B, Kroman N, Offersen B, Bodilsen A, Jensen MB (2018) Breast conserving surgery versus mastectomy: overall and relative survival-a population based study by the Danish Breast Cancer Cooperative Group (DBCG). Acta Oncol 57(1):19–25
Funding
This study was supported by funding of the Michael van Vloten Foundation, Nijbakker-Morra Foundation and the Leids University Foundation / Van Trigt Foundation (Grant No. W18232-2-55).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author M.B. Jensen declares institutional research support from NanoString and institutional research support from Oncology Venture. All other authors declare that they have no conflicts of interest.
Ethical approval
The scientific committee of the NBCA and the DBCG Board, and the RKKP approved this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The Danish Breast Cancer Clinical Quality Database is approved by the Danish Health Authority (Sundhedsdatastyrelsen). The DBCG holds permission to collect, store, and process data on all patients diagnosed with invasive breast cancer in Denmark, and the programme is exempt from patient consent to data collection. According to the Dutch law, all breast cancer patients are included in the NBCA database, unless the patient has objected to be registered. Therefore, informed consent is not applicable for the current register-based research that does not involve contact with study participants or biological samples.
Role of funding source
Funding sources had no role in the study design, data collection, analysis, interpretation of the data, writing of the manuscript, or the decision to publish.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heeg, E., Jensen, M.B., Mureau, M.A.M. et al. Breast-contour preserving procedures for early-stage breast cancer: a population-based study of the trends, variation in practice and predictive characteristics in Denmark and the Netherlands. Breast Cancer Res Treat 182, 709–718 (2020). https://doi.org/10.1007/s10549-020-05725-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05725-z