Abstract
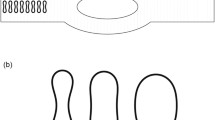
Bifurcations and confluences are very common geometries in biomedical microdevices. Blood flow at microchannel bifurcations has different characteristics from that at confluences because of the multiphase properties of blood. Using a confocal micro-PIV system, we investigated the behaviour of red blood cells (RBCs) and cancer cells in microchannels with geometrically symmetric bifurcations and confluences. The behaviour of RBCs and cancer cells was strongly asymmetric at bifurcations and confluences whilst the trajectories of tracer particles in pure water were almost symmetric. The cell-free layer disappeared on the inner wall of the bifurcation but increased in size on the inner wall of the confluence. Cancer cells frequently adhered to the inner wall of the bifurcation but rarely to other locations. Because the wall surface coating and the wall shear stress were almost symmetric for the bifurcation and the confluence, the result indicates that not only chemical mediation and wall shear stress but also microscale haemodynamics play important roles in the adhesion of cancer cells to the microchannel walls. These results provide the fundamental basis for a better understanding of blood flow and cell adhesion in biomedical microdevices.









Similar content being viewed by others
References
A.S. Ahuja, W.R. Hendee, P.L. Carson, Transport phenomena in laminar flow of blood. Phys. Med. Biol. 23, 928–936 (1978)
E. Bastida, L. Almirall, M.C. Bertomeu, A. Ordinas, Influence of shear stress on tumor-cell adhesion to endothelial-cell extracellular matrix and its modulation by fibronectin. Int. J. Cancer 43, 1174–1178 (1989)
J.G. Beeson, S.J. Rogerson, B.M. Cooke et al., Adhesion of Plasmodium falciparum-infected erythrocytes to hyaluronic acid in placental malaria. Nat. Med. 6, 86–90 (2000)
N. Casson, Rheology of Disperse System (Pergamon, London, 1959)
A.F. Chambers, A.C. Groom, I.C. MacDonald, Dissemination and growth of cancer cells in metastatic sites. Nat. Rev. Cancer 2, 563–572 (2002)
X. Chen, D.F. Cui, C.C. Liu, H. Li, Microfluidic chip for blood cell separation and collection based on crossflow filtration. Sen. Actuators B 130, 216–221 (2008)
J.A. DiVietro, D.C. Brown, L.A. Sklar, R.S. Larson, M.B. Lawrence, Immobilized stromal cell-derived factor-1alpha triggers rapid VLA-4 affinity increases to stabilize lymphocyte tethers on VCAM-1 and subsequently initiate firm adhesion. J. Immunol. 178, 3903–3911 (2007)
R. Fahraeus, T. Lindqvist, The viscosity of the blood in narrow capillary tubes. Am. J. Physiol. 96, 562–568 (1931)
I.J. Fidler, The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat. Rev. Cancer 3, 453–458 (2003)
H. Fujiwara, T. Ishikawa, R. Lima, N. Matsuki, Y. Imai, H. Kaji, M. Nishizawa, T. Yamaguchi, Red blood cell motions in high-hematocrit blood flowing through a stenosed microchannel. J. Biomech. 42, 838–843 (2009)
O.V. Glinskii, V.H. Huxley, G.V. Glinsky et al., Mechanical entrapment is insufficient and intercellular adhesion is essential for metastatic cell arrest in distant organs. Neoplasia 7, 522–527 (2005)
J. Haier, G.L. Nicolson, Tumor cell adhesion under hydrodynamic conditions of fluid flow. Acta Pathol. Microbiol. Immunol. Scand. 109, 241–262 (2001)
H.W. Hou, Q.S. Li, G.Y.H. Lee, A.P. Kumar, C.N. Ong, C.T. Lim, Deformability study of breast cancer cells using microfluidics. Biomed. Microdevices 11, 557–564 (2009)
J. Kitayama, N. Tsuno, E. Sunami, T. Osada, T. Muto, H. Nagawa, E-selectin can mediate the arrest type of adhesion of colon cancer cells under physiological shear flow. Eur. J. Cancer 36, 121–127 (2000)
S. Liang, M.J. Slattery, C. Dong, Shear stress and shear rate differentially affect the multi-step process of leukocyte-facilitated melanoma adhesion. Exp. Cell Res. 310, 282–292 (2005)
S. Liang, M.J. Slattery, D. Wagner, S.I. Simon, C. Dong, Hydrodynamic shear rate regulates melanoma-leukocyte aggregation, melanoma adhesion to the endothelium, and subsequent extravasation. Ann. Biomed. Eng. 36, 661–671 (2008)
R. Lima, S. Wada, K. Tsubota, T. Yamaguchi, Confocal micro-PIV measurements of three-dimensional profiles of cell suspension flow in a square microchannel. Meas. Sci. Technol. 17, 797–808 (2006)
R. Lima, T. Ishikawa, Y. Imai, M. Takeda, S. Wada, T. Yamaguchi, Radial dispersion of red blood cells in blood flowing through glass capillaries: role of heamatocrit and geometry. J. Biomech. 41, 2188–2196 (2008)
R. Lima, T. Ishikawa, Y. Imai, M. Takeda, S. Wada, T. Yamaguchi, Measurement of individual red blood cell motions under high hematocrit conditions using a confocal micro-PTV system. Ann. Biomed. Eng. 37, 1546–1559 (2009)
E. Meijering, I. Smal, G. Danuser, Tracking in molecular bioimaging. IEEE Signal Process Mag. 23, 46–53 (2006)
F.L. Miles, F.L. Pruitt, K.L. van Golen, C.R. Cooper, Stepping out of the flow: capillary extravasation in cancer metastasis. Clin. Exp. Metastasis 25, 305–324 (2008)
S. Mine, T. Fujisaki, C. Kawahara et al., Hepatocyte growth factor enhances adhesion of breast cancer cells to endothelial cells in vitro through up-regulation of CD44. Exp. Cell Res. 288, 189–197 (2003)
H. Mohamed, M. Murray, J.N. Turner, M. Caggana, Isolation of tumor cells using size and deformation. J. Chromatogr. A 1216, 8289–8295 (2009)
M.S. Moss, B. Sisken, S. Zimmer, K.W. Anderson, Adhesion of nonmetastatic and highly metastatic breast cancer cells to endothelial cells exposed to shear stress. J. Biorheology 36, 359–371 (1999)
S. Nagrath et al., Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature 450, 1235–1239 (2007)
G. Ostermann, K.S. Weber, A. Zernecke, A. Schroder, C. Weber, JAM-1 is a ligand of the beta(2) integrin LFA-1 involved in transendothelial migration of leukocytes. Nat. Immunol. 3, 151–158 (2002)
A.S. Popel, P.C. Johnson, Microcirculation and hemorheology. Annu. Rev. Fluid Mech. 37, 43–69 (2005)
C. Scholander, C.J. Treutiger, K. Hultenby, M. Wahlgren, Novel fibrillar structure confers adhesive property to malaria?infected erythrocytes. Nat. Med. 2, 204–208 (1996)
S.J. Tan, L. Yobas, G.Y.H. Lee, C.N. Ong, C.T. Lim, Microdevice for the isolation and enumeration of cancer cells from blood. Biomed. Microdevices 11, 883–892 (2009)
V. Thamilselvan, A. Patel, J.V. Zyp, M.D. Basson, Colon cancer cell adhesion in response to Src Kinase activation and actin-cytoskeleton by non-laminar shear stress. J. Cell. Biochem. 92, 361–371 (2004)
P. Wilding, L.J. Kricka, J. Cheng, G. Hvichia, M.A. Shoffner, P. Fortina, Integrated cell isolation and polymerase chain reaction analysis using silicon microfilter chambers. Anal. Biochem. 257, 95–100 (1998)
Acknowledgments
The authors are grateful for helpful discussions with Dr. R. Lima in Braganca Polytechnic Institute, and Prof. C. T. Lim in National University of Singapore. This study was supported by Grant-in-Aid for Scientific Research (S) from the Japan Society for the Promotion of Science (JSPS; No. 19100008) and by a Grant-in-Aid for Young Scientists (A) from the JSPS (No. 19686016). We also acknowledge the support from the 2007 Global COE Program “Global Nano-Biomedical Engineering Education and Research Network Centre”.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Distribution of RBCs and cell-free layers around the bifurcation. The movie is taken by a standard halogen light, and hematocrit is about 10%. (MOV 1345 kb)
Distribution of RBCs and cell-free layers around the confluence. The movie is taken by a standard halogen light, and hematocrit is about 10%. (MOV 1355 kb)
Appendix A: Confocal micro-PIV system
Appendix A: Confocal micro-PIV system
The confocal micro-PIV system used in this study shown in Fig. 1 consisted of an inverted microscope (IX71; Olympus, Tokyo, Japan), a confocal scanning system (CSU22; Yokogawa, Tokyo, Japan), a high-speed camera (Phantom v7.1; Vision Research, Wayne, NJ, USA), a diode-pumped solid-state (DPSS) laser (Laser Quantum, Cheshire, UK), a syringe pump (KD Scientific, Holliston, MA, USA) to achieve constant flow, a thermo plate (Tokai Hit, Shizuoka, Japan) to control the temperature and an objective lens (magnification, 20×; N.A., 0.75; W.D., 0.17 mm; Olympus). The estimated thickness of the measurement plane (optical slice thickness) was 4.97 μm. By exposing the labelled cells to the laser, the system enabled us to track individual cells inside a blood flow of up to 20% Hct with high resolution and low optical thickness. The recorded images were evaluated in Image J (NIH, Bethesda, MD, USA) using the manual tracking MtrackJ plug-in.
Rights and permissions
About this article
Cite this article
Ishikawa, T., Fujiwara, H., Matsuki, N. et al. Asymmetry of blood flow and cancer cell adhesion in a microchannel with symmetric bifurcation and confluence. Biomed Microdevices 13, 159–167 (2011). https://doi.org/10.1007/s10544-010-9481-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-010-9481-7