Abstract
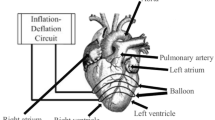
Continuous flow left ventricular assist devices (LVADs) are commonly used as bridge-to-transplantation or destination therapy for heart failure patients. However, non-optimal pumping speeds can reduce the efficacy of circulatory support or cause dangerous ventricular arrhythmias. Optimal flow control for continuous flow LVADs has not been defined and calls for an implantable pressure sensor integrated with the LVAD for real-time feedback control of pump speed based on ventricular pressure. A MEMS pressure sensor prototype is designed, fabricated and seamlessly integrated with LVAD to enable real-time control, optimize its performance and reduce its risks. The pressure sensing mechanism is based on Fabry-Pérot interferometer principle. A biocompatible parylene diaphragm with a silicon mirror at the center is fabricated directly on the inlet shell of the LVAD to sense pressure changes. The sensitivity, range and response time of the pressure sensor are measured and validated to meet the requirements of LVAD pressure sensing.









Similar content being viewed by others
References
K.M. Ainslie, T.A. Desai, Microfabricated implants for applications in therapeutic delivery, tissue engineering, and biosensing. Lab Chip 8(11), 1864–1878 (2008)
M.G. Allen, Micromachined endovascularly-implantable wireless aneurysm pressure sensors: from concept to clinic. Solid-State Sensors, Actuators and Microsystems, 2005. Digest of Technical Papers. TRANSDUCERS ’05. The 13th International Conference on. (2005)
A. Arndt, P. Nüsser et al., Physiological control of a rotary blood pump with selectable therapeutic options: control of pulsatility gradient. Artif. Organs 32(10), 761–771 (2008)
V. Arya, M. de Vries et al., Exact analysis of the extrinsic Fabry-Perot interferometric optical fiber sensor using Kirchhoff’s diffraction formalism. Opt. Fiber Technol. 1(4), 380–384 (1995)
Y. Backlund, L. Rosengren, B. Hok, B. Svedbergh, Passive silicone transensor intended for biomedical, remote pressure monitoring. Sensor. Actuator. 21(1–3), 58 (1990)
E.J. Birks, P.D. Tansley et al., Left ventricular assist device and drug therapy for the reversal of heart failure. N. Engl. J. Med. 355(18), 1873–1884 (2006)
K. Biswas, S. Kal, Etch characteristics of KOH, TMAH and dual doped TMAH for bulk micromachining of silicon. Microelectron. J. 37(6), 519–525 (2006)
L. Bowman, J.D. Meindl, The packaging of implantable integrated sensors. IEEE Trans. Biomed. Eng. 33(2), 248–255 (1986)
E.I. Bromley, J.N. Randall et al., A technique for the determination of stress in thin-films. J. Vac. Sci. Tech. B 1(4), 1364–1366 (1983)
E. Bullister, S. Reich et al., Physiologic control algorithms for rotary blood pumps using pressure sensor input. Artif. Organs 26(11), 931–938 (2002)
M.A. Chan, S.D. Collins et al., A micromachined pressure sensor with fiber-optic interferometric readout. Sensor. Actuator. A Phys. 43(1–3), 196–201 (1994)
T.Y. Chang, V.G. Yadav et al., Cell and protein compatibility of parylene-C surfaces. Langmuir 23(23), 11718–11725 (2007)
P.-J. Chen, D.C. Rodger et al., Unpowered spiral-tube parylene pressure sensor for intraocular pressure sensing. Sensor. Actuator. A Phys. 127(2), 276–282 (2006)
P.J. Chen, D.C. Rodger et al., Microfabricated implantable parylene-based wireless passive intraocular pressure sensors. J. Microelectromech. Syst. 17(6), 1342–1351 (2008)
P.-J. Chen, S. Saati et al., Wireless intraocular pressure sensing using microfabricated minimally invasive flexible-coiled LC sensor implant. J. Microelectromech. Syst. 19(4), 721–734 (2010)
S. Choi, J.R. Boston et al., Hemodynamic controller for left ventricular assist device based on pulsatility ratio. Artif. Organs 31(2), 114–125 (2007)
E. Cibula, D. Ðonlagic, Miniature fiber-optic pressure sensor with a polymer diaphragm. Appl. Opt. 44(14), 2736–2744 (2005)
E.R. Cosman, N.T. Zervas, P.H. Chapman, B.J. Cosman, M.A. Arnold, A telemetric pressure sensor for ventricular shunt systems. Surg. Neurol. 11, 287 (1979)
S. Dabral, J. Vanetten et al., Stress in thermally annealed parylene films. J. Electron. Mater. 21(10), 989–994 (1992)
W.P. Eaton, J.H. Smith, Micromachined pressure sensors: review and recent developments. Smart Mater. Struct. 6, 530–539 (1997)
S.A. Egorov, A.N. Mamaev, et al., Advanced signal processing method for interferometric fiber optic sensors with straightforward spectral detection. SPIE. (1998)
S.J. Farlow, Partial differential equations for scientists and engineers (Dover, Mineola, 1993)
N.E. Fearnot, T.G. Kozma, et al., Coated implantable medical device. USPO. (USA, 1997)
A. Ferreira, J.R. Boston et al., A control system for rotary blood pumps based on suction detection. IEEE Trans. Biomed. Eng. 56(3), 656–665 (2009)
B.B. Flick, R. Orglmeister, A portable microsystem-based telemetric pressure and temperature measurement unit. IEEE Trans. Biomed. Eng. 47(1), 12–16 (2000)
B. Fritz, J. Cysyk et al., Development of an inlet pressure sensor for control in a left ventricular assist device. ASAIO J. 56(3), 180–185 (2010)
M. Harada, Y. Qin et al., G-CSF prevents cardiac remodeling after myocardial infarction by activating the Jak-Stat pathway in cardiomyocytes. Nat. Med 11(3), 305–311 (2005)
T. Harder, T.J. Yao, et al., Residual stress in thin-film Parylene-C. Fifteenth IEEE International Conference on Micro Electro Mechanical Systems (MEMS ’02), pp. 471–474. (Las Vegas, USA, 2002).
E. Hong, R. Smith et al., Residual stress development in Pb(Zr, Ti)O-3/ZrO2/SiO2 stacks for piezoelectric microactuators. Thin Solid Films 510(1–2), 213–221 (2006a)
E. Hong, S. Trolier-McKinstry et al., Vibration of micromachined circular piezoelectric diaphragms. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 53(4), 697–706 (2006b)
J.-M. Hsu, S. Kammer, et al., Characterization of Parylene-C film as an encapsulation material for neural interface devices. Multi-Material Micro Manufacture (4M2007). (Borovets, Bulgaria, 2007).
R. John, Current axial-flow devices—the HeartMate II and Jarvik 2000 left ventricular assist devices. Semin. Thorac. Cardiovasc. Surg. 20(3), 264–272 (2008)
E. Kalvesten, L. Smith, et al., The first surface micromachined pressure sensor for cardiovascular pressure measurements. Micro Electro Mechanical Systems, 1998. MEMS 98. Proceedings., The Eleventh Annual International Workshop on (1998).
R. Krishnamani, D. DeNofrio et al., Emerging ventricular assist devices for long-term cardiac support. Nat. Rev. Cardiol. 7(2), 71–76 (2010)
W. Li, D.C. Rodger et al., Wafer-level parylene packaging with integrated RF electronics for wireless retinal prostheses. J. Microelectromech. Syst. 19(4), 735–742 (2010)
H.-W. Lo, W.-C. Kuo, et al., Recrystallized parylene as a mask for silicon chemical etching. 3rd IEEE Int. Conf. on Nano/Micro Engineered and Molecular Systems (NEMS). (Sanya, China, 2008).
B. Lu, S. Zheng et al., A study of the autofluorescence of parylene materials for [small mu]TAS applications. Lab Chip 10(14), 1826–1834 (2010)
L.W. Miller, F.D. Pagani et al., Use of a continuous-flow device in patients awaiting heart transplantation. N. Engl. J. Med. 357(9), 885–896 (2007)
W. Mokwa, Medical implants based on microsystems. Meas. Sci. Technol. 18(5), R47–R57 (2007)
W. Mokwa, U. Schnakenberg, On-chip microsystems for medical applications. Microsystem Symp. (Delft) (1998).
K.A. Murphy, M.F. Gunther et al., Quadrature phase-shifted, extrinsic Fabry-Perot optical fiber sensors. Opt. Lett. 16(4), 273–275 (1991)
T.J. Myers, M. Bolmers et al., Assessment of arterial blood pressure during support with an axial flow left ventricular assist device. J. Heart Lung Transplant. 28(5), 423–427 (2009)
T. Ohki, K. Ouriel et al., Initial results of wireless pressure sensing for endovascular aneurysm repair: The APEX Trial—Acute Pressure Measurement to Confirm Aneurysm Sac EXclusion. J. Vasc. Surg. 45(2), 236–242 (2007)
R. Puers, G. Vandevoorde, D. De Bruyker, Electrodeposited copper inductors for intraocular pressure telemetry. J. Micromech. Microeng. 10(2), 124 (2000)
B. Puers, A. Van Den Bossche et al., An implantable pressure sensor for use in cardiology. Sensor. Actuator. A Phys. 23(1–3), 944–947 (1990)
A.O. Ragheb, B.L. Bates, et al., Coated implantable medical device. USPO. (USA, 2001)
R.A.M. Receveur, F.W. Lindemans et al., Microsystem technologies for implantable applications. J. Micromech. Microeng. 17(5), R50–R80 (2007)
D.C. Rodger, J.D. Weiland et al., Scalable high lead-count parylene package for retinal prostheses. Sensor. Actuator. B Chem. 117(1), 107–114 (2006)
J.G. Rogers, K.D. Aaronson et al., Continuous flow left ventricular assist device improves functional capacity and quality of life of advanced heart failure patients. J. Am. Coll. Cardiol. 55(17), 1826–1834 (2010)
K. Sato, M. Shikida et al., Anisotropic etching rates of single-crystal silicon for TMAH water solution as a function of crystallographic orientation. Sensor. Actuator. A Phys. 73(1–2), 131–137 (1999)
H. Schima, M. Vollkron et al., First clinical experience with an automatic control system for rotary blood pumps during ergometry and right-heart catheterization. J. Heart Lung Transplant. 25(2), 167–173 (2006)
E. Schmidt, J. McIntosh et al., Long-term implants of Parylene-C coated microelectrodes. Med. Biol. Eng. Comput. 26(1), 96–101 (1988)
U. Schnakenberg, C. Krüger et al., Intravascular pressure monitoring system. Sensor. Actuator. A Phys. 110(1–3), 61–67 (2004)
J.P. Seymour, Y.M. Elkasabi et al., The insulation performance of reactive parylene films in implantable electronic devices. Biomaterials 30(31), 6158–6167 (2009)
C.Y. Shih, T.A. Harder et al., Yield strength of thin-film parylene-C. Microsyst. Technol. 10(5), 407–411 (2004)
M.S. Slaughter, J.G. Rogers et al., Advanced heart failure treated with continuous-flow left ventricular assist device. N. Engl. J. Med. 361(23), 2241–2251 (2009)
D.S. Soane, Z. Martynenko, Polymers in microelectronics, (Elsevier Science Ltd., 1989)
N. Stark, Literature review: biological safety of parylene C. Med. Plast. Biomater. 3(2), 30–35 (1996)
O. Tabata, R. Asahi et al., Anisotropic etching of silicon in TMAH solutions. Sensor. Actuator. A: Phys. 34(1), 51–57 (1992)
M.S. Taylor, J.L. Williams, Barrier coating on blood contacting devices. USPO. (USA 1991)
C.M. Terracciano, L.W. Miller et al., Contemporary use of ventricular assist devices. Annu. Rev. Med. 61, 255–270 (2010)
S. Timoshenko, S. Woinowsky-Krieger, Theory of plates and shells. (McGraw-Hill, 1959)
M. Vollkron, H. Schima et al., Development of a suction detection system for axial blood pumps. Artif. Organs 28(8), 709–716 (2004)
M. Vollkron, H. Schima et al., Advanced suction detection for an axial flow pump. Artif. Organs 30(9), 665–670 (2006)
M. Vollkron, P. Voitl et al., Suction events during left ventricular support and ventricular arrhythmias. J. Heart Lung Transplant. 26(8), 819–825 (2007)
Z. Xiao, O. Engström et al., Diaphragm deflection of silicon interferometer structures used as pressure sensors. Sensor. Actuator. A Phys. 58(2), 99–107 (1997)
H. Xiao, J. Deng et al., Single-crystal sapphire fiber-based strain sensor for high-temperature applications. J. Lightwave Technol. 21(10), 2276 (2003)
B. Yu, A. Wang et al., Analysis of fiber Fabry-Pérot interferometric sensors using low-coherence light sources. J. Lightwave Technol. 24(4), 1758 (2006)
S. Zheng, H.K. Lin, et al., A novel 3D micro membrane filtration device for capture viable rare circulating tumor cells from whole blood. The 13th in the series of Hilton Head Workshops on the science and technology of solid-state sensors, actuators, and microsystems (Hilton Head 2008). (Hilton Head Island, SC, USA, 2008)
S. Zheng, H.K. Lin et al., 3D microfilter device for viable circulating tumor cell (CTC) enrichment from blood. Biomed. Microdevices 13(1), 203–213 (2011)
Acknowledgements
The authors appreciate assistance and help from Penn State Material Research Institute (MRI) and Nanofabrication laboratory (Nanofab). We would also like to express our thanks to Mr. Gene Gerber for his help on the prototype fabrication and Dr. Donghai Wang and his student Zhongxue Chen for helping us melt the parylene-C film.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, MD., Yang, C., Liu, Z. et al. An implantable Fabry-Pérot pressure sensor fabricated on left ventricular assist device for heart failure. Biomed Microdevices 14, 235–245 (2012). https://doi.org/10.1007/s10544-011-9601-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-011-9601-z