Abstract
A mold-cast polydimethylsiloxane (PDMS) confined window was integrated with a poly-silicon wire (PSW) ion sensor. The PSW sensor surface inside the confined window was coated with a 3-aminopropyltriethoxysilane (γ-APTES) sensitive layer which allowed a single living cell to be cultivated. The change in the microenvironment due to the extracellular acidification of the single cell could then be determined by measuring the current flowing through the PSW channel. Based on this, the PSW sensor integrated with a confined sensitive window was used to detect the apoptosis as well as the effect of anti-cancer medicines on the single living non-small-lung-cancer (NSLC) cells including lung adenocarcinoma cancer cells A549 and H1299, and lung squamous-cell carcinoma CH27 cultivated inside the confined window. Single human normal cells including lung fibroblast cells WI38, lung fibroblast cells MRC5, and bronchial epithelium cell Beas-2B were tested for comparison. Two targeted anti-NSCLC cancer medicines, Iressa and Staurosporine, were used in the present study. It was found that the PSW sensor can be used to accurately detect the apoptosis of single cancer cells after the anti-cancer medicines were added. It was also found that Staurosporine is more effective than Iressa in activating the apoptosis of cancer cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Recent advances in molecular medicine have identified several molecular targets within the cancer cell regulation cycle as a basis for anti-cancer treatments. New agents aimed at target-specific intracellular pathways related to the distinctive properties of cancer cells such as angiogenesis inhibitors, epidermal growth factor receptor (EGFR) inhibitors, and protein kinase C (PKC) inhibitors (Bertrand et al. 2002; Yeow et al. 2006; Gallego et al. 2004; Rosell et al. 2004; Fabian et al. 2005; Maemondo et al. 2010) have been developed and tested. At the same time, in vitro testing of cancer cells treated with anti-cancer medicines using cell-based assays has become the usual way for developing anti-cancer medicines for the past 10 years. One of the key factors in developing anti-cancer medicines is activating the apoptosis mechanism of the cancer cells. Many reports have pointed out that manipulating the intrinsic pathway for mitochondria-dependent apoptosis activation is an efficient way for cancer cells treatment (Shi 2001). Upon anti-cancer medicine treatment, the mitochondrial proteins cytochrome c (cyt-c) and Smac protein/Direct Inhibitor of Apoptosis (IAP) binding protein with low isoelectric point (pI) (DIABLO) are released into the cytosol. Here they synergistically activate capiases by activating apoptotic protease activating factor 1 (APAF-1) and relieving the apoptotic inhibition by IAPs (Tafani et al. 2002; Lagadic-Gossmann et al. 2004; Chi and Pizzo 2006; Gong et al. 2007; Cragg et al. 2007; Chang et al. 2008). Some chemosensitive testing techniques such as enzyme-linked immunosorbent assay (ELISA), immunofluorescence analysis (IFA) and immunoblotting technique (IMB) were developed for the study of mitochondria-dependent apoptosis of cancer cells after they were treated with targeted anti-cancer medicines (Tafani et al. 2002; Lagadic-Gossmann et al. 2004; Chi and Pizzo 2006; Gong et al. 2007; Cragg et al. 2007; Chang et al. 2008). Several targeted anti-cancer medicines, such as Iressa and Staurosporine were developed based on this mechanism. In addition, it has been shown that Na+/H+ exchanger (NHE) activity or the reversal of mitochondrial FoF1-ATPase in cancer cells becomes regulated after being treated with Iressa or Staurosporine, thereby causing extracellular pH value changes and activating the apoptosis (Tafani et al. 2002; Lagadic-Gossmann et al. 2004). However, testing of anti-cancer medicines using ELISA, IFA or IMB is time consuming and requires adding labeling agents. Besides, the traditional biomedical characterization of cells often deals with a large population of cells which overlooks the information of the heterogeneity of individual cells and is likely to lead to some misleading conclusions (Ferrell and Machleder 1998; Teruel and Meyer 2002; Helmke and Minerick 2006). On the other hand, apoptosis occurs and should be detected at the single cell level (Kannan and Jain 2000).
In our previous studies we successfully demonstrated that a PSW ion sensor can be used for pH, glucose and DNA detections with good linearity, ultra-high sensitivity and ultra-low detection limit (Hsu et al. 2009; Wu et al. 2010; Wu et al. 2011a, 2011b, 2011c). We also proved that the PSW sensor inside a PDMS confined sensitive window was able to detect the adhesion, apoptosis and extracellular acidification of a single cell cultivated inside the confined window (Wu et al. 2011a). Since the activation of mitochondria-dependent apoptosis is always accompanied with extracellular changes in pH value, the PSW sensor with a confined sensitive window is therefore able to detect the effect of anti-cancer medicines on the single cancer cells cultivated inside the confined window. In the present study, human normal cells WI38, MRC5, and Beas-2B, as well as NSCLC cells A549, H1299, and CH27, were cultivated separately inside the confined sensitive window. They were cultivated with and without adding the targeted anti-cancer medicines, the EGFR inhibitor - Iressa or the PKC inhibitor - Staurosporine, respectively, into the culture mediums. The current flowing through the PSW channel was measured and then the current change in the PSW channel before and after being treated with the anti-cancer medicine was determined.
2 Materials and methods
2.1 PSW sensor fabrication
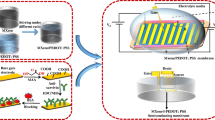
A P-type (100) silicon wafer was used as the substrate in this work. After standard RCA clean (Kern and Puotinen 1970), a 12 nm-thick thermal oxide was grown at 900 °C. A phosphorous-doped polysilicon layer with a thickness of 80 nm was then deposited onto the oxide layer at 620 °C by vertical furnace and having a sheet resistance of 40–50 Ω/square. An e-beam writer was used to define the pattern of the PSW. After development, the poly-Si wire was obtained by reactive-ion etching. The line width and length of the PSW were 200 nm and 3 μm, respectively. With the help of an optical microscope, a 1 μL γ-APTES ethanol solution (1 %) was dropped onto the PSW surface using a micropipette, followed by a 120 °C, 5 min curing process to improve the adhesion of the living cell with the PSW surface (Lee et al. 2005). The γ-APTES layer covered about 0.132 mm2 in the central area of the PSW surface, which is about the same size of a single cell and ensured single cell adhesion. A square mold measuring 200 μm × 200 μm × 400 μm was used for the fabrication of the confined window, which was first defined and developed by standard photolithographic process using the negative photoresist SU-8-2150 (Microchem, U.S.A.). After curing at 200 °C for 30 min, a PDMS solution (Sylgard 184, Dow Corning) mixed with Sylgard 184 curing agent in a 10:1 ratio was then poured into the square photoresist mold. This was then followed by a 65 °C, 12 h curing process in vacuum. After being peeled off from the mold, the PDMS confined window was subjected to UV irradiation (with a wavelength λ = 365 nm) for 40 min to convert it from being hydrophobic to hydrophilic (Schnyder et al. 2003; Berdichevsky et al. 2004). Then, with the help of an optical microscope, the PDMS confined window was placed and adhered onto the γ-APTES coated PSW surface. Figure 1(a) illustrates the fabrication process of the PDMS confined window onto the γ-APTES coated PSW surface. Figure 1(b) shows the top-view, using an optical microscope, of the PSW sensor integrated with a confined sensitive window as well as the center part of the PSW sensor, using a scanning electron microscope. The side gates of the PSW sensor were not used in this work. After being placed into an autoclave sterilizer for sterilization at 110 °C for 90 min in vacuum, the PSW sensor with a confined window was then ready for cell culture.
(a) Schematic diagram illustrating the fabrication and installation process of the PDMS confined sensitive window. (b) Top-view of the PSW sensor integrating a confined sensitive window using an optical microscope and the image of the center part of the PSW sensor using a scanning electron microscope
2.2 Cell culture
Before cultivating the cells on the surface of the PSW sensor, different cell lines were cultured in their respective culture medium. In other words; the WI38 was in a 5 mL Eagle’s minimum essential medium (MEM) containing 10 % fetal bovine serum (FBS) supplemented with 10 mL/L penicillin/streptomycin and 10 mL/L L-glutamine (Life Technologies, Inc., Frederick, MD); the MRC5 was in a 5 mL Eagle's Basal Medium (BME) containing 10 % FBS supplemented with non-essential amino acid with 2 mM L-glutamine (Life Technologies, Inc., Frederick, MD); the Beas-2B (obtained from the American Type Culture Collection, Manassas, VA) was in a 5 mL RPMI 1640 medium (Invitrogen; U.S.A.); the A549 and H1299 (obtained from the American Type Culture Collection, Manassas, VA) were in a 5 mL Dulbecco’s modified Eagle’s medium (DMEM) containing 10 % FBS supplemented with penicillin (50 units/mL) and streptomycin (50 μg/mL); and the CH27 was in a 5 mL RPMI 1640 medium containing 10 % FBS supplemented with 2 mM L-glutamine/antibiotic-antimycotic and 2 g/L sodium bicarbonate, all in a 100 mm tissue culture plate. All the culture mediums had a pH value of 7.2. All the cell lines were cultured in an incubator with 5 % CO2 at 37 °C. After cultivating the cancer cells for 3 days and the normal cells for 7 days, each cell line was seeded (2μL) separately into the confined windows located on the surface of the PSW sensor by micropipette. After 1 h cultivation in an incubator with 5 % CO2 at 37 °C to assure cell adhesion on the γ-APTES surface, the excessive cells that adhered outside the γ-APTES region in the confined window were carefully washed off by a phosphate buffer solution (PBS) (Wu et al. 2011a). It has been reported that cells can have better attachment and higher survival rate when cultured on a substrate surface containing amine (NH2) group (Valentini et al. 1994). Therefore, only a single cell was left in the confined window after removal of the excessive cells because the γ-APTES could provide rich NH2 bonds on its surface and its area was about the same size of a single cell. The PSW was then placed in the incubator with 5 % CO2 at 37 °C for another 24 h cultivation, to ensure that the single cell fully adhered to the γ-APTES surface inside the confined sensitive window (Wu et al. 2011a). Figure 2 (a) shows the top-view images, using an optical microscope, of the single NSCLC cells A549, H1299, and CH27 as well as the single normal cells Beas-2B, MRC5, and WI38 which were successfully cultivated inside the confined sensitive window on the surface of the PSW sensor, respectively.
(a) Top-view images, using an optical microscope, of the PSW sensor integrated with a confined sensitive window inside of which single isolated cancer cells A549, H1299, and CH27, as well as single isolated normal cells Beas-2B, MRC5 and WI38 were cultured successfully. (b) Schematic diagram of the overall setup needed for the measurement
2.3 Sensor characterization and anti-cancer medicine test
After the 24 h cell cultivation, the drain-source current IDS flowing through the PSW channel was measured by applying DC biases between the source (S) and the drain (D) terminals, using the semiconductor parameter analyzer Agilent 4156 C. Then the differences in the current with and without single cell cultivated inside the confined window, i.e., ΔIcell = IDS (with single cell) – IDS (without single cell), were obtained. All the electrical measurements were carried out in a light-sealed probe station. Figure 2(b) shows the schematic diagram of the overall setup for taking the measurement. No bias was applied between the side gates during the measurements.
For the anti-cancer medicine tests, 10μL Iressa and Staurosporine (Sigma-Aldrich, U.S.A.) solutions of different concentrations were prepared and added separately into 5 mL of the corresponding culture medium for each cell line (Bertrand et al. 2002; Wu et al. 2010, 2006; Gallego et al. 2004; Rosell et al. 2004; Fabian et al. 2005; Maemondo et al. 2010). The anti-medicine-containing culture medium was then used to replace the original medicine-free culture medium inside the confined window containing a single NSCLC cell or a single normal cell cultivated for 24 h. The IDS flowing through the PSW channel was measured in order to determine the channel current change ΔIcell as a function of time. From the ΔIcell vs. time curve, the apoptosis of the cancer cells was then determined to start from the time the ΔIcell began to drop. Fifteen samples were registered for each measurement in this work.
3 Results and discussion
3.1 Characterization of single cells
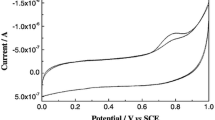
As reported in our previous paper (Wu et al. 2011a), the PSW sensor with an isolation window is able to detect a single cell in the confined window. Figure 3(a) shows the channel current change ΔIcell, measured at VDS = 5 V, of the PSW sensor for different cell lines as a function of time starting from each single cell being seeded into the confined sensitive window. It is evident that within the first 24 h the ΔIcell’s for all the cancer cell lines increase rapidly with time, while all the normal cell lines increase only slowly with time. This indicates that the cancer cell lines have a higher extracellular acidification rate than the normal cell lines. It is also obvious that the ΔIcell’s for both the cancer and the normal cell lines saturate after 24 h, and that the ΔIcell’s of all cancer cells are higher than those of the normal cells. This suggests that the cancer cells produce more H+ ions than the normal cell lines. These results are consistent with those of the reports in (Gillies et al. 1994; McCoy et al. 1995; Cardone et al. 2005). The ΔIcell’s saturation after 24 h for both the cancer and the normal cells reveals that all the cell lines take at least 24 h to completely adhere to the surface of the PSW. In order to make sure that what we had obtained was not caused by surface degradation of the culture mediums, as reported in our previous paper (Wu et al. 2011a), we measured the PSW channel current changes with and without culture medium inside the confined window, i.e., ΔImedium = IDS (with culture medium) – IDS (without culture medium), as a function of time at VDS = 5 V for each culture medium, DMEM, BME, MEM and RPMI1640, without a cell in them. The results are shown in Fig. 3 (b) (Wu et al. 2011a). Apparently, none of the cell-free culture mediums cause any degradation of the PSW surface, not even after 50 h.
Channel current changes ΔI of the PSW sensor measured at VDS = 5 V for (a) single normal cells and cancer cells cultivated from the very beginning of seeding the single cell into the confined sensitive window, and (b) their respective cell-free culture mediums as a function of time (Wu et al. 2011a)
Figure 4(a) shows the channel current change ΔIcell as a function of drain-source voltage VDS for single normal and cancer cells cultivated for 24 h inside the confined sensitive window. This 24 h cultivation is needed to ensure that the single cells are completely adhered to the PSW surface (Wu et al. 2011a). It was found that the ΔIcell’s for both the normal cells and the cancer cells increase almost linearly with the applied voltage VDS after a certain threshold voltage is reached. It was observed again that at any voltage, the cancer cells induced higher ΔIcell’s than the normal cells, indicating that the cancer cells produce higher extracellular acidification than the normal cells. We once again measured and compared the ΔImedium vs. VDS characteristics for each cell-free culture medium shown in Fig. 4(b), to ensure that the obtained ΔIcell’s shown in Fig. 4(a) were not the result of surface degradation caused by the culture mediums. We found that the cell-free mediums did not cause any ΔImedium’s degradation across the entire range of measured VDS.
Since extracellular acidification stops once the cell apoptosis is activated, we had to make sure that the PSW sensor was able to detect the apoptosis of the single cells cultivated inside the confined sensitive window. As noted previously, the ΔIcell’s for both the cancer and the normal cell lines saturate after 24 h. Figure 5(a) shows the saturation current changes ΔIcell’s measured at VDS = 5 V of both the single cancer cells and the normal cells cultivated inside the confined sensitive window as a function of time, with time zero taken as the time after 24 h cultivation in the incubator with 5 % CO2 at 37 °C, that is to say, after the cells were completely adhered to the PSW surface. We found that initially all the ΔIcell’s remained unchanged for both the cancer and the normal cells. The ΔIcell’s for the cancer cells however, began to drop after 4.5 h and became zero after 5.5 h, while those for the normal cells began to drop after 3 h and became zero after 4 h. The fact that the ΔIcell’s dropped to zero is believed to be caused by the apoptosis of the cells. It should be noted that all the electrical measurements in this work were carried out in atmospheric environment rather than in an incubator due to the limited electrical measurement setup. The excessive oxygen in atmospheric environment could trigger the apoptosis of the cells much earlier (Kannan and Jain 2000), which explained why the apoptosis of the single cells was activated within hours as shown in Fig. 5(a). In order to ensure that the ΔIcell’s dropping to zero was due to the apoptosis of the cells instead of cell detachment, we took the images by an optical microscope of the cancer cells and the normal cells cultivated inside the confined window before and after the ΔIcell’s dropped to zero. As reported in our previous work (Wu et al. 2011a), the images are shown in Fig. 5(b) and the cell apoptosis is confirmed. It should be noted that the extracellular H+ ions can only build up on the external surface of the cell membrane (Matsuyama and Reed 2000), and that they do not dissolve into the culture medium. Consequently, the apoptosis of a cell does not result in H+ ions accumulating on the outer surface of the cell membrane, hence a zero PSW channel current change (Baumann et al. 1999; Cardone et al. 2005; Moreno-Sanchez et al. 2007).
(a) Saturation current changes ΔI of the PSW sensor as a function of time measured at VDS = 5 V, of single cancer cells and normal cells cultivated inside the confined sensitive window, with time zero taken as the time after 24 h of cultivation in the incubator with 5 % CO2 at 37 °C. (b) Photographs taken by optical microscope of cancer cells and normal cells cultivated inside the confined sensitive window before and after the saturation current changes dropped to zero (Wu et al. 2011a)
3.2 Anti-cancer medicine test
Figures 6(a) and 6(b) show the saturation current change ΔIcell’s of the PSW as a function of time measured at VDS = 5 V for single cancer cells, A549, H1299, and CH27. These cancer cells were cultivated inside the confined sensitive window after their respective medicine-free culture mediums were replaced with Iressa-containing culture medium and Staurosporine-containing culture medium, respectively, with different concentrations (1, 10, and 100 nM). For the sake of comparison, the ΔIcell’s vs. time curves for the single cancer cells cultivated in their respective medicines-free culture mediums (control) are also shown in Fig. 6(a) and (b). It is evident that there is almost no change in the ΔIcell’s for the single cancer cells cultivated in medicine-free culture mediums, while those cultivated in anti-cancer-medicine-containing culture mediums decrease rapidly with time. As observed, increasing the concentration of the anti-cancer medicine in the culture medium accelerates the decrease of the ΔIcell’s. Even for a concentration as small as 1 nM, the ΔI took about 2.25 h for A549, 1.75 h for H1299, and 1.25 h for CH27 to drop to zero after their respective culture mediums were replaced with Iressa-containing culture mediums, while it took only about 1.5 h for A549, 1.0 h for H1299, and 0.75 h for CH27 to drop to zero after their respective culture mediums were replaced with Staurosporine-containing culture mediums. Images taken by optical microscope of the cancer cells cultivated inside the confined window after the ΔIcell’s dropped to zero confirm that the ΔIcell’s dropping to zero resulted from the apoptosis of the cells rather than from cell detachment. In order to ensure that the ΔIcell drop is not caused by the degradation of the PSW surface due to long-term immersion in anti-cancer medicine with added culture mediums, we measured the ΔImedium’s vs. the time curves for the cell-free culture mediums with 100 nM Iressa and Staurosporine, respectively, as shown in Fig. 7 (a) and (b). No apparent change in ΔImedium’s was observed after more than 5 h immersion of the PSW sensor surface in any of the cell-free but with medicine-added culture mediums. This result indicates that the ΔIcell’s drop shown in Fig. 6 is strictly due to the addition of the anti-cancer medicines. We found that A549 had the longest survival time among the three cancer cells under the treatment of either Iressa or Staurosporine. This is consistent with those reports that found that the malignancy of A549 is much more severe than that of H1299 and CH27 (Su et al. 2006; Huang et al. 2009). By taking a zero channel current change as the criterion for cell apoptosis and then compare that with the time required for the natural death of the cells to occur as shown in Fig. 5, we could be sure that adding either Iressa or Staurosporine into the culture medium activated the apoptosis of the cancer cells. We also noticed that the Staurosporine is more effective than Iressa in activating the apoptosis of the NSCLC cells. This also suggests that a PKC inhibitor (such as Staurosporine) is more effective in suppressing the NHE activity and reducing the extracellular H+ ion concentration than an EGFR inhibitor (such as Iressa).
Channel current changes ΔI of the PSW sensor as a function of time measured at VDS = 5 V for the single NSCLC cells, A549, H1299, and CH27 cultivated inside the confined sensitive window after replacing their respective medicine-free culture mediums with (a) Iressa-containing culture medium and (b) Staurosporine-containing culture medium, and at different concentrations. In addition, the ΔI’s vs. time curves for the single cancer cells cultivated in their respective medicines-free culture mediums (control) are shown for comparison
It is well known that common anti-cancer medicines can possibly kill human normal cells as well, and therefore we conducted an experiment to check the effect of Staurosporine and Iressa on the normal cells. We replaced the respective culture mediums of the single normal cells, Beas-2B, WI38, and MRC5, separately with Iressa-containing and Staurosporine-containing culture mediums with different concentrations, and then measured the ΔIcell’s vs. culture time curves. The result is shown in Fig. 8 (a) and (b). It was evident that both of the targeted anti-cancer medicines, Iressa and Staurosporine had little effect on the human normal cells. This confirmed that both Iressa and Staurosporine were effective targeted anti-cancer medicines.
Channel current changes ΔI of the PSW sensor as a function of time measured at VDS = 5 V for the single normal cells, Beas-2B, WI38, MRC5 cultivated inside the confined sensitive window after replacing their respective medicine-free culture mediums with (a) Iressa-containing culture medium and (b) Staurosporine-containing culture medium, respectively, with different concentrations. The ΔI’s vs. time curves for the single cancer cells cultivated in their respective medicines-free culture mediums (control) are shown for comparison
To further confirm that our PSW sensor was useful for anti-cancer medicine test, we checked the single cancer cells by optical microscopy at different hours after their respective culture mediums were replaced with anti-medicine-containing culture mediums. The images of the single cells A549, H1299 and CH27 by optical microscopy, after their respective culture mediums were replaced with 100nM Iressa-containing culture mediums for 0, 1.25, 1.75 and 2.25 h. are shown in Fig. 9(a). On the other hand, those that were replaced with 100nM Staurosporine-containing culture mediums for 0, 0.75, 1 and 1.5 h are shown in Fig. 9(b). We found that 1.25 h after adding the Iressa, CH27 exhibited near cell apoptosis, but both A549 and H1299 showed only some changes in cell morphology. After adding Iressa, the time required for apoptosis of H1299 and A549 was about 1.75 h and 2.25 h, respectively. For the treatment of Staurosporine, it took only about 0.75 h for CH27, 1 h for H1299 and 1.5 h for A549 to show apoptosis. This is consistent with our measurement data shown in Fig. 6.
4 Conclusions
In this paper, we reported the effect of adding targeted anti-cancer medicines to the extracellular acidification of single cancer cells cultivated inside a confined sensitive window installed on a PSW ion sensor surface. We found that each single cell has its own characteristic PSW channel current change ΔIcell which is related to the extracellular acidification of the single cell. Our results showed that after 24 h cultivation on the PSW surface, all single cancer cells had higher ΔIcell than the single normal cells, indicating that the extracellular acidification of cancer cells was stronger than that of normal cells. The proposed PSW sensor correctly detected the apoptosis of the single cells cultivated inside the confined sensitive window by observing the PSW channel current change drop to zero as a result of the extracellular acidification being suppressed when cell apoptosis was activated. In this work we also confirmed that adding targeted anti-cancer medicines only activates the apoptosis of the NSCLC cells but not the normal cells. The results of our experiment showed that the PKC-inhibitor Staurosporine is more effective than the EGFR inhibitor Iressa in activating the apoptosis of the cancer cells. In conclusion, the PSW ion sensor combined with a confined sensitive window is an effective tool for the detection of extracellular acidification of a single cell and can be used in the development of new anti-cancer medicines.
References
W.H. Baumann, M. Lehmann, A. Schwinde, R. Ehret, M. Brischwein, B. Wolf, Sens. Actuators B Chem. 55, 77–89 (1999)
Y. Berdichevsky, J. Khandurina, A. Guttman, Y.J. Lo, Sens. Actuators B Chem. 97, 402–408 (2004)
J. Bertrand, M. Philippe, F. Pierre, K. Guido, L. Rolf, Z. Boris, Oncogene 21, 65–77 (2002)
R.A. Cardone, V. Casavola, S.J. Reshkin, Nat. Rev. Cancer 5, 786–795 (2005)
G.C. Chang, C.T.R. Yu, C.H. Tsai, J.R. Tsai, J.C. Chen, C.C. Wu, W.J. Wu, S.L. Hsu, Eur. J. Pharmacol. 600, 37–44 (2008)
S.L. Chi, S.V. Pizzo, Cancer Res. 15, 875–882 (2006)
M.S. Cragg, J. Kuroda, H. Puthalakath, D.C.S. Huang, A. Strasser, PLos Med. 4, 1681–1690 (2007)
M.A. Fabian, W.H. Biggs, D.K. Treiber, C. EAtteridge, M.D. Azimioara, M.G. Benedetti, T.A. Carter, P. Ciceri, P.T. Edeen, M. Floyd, J.M. Ford, M. Galvin, J.L. Gerlach, R.M. Grotzfeld, S. Herrgard, D.E. Insko, M.A. Insko, A.G. Lai, J. Lélias, S.A. Mehta, Z.V. Milanov, A.M. Velasco, L.M. Wodicka, H.K. Patel, P.P. Zarrinkar, D.J. Lockhart, Nat. Biotech 23, 329–336 (2005)
J.E. Ferrell, E.M. Machleder, Science 280, 895–898 (1998)
M. Gallego, B. Joseph, T.H. Hemstrom, S. Tamiji, L. Mortier, G. Kroemer, P. Formstecher, B. Zhivotovsky, P. Marchetti, Oncogene 23, 6282–6291 (2004)
R.J. Gillies, Z. Liu, Z. Bhujwalla, Am. J. Physiol. 267, C195–C203 (1994)
Y. Gong, R. Somwar, K. Politi, M. Balak, J. Chmielecki, X. Jiang, W. Pao, PLos Med. 4, 1655–1668 (2007)
B.P. Helmke, A.R. Minerick, Proc. Natl. Acad. Sci. U.S.A. 103, 6419–6424 (2006)
P.Y. Hsu, J.J. Lin, Y.L. Wu, W.C. Hung, A.G. Cullis, Sens. Actuators B Chem. 142, 273–279 (2009)
C.Y. Huang, Y.C. Fong, C.Y. Lee, M.Y. Chen, H.C. Tsai, H.C. Hsu, C.H. Tang, Biochem. Pharmacol. 77, 794–803 (2009)
K. Kannan, A.K. Jain, Pathophysiology 7(27), 153–163 (2000)
W. Kern, D.A. Puotinen, RCA Rev. 31, 187–206 (1970)
D. Lagadic-Gossmann, L. Huc, V. Lecureur, Cell Death Differ. 11, 953–961 (2004)
M.H. Lee, D.A. Brass, R. Morris, R.J. Composto, P. Ducheyne, Biomaterials 26, 1721–1730 (2005)
M. Maemondo, A. Inoue, K. Kobayashi, S. Sugawara, S. Oizumi, H. Isobe, A. Gemma, M. Harada, H. Yoshizawa, I. Kinoshita, Y. Fujita, S. Okinaga, H. Hirano, K. Yoshimori, T. Harada, T. Ogura, M. Ando, H. Miyazawa, T. Tanaka, Y. Saijo, K. Hagiwara, S. Morita, T. Nukiwa, The New Eng. J. Med. 362, 2380–2388 (2010)
S. Matsuyama, J.C. Reed, Cell Death Differ. 7, 1155–1165 (2000)
C.L. McCoy, C.S. Parkins, D.J. Chaplin, J.R. Griffiths, L.M. Rodrigues, M. Stubbs, Br. J. Cancer 72, 905–911 (1995)
R. Moreno-Sanchez, S. Rodriguez-Enriquez, A. Marin-Hernandez, E. Saavedra, FEBS J. 274, 1393–1418 (2007)
R. Rosell, E. Felip, R. Garcia-Campelo, C. Balana, Lung Cancer. 46, 135–148 (2004)
B. Schnyder, T. Lipperta, R. Kötza, A. Wokauna, V.-M. Graubnerb, O. Nuyken, Surf. Sci 532-535, 1067–1071 (2003)
Y. Shi, Nat. Struct. Mol. Biol. 8, 394–401 (2001)
J.L. Su, P.C. Yang, J.Y. Shih, C.Y. Yang, L.H. Wei, C.Y. Hsieh, C.H. Chou, Y.M. Jeng, M.Y. Wang, K.J. Chang, M.C. Hung, M.L. Kuo, Cancer Cell 9, 209–223 (2006)
M. Tafani, J.A. Cohn, N.O. Karpinich, R.J. Rothman, M.A. Russo, J.L. Farber, J. Biol, Chem. 277, 49569–49576 (2002)
M.N. Teruel, T. Meyer, Science 295, 1910–1912 (2002)
R.F. Valentini, T.G. Vargo, G.A. Gardella Jr., P. Aebischer, J. Biomaterials Science, Polymer Edition 5, 13–36 (1994)
Y.L. Wu, P.Y. Hsu, C.P. Hsu, W.C. Liu, J. Electrochem, Soc. 157, J191–J195 (2010)
Y.L. Wu, P.Y. Hsu, C.P. Hsu, C.C. Wang, L.W. Lee, J.J. Lin, Biomed. Microdevices 13, 939–947 (2011a)
Y.L. Wu, P.Y. Hsu, J.J. Lin, Biosens. Bioelectron. 26, 2281–2286 (2011b)
Y.L. Wu, J.J. Lin, P.Y. Hsu, C.P. Hsu, Sens. Actuators B Chem. 155, 709–715 (2011c)
W.S. Yeow, M.F. Ziauddin, J.B. Maxhimer, S. Shamimi-Noori, A. Barasl, A. Chua, D.S. Schrump, D.M. Nguyen, Potentiation of the anticancer effect of valproic acid. Br. J. Cancer 94, 1436–1445 (2006)
Acknowledgments
This work was financially supported in part by the Taichung Veterans General Hospital-National Chi Nan University Joint Research Program under contract no. TCVGH-NCNU977903 and in part by the National Science Council of Taiwan, Republic of China, under contract no. NSC 100-2221-E-260-005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, YL., Hsu, PY., Hsu, CP. et al. Detecting the effect of targeted anti-cancer medicines on single cancer cells using a poly-silicon wire ion sensor integrated with a confined sensitive window. Biomed Microdevices 14, 839–848 (2012). https://doi.org/10.1007/s10544-012-9664-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-012-9664-5