Abstract
Lactoferrin (LF) is abundant in human milk and plays an important role in the health of children. Bovine LF (bLF) has high homology with human LF and has been reported to have multiple biological functions. Several clinical studies have been conducted considering these properties, which reported the usefulness of bLF. This review was aimed to provide an overview of the clinical evidence in children. We searched clinical reports investigating the effects of bLF in children and identified 36 studies on the role of bLF in infections, iron metabolism, body growth, cerebral development, and fecal microbiome. Considering the accumulated evidence, bLF may contribute to the child health, particularly by suppressing or alleviating gastrointestinal and respiratory symptoms, and improving the iron status of children with anemia or those at high risk of anemia. The dose of bLF varies depending on the expected effect and target age, but may not necessarily have to be as high as human LF in human milk. Some of the beneficial effects of bLF have not been fully validated due to limited clinical evidence or being observed in the secondary analysis of some studies. Further clinical evidence would add significant value to the use of bLF in child health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lactoferrin (LF) is an iron-binding glycoprotein and well-known for its multiple biological functions such as antimicrobial and immunomodulatory activities. LF is abundant in human breast milk and its concentration is maximum during early lactation, which rapidly declines thereafter and remains relatively constant from one month to two years of lactation (Rai et al. 2014). This means that LF is an important component for infants and children even after the age of one year.
Human and bovine LF (hLF and bLF, respectively) share 69% amino acid sequence identity based on the protein sequence alignment analysis (Pierce et al. 1991), and their bioactivities as assessed in vitro or in animal models are comparable (Steijns and van Hooijdonk 2000; Lönnerdal et al. 2011). bLF is manufactured on an industrial scale and used worldwide in a variety of food products such as powdered formula. From the 1980s to the present, multiple clinical studies have been conducted in children fed bLF. In this review, we focus on clinical studies that examined the efficacy of bLF in children and provide an overview of the potential contribution of bLF intake to child health.
Materials and methods
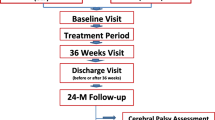
We searched clinical reports investigating the effects of bLF in children using PubMed, Google Scholar, and additional hand searching. In this review, we identified 36 studies and obtained full-length papers. The main effects discussed in these studies were protection from infection, modulation of iron metabolism, body growth, cerebral development, and regulation of the fecal microbiome.
Results and discussion
Suppressive and alleviative effects on symptoms of infections
We identified 10 published clinical studies that investigated the effects of bLF on the symptoms of infections (Table 1).
Although the methods for evaluating the outcomes varied depending on the study, 8 studies (Okuda et al. 2005; King et al. 2007; Ochoa et al. 2008, 2013; Chen et al. 2016, 2021; Motoki et al. 2020; Tsukahara et al. 2020) reported beneficial effects of bLF intake in children. Among them, seven studies (Okuda et al. 2005; Ochoa et al. 2008, 2013; Chen et al. 2016, 2021; Motoki et al. 2020; Tsukahara et al. 2020) showed suppressive or alleviative effects on gastrointestinal symptoms, and four studies (King et al. 2007; Chen et al. 2016, 2021; Motoki et al. 2020) showed such effects on respiratory symptoms.
A meta-analysis of clinical studies on adults suggested that bLF could increase the eradication rate and suppress the side effects of anti-H. pylori therapy (Zou et al. 2009). On the other hand, clinical studies on the effect of bLF on H. pylori infection in children are limited and have not yet been fully investigated (Okuda et al. 2005). As an overall trend, numerous clinical studies on H. pylori eradication by bLF were conducted in the early 2000s, but only a few studies have been conducted in recent years, probably owing to the improvement in drinking water and standard anti-H. pylori therapy.
A recent meta-analysis including studies on adults and children suggested that bLF could reduce the risk of respiratory tract infections (Ali et al. 2021) supporting the usefulness of bLF in the management of respiratory infections in children.
Based on basic research, the mechanisms underlying these protective effects of bLF can be attributed to its antibacterial, antiviral, immunomodulatory activities, and barrier functions.
bLF exhibits antibacterial activity against various bacteria mainly by sequestering iron, which is essential for bacterial growth (Arnold et al. 1977), or by directly binding with lipopolysaccharide (LPS) embedded in the gram-negative bacterial surface, leading to destabilization and permeability of the bacterial outer membrane (Drago-Serrano et al. 2012). bLF and lactoferricin, an antimicrobial peptide derived from pepsin digestion of bLF, have been demonstrated to exhibit antibacterial activity against H. pylori in vitro (Dial et al. 1998).
Antiviral properties of bLF have also been extensively studied (Oda et al. 2020a). In vitro studies have suggested that bLF exerts antiviral activity against viruses that infect the gastrointestinal tract through inhibition of viral attachment to their target cells and suppression of viral replication via interferons (IFNs) (Superti et al. 1997; Ishikawa et al. 2013; Shin et al. 2017; Oda et al. 2021).
bLF also exerts immunomodulatory effects. Intelectin, a receptor for LF, is expressed in the small intestine, particularly the epithelium overlying the Peyer’s patches (Talukder et al. 2003) where immune cells are located, suggesting that it may mediate the interaction between bLF and immune cells. In particular, orally-administered bLF activates natural killer (NK) cells via type I IFN (Kuhara et al. 2006). Moreover, bLF activates CD4+ and CD8+ T cells and enhances the production of IgA from plasma cells (Arciniega-Martínez et al. 2016). Recently, bLF has been reported to activate human plasmacytoid dendritic cells in adults, which produce type I IFN, activate NK cells, CD4+ and CD8+ T cells, and B cells, and play an important role in systemic viral clearance by modulating innate and adaptive immune responses (Miyakawa et al. 2021a). In contrast, bLF suppresses the production of inflammatory cytokines such as interleukin (IL)-6 and tumor necrosis factor (TNF)-α (Zimecki et al. 1999).
bLF induces the growth and differentiation of enterocytes, strengthens the tight junctions, and thus enhances the integrity of intestinal epithelia (Zhao et al. 2019). bLF also induces the production of type I and type III IFNs, antiviral cytokines from enterocytes (Shin et al. 2017; Miyakawa et al. 2021b).
Collectively, orally-administered bLF exerts local antibacterial and antiviral activities, local and systemic immunomodulatory activity, and strengthens the intestinal barrier, leading to suppression and alleviation of gastrointestinal and respiratory symptoms.
The dose of bLF varied in different studies, and ranged from 35.8 to 1000 mg per day. Some studies were conducted using a high dose of bLF, which is almost equivalent to the amount of hLF that infants could consume from breast milk; on the other hand, some studies were conducted using a relatively low dose of bLF as that contained in commercially available formula. In a study, dose-dependent efficacy was observed with 91.5 mg of bLF being more effective than 47.2 mg of bLF in suppressing gastrointestinal symptoms (Chen et al. 2021). While, 200 mg of bLF has been reported to prevent acute gastrointestinal and respiratory symptoms (Mizuki et al. 2020; Miyakawa et al. 2021b) and shorten the duration of infectious diseases (Oda et al. 2020b) in adults. Considering body weight, the dose of bLF might not necessarily have to be as high as that found in human breast milk to exert beneficial effects in children.
Two studies (Yen et al. 2011; Björmsjö et al. 2020) showed no beneficial effects of bLF fortification; subject characteristics, public health environment, or disease burden might have affected these results. The quality of bLF such as iron saturation, contaminant, and degradation might vary depending on the suppliers, and it might also affect the results. Properties of bLF were compared among suppliers by several in vitro assays, but no consistent features were observed (Lönnerdal et al. 2021). It is desirable to develop good in vitro assay models for each biological functions to be evaluated in human, and assess the activities of bLF prior to conducting clinical studies.
Five studies (Egashira et al. 2007; Zuccotti et al. 2009; Tolone et al. 2012; Cheng et al. 2019; Li et al. 2019) showed the beneficial effects of bLF in combination with other components often contained in breast milk or formula such as bifidobacteria, probiotics, lactulose, lysozyme, or milk fat globule membrane (MFGM), although relative contribution of each component was not determined (Table 2). Combination with other functional components may produce a synergistic positive effect on the child health.
Immunomodulatory effect
Some clinical studies have investigated the effect of bLF on immune responses in children and demonstrated its immunomodulatory effect to some extent (Table 3).
Modulation of T cells, phagocytes, monocytes, and Th1/Th2 balance has been observed in HIV-infected children after bLF intake (Zuccotti et al. 2006, 2007). However, it is uncertain whether these effects can be observed in healthy individuals. Combination of bLF with curcumin also modulated T cells and monocytes in children with recurrent respiratory tract infection (RRTI) (Zuccotti et al. 2009) (Table 2). Chen et al. observed dose-dependent effects of bLF on fecal biochemical indices such as human beta defensin 2 (HBD-2), cathelicidin LL-37, secretory IgA (sIgA), butyrate, and calprotectin in children (Chen et al. 2021).
These immunomodulatory actions could be a mechanism underlying the suppression of diarrhea and the regulation of the microbiome. Nonetheless, there are some limitations, such as few studies, small sample size, study design, and subject characteristics, including children with illness; therefore, additional clinical studies are needed to clarify whether bLF modulates the immune responses in children.
Improvement in iron metabolism
We identified 16 published clinical studies that investigated the effect of bLF on iron metabolism (Table 4).
Among the seven studies (Fairweather-Tait et al. 1987; Schulz-Lell et al. 1991; Chierici et al. 1992; Lönnerdal and Hernell 1994; Hernell and Lönnerdal 2002; King et al. 2007; Björmsjö et al. 2020) investigating the effect of bLF in healthy and near-term newborns, five (Fairweather-Tait et al. 1987; Schulz-Lell et al. 1991; Lönnerdal and Hernell 1994; Hernell and Lönnerdal 2002; Björmsjö et al. 2020) did not show any beneficial effect on iron absorption or iron status after bLF intake during the first six months. Healthy term infants with normal birth weight are born with iron stores sufficient for their growth during the first six months of life (Dallman et al. 1980). In some of the above studies (Lönnerdal and Hernell 1994; Hernell and Lönnerdal 2002; King et al. 2007; Björmsjö et al. 2020), after intervention, hematological parameters such as hemoglobin (Hb) or serum ferritin showed relatively high values in accordance with the WHO guidelines (World Health Organization 2001). Therefore, it was suggested that bLF was administered when iron demand was not high, and these conditions might have affected the results.
During the second half of infancy, the requirement for exogenous iron rapidly increases as the infant grows. In a study of infants who were previously exclusively breastfed and assumed to be at a high risk of anemia, after 3 months of bLF intervention, the iron status, including Hb, serum ferritin, transferrin receptor-ferritin (TFR-F) index, and total body iron content (TBIC) was improved, leading to a lower prevalence of anemia, iron deficiency (ID), and iron deficiency anemia (IDA) (Chen et al. 2015a). In addition, several studies on anemic children have shown that bLF consistently improved the iron status (El-Khawaga and Abdelmaksoud 2019; Chen et al. 2020; Mikulic et al. 2020; Kamal et al. 2021; El-Asheer et al. 2021; Omar et al. 2021; Atia et al. 2021). A recent meta-analysis of studies on pregnant women suggested that bLF improved IDA (Abu Hashim et al. 2017), and these findings are consistent with the results obtained from studies on children.
The mechanisms underlying the improvement in anemia by bLF are likely related to its anti-inflammatory activity. It has been reported that a part of anemia is associated with high levels of IL-6 that upregulates hepcidin, a peptide hormone mainly synthesized by hepatocytes. Hepcidin binds to ferroportin, causes its degradation, and leads to a significant decrease in iron export from the cells into plasma, and consequently, IDA may be detected (Rosa et al. 2017). Several studies on pregnant women (Paesano et al. 2009, 2010, 2012, 2014; Lepanto et al. 2018) suggest that bLF decreases IL-6 levels, restores iron delocalization, and improves hematological parameters. Atia et al. observed a decrease in serum IL-6 and hepcidin levels in anemic children after bLF ingestion (Atia et al. 2021), which suggests that bLF improves iron metabolism in children by a mechanism similar to that reported in adults. According to the secondary analysis of some studies, ingestion of bLF protected children from infections (Chen et al. 2016, 2021). This might be attributed to the decrease in inflammatory cytokines, including IL-6.
Furthermore, Mikulic et al. reported that apo-bLF might promote dietary iron absorption in anemic infants (Mikulic et al. 2020). bLF was reported to solubilize a > 70-fold molar equivalent of iron at neutral pH in vitro (Kawakami et al. 1993), suggesting that ingested bLF could solubilize iron in the intestine, promote iron absorption, and consequently, improve anemia. Furthermore, bLF may improve intestinal iron absorption in children by promoting the maturation of intestinal epithelia (Yang et al. 2014; Hu et al. 2019).
Growth promotion
We identified 8 published clinical studies that reported the effects of bLF on anthropometric indices (Table 5).
Several studies have reported that bLF promotes body growth such as increase in height and weight (Hernell and Lönnerdal 2002; King et al. 2007; Ochoa et al. 2008; Chen et al. 2015a; Li et al. 2019).
We identified 3 published clinical studies that reported the effects of bLF with other components such as lysozyme and MFGM on anthropometric indices (Table 6). Two studies (Cheng et al. 2019; Li et al. 2019) showed the beneficial effects, although relative contribution of each component was not determined.
In a neonatal animal model, dietary bLF has been suggested to promote intestinal maturation such as the development of crypt-villus structures and mucosal barrier, and increased enzyme activity (Yang et al. 2014; Hu et al. 2019). Intestinal development is important for the digestion and absorption of nutrients; therefore, bLF might have promoted body growth by improving the absorption of nutrients. Furthermore, bLF has been reported to suppress fat accumulation and promote lipolysis (Ono et al. 2013). bLF may facilitate efficient utilization of milk fat as an energy source. However, the intake of solid food or subtle differences in the amount of total protein in the test food can also affect the infant’s body growth. To evaluate the growth-promoting effect of bLF, further studies are needed under strict control of the test food composition and considering the effects of alternative nutrient sources such as solid food.
Cerebral development and fecal microbiome
Several animal studies have suggested the potential involvement of bLF in neuroprotection, neurodevelopment, and learning. bLF administration through lactation showed a protective effect on impaired cerebral development in intrauterine growth restricted rats (Somm et al. 2014) and neuroprotective effect against hypoxia/ischemia-induced and LPS-induced brain injury (van de Looij et al. 2014; Ginet et al. 2016). bLF has also been reported to promote early cognitive function and learning in neonatal piglets (Chen et al. 2015b). On the other hand, there are limited clinical reports on the effect of bLF or bLF with other components on cerebral development (Tables 7, 8). One of them reported that bLF improved sleep quality (Miyakawa et al. 2020), but it was a secondary analysis of the study. Another reported improved neurodevelopment when bLF was administered in combination with MFGM (Li et al. 2019), but MFGM itself was also reported to have neurodevelopmental effects (Timby et al. 2014) and the net contribution of bLF did not evaluated. Due to above limitations, further clinical evidence is required.
Differences in the fecal microbiome of breastfed infants and formula-fed infants have been indicated in previous studies (Yoshioka et al. 1983; Balmer and Wharton 1989), and the association of the fecal microbiome with immune function and cerebral development has also been discussed. In vitro studies have reported that bLF exhibits antibacterial activity against a wide range of pathogenic bacteria (Jenssen and Hancock 2009), whereas bLF and its digestive peptide show bifidogenic activity, particularly against infant-representative species (Oda et al. 2013). Increased secretion of HBD-2, cathelicidin, sIgA, and butyrate by bLF may also contribute to the regulation of the microbiome (Chen et al. 2021). However, no consistent effect of bLF or bLF with other components on the fecal microbiome was observed (Tables 7, 8). Compared with other components of breast milk such as human milk oligosaccharides and sIgA, the effect of LF on the fecal microbiome may be limited.
Conclusions
bLF may contribute to the child health, particularly by suppressing or alleviating gastrointestinal and respiratory symptoms and improving the iron status of children with anemia or those at a high risk of anemia. The dose of bLF varies depending on the expected effect and target age, ranging from 35.8 to 1000 mg per day, and it may not necessarily have to be as high as that found in human breast milk. Subject characteristics, field conditions and quality of bLF may have led to inconsistent results. In addition, some beneficial effects of bLF were observed in the secondary analysis of the study. Further clinical evidence as the primary endpoint is needed to accurately describe the beneficial effects of bLF on the child health.
Data availability
The data presented in this review are openly available on PubMed, Google Scholar, and the journal website.
References
Abu Hashim H, Foda O, Ghayaty E (2017) Lactoferrin or ferrous salts for iron deficiency anemia in pregnancy: a meta-analysis of randomized trials. Eur J Obstet Gynecol Reprod Biol 219:45–52. https://doi.org/10.1016/j.ejogrb.2017.10.003
Ali AS, Hasan SS, Kow CS, Merchant HA (2021) Lactoferrin reduces the risk of respiratory tract infections: a meta-analysis of randomized controlled trials. Clin Nutr ESPEN 45:26–32. https://doi.org/10.1016/j.clnesp.2021.08.019
Arciniega-Martínez IM, Campos-Rodríguez R, Drago-Serrano ME et al (2016) Modulatory effects of oral bovine lactoferrin on the IgA response at inductor and effector sites of distal small intestine from BALB/c mice. Arch Immunol Ther Exp (warsz) 64:57–63. https://doi.org/10.1007/s00005-015-0358-6
Arnold RR, Cole MF, McGhee JR (1977) A bactericidal effect for human lactoferrin. Science 197:263–265. https://doi.org/10.1126/science.327545
Atia MM, Gama RM, Saad MA, Hamam MA (2021) Comparative study of the effects of lactoferrin versus oral iron therapy in obese children and adolescents with iron deficiency anemia. J Adv Med 33:104–114
Balmer SE, Wharton BA (1989) Diet and faecal flora in the newborn: breast milk and infant formula. Arch Dis Child 64:1672–1677. https://doi.org/10.1136/adc.64.12.1672
Balmer SE, Scott PH, Wharton BA (1989) Diet and faecal flora in the newborn: lactoferrin. Arch Dis Child 64:1685–1690. https://doi.org/10.1136/adc.64.12.1685
Björmsjö M, Hernell O, Lönnerdal B, Berglund SK (2020) Reducing iron content in infant formula from 8 to 2 mg/L does not increase the risk of iron deficiency at 4 or 6 months of age: a randomized controlled trial. Nutrients 13:E3. https://doi.org/10.3390/nu13010003
Chen K, Zhang L, Li H et al (2015a) Iron metabolism in infants: influence of bovine lactoferrin from iron-fortified formula. Nutrition 31:304–309. https://doi.org/10.1016/j.nut.2014.07.006
Chen Y, Zheng Z, Zhu X et al (2015b) Lactoferrin promotes early neurodevelopment and cognition in postnatal piglets by upregulating the BDNF signaling pathway and polysialylation. Mol Neurobiol 52:256–269. https://doi.org/10.1007/s12035-014-8856-9
Chen K, Chai L, Li H et al (2016) Effect of bovine lactoferrin from iron-fortified formulas on diarrhea and respiratory tract infections of weaned infants in a randomized controlled trial. Nutrition 32:222–227. https://doi.org/10.1016/j.nut.2015.08.010
Chen K, Zhang G, Chen H et al (2020) Dose effect of bovine lactoferrin fortification on iron metabolism of anemic infants. J Nutr Sci Vitaminol (tokyo) 66:24–31. https://doi.org/10.3177/jnsv.66.24
Chen K, Jin S, Chen H et al (2021) Dose effect of bovine lactoferrin fortification on diarrhea and respiratory tract infections in weaned infants with anemia: a randomized, controlled trial. Nutrition 90:111288. https://doi.org/10.1016/j.nut.2021.111288
Cheng WD, Wold KJ, Bollinger LB et al (2019) Supplementation with lactoferrin and lysozyme ameliorates environmental enteric dysfunction: a double-blind, randomized, placebo-controlled trial. Am J Gastroenterol 114:671–678. https://doi.org/10.14309/ajg.0000000000000170
Chichlowski M, Bokulich N, Harris CL et al (2021) Effect of bovine milk fat globule membrane and lactoferrin in infant formula on gut microbiome and metabolome at 4 months of age. Curr Dev Nutr 5:nzab027. https://doi.org/10.1093/cdn/nzab027
Chierici R, Sawatzki G, Tamisari L et al (1992) Supplementation of an adapted formula with bovine lactoferrin. 2. Effects on serum iron, ferritin and zinc levels. Acta Paediatr 81:475–479. https://doi.org/10.1111/j.1651-2227.1992.tb12277.x
Dallman PR, Siimes MA, Stekel A (1980) Iron deficiency in infancy and childhood. Am J Clin Nutr 33:86–118. https://doi.org/10.1093/ajcn/33.1.86
Dial EJ, Hall LR, Serna H et al (1998) Antibiotic properties of bovine lactoferrin on helicobacter pylori. Dig Dis Sci 43:2750–2756. https://doi.org/10.1023/A:1026675916421
Drago-Serrano ME, de la Garza-Amaya M, Luna JS, Campos-Rodríguez R (2012) Lactoferrin-lipopolysaccharide (LPS) binding as key to antibacterial and antiendotoxic effects. Int Immunopharmacol 12:1–9. https://doi.org/10.1016/j.intimp.2011.11.002
Egashira M, Takayanagi T, Moriuchi M, Moriuchi H (2007) Does daily intake of bovine lactoferrin-containing products ameliorate rotaviral gastroenteritis? Acta Paediatr 96:1242–1244. https://doi.org/10.1111/j.1651-2227.2007.00393.x
El-Asheer OM, Ahmed AG, AbdelAal Abdel Hafez Z et al (2021) Lactoferrin efficacy versus ferrous sulfate in treatment of children with iron deficiency anemia. J Child Sci 11:e199–e204. https://doi.org/10.1055/s-0041-1731073
El-Hawy MA, Abd Al-Salam SA, Bahbah WA (2021) Comparing oral iron bisglycinate chelate, lactoferrin, lactoferrin with iron and iron polymaltose complex in the treatment of children with iron deficiency anemia. Clin Nutr ESPEN. https://doi.org/10.1016/j.clnesp.2021.08.040
El-Khawaga A, Abdelmaksoud H (2019) Effect of lactoferrin supplementation on iron deficiency anemia in primary school children. IJMA 1:48–52. https://doi.org/10.21608/ijma.2019.12596.1003
Fairweather-Tait SJ, Balmer SE, Scott PH, Minski MJ (1987) Lactoferrin and iron absorption in newborn infants. Pediatr Res 22:651–654. https://doi.org/10.1203/00006450-198712000-00007
Ginet V, van de Looij Y, Petrenko V et al (2016) Lactoferrin during lactation reduces lipopolysaccharide-induced brain injury. BioFactors 42:323–336. https://doi.org/10.1002/biof.1278
Hernell O, Lönnerdal B (2002) Iron status of infants fed low-iron formula: no effect of added bovine lactoferrin or nucleotides. Am J Clin Nutr 76:858–864. https://doi.org/10.1093/ajcn/76.4.858
Hu P, Zhao F, Zhu W, Wang J (2019) Effects of early-life lactoferrin intervention on growth performance, small intestinal function and gut microbiota in suckling piglets. Food Funct 10:5361–5373. https://doi.org/10.1039/c9fo00676a
Ishikawa H, Awano N, Fukui T et al (2013) The protective effects of lactoferrin against murine norovirus infection through inhibition of both viral attachment and replication. Biochem Biophys Res Commun 434:791–796. https://doi.org/10.1016/j.bbrc.2013.04.013
Jenssen H, Hancock REW (2009) Antimicrobial properties of lactoferrin. Biochimie 91:19–29. https://doi.org/10.1016/j.biochi.2008.05.015
Johnston WH, Ashley C, Yeiser M et al (2015) Growth and tolerance of formula with lactoferrin in infants through one year of age: double-blind, randomized, controlled trial. BMC Pediatr 15:173. https://doi.org/10.1186/s12887-015-0488-3
Kamal MY, Rezk M, Hafez M (2021) A comparative study for the efficacy of lactoferrin-100 versus lactoferrin-100 and ferrous gluconate versus ferric hydroxide on iron deficiency anemia. Curr Pediatr Res 25:444–449
Kawakami H, Dosako S, Nakajima I (1993) Effect of lactoferrin on iron solubility under neutral conditions. Biosci Biotechnol Biochem 57:1376–1377. https://doi.org/10.1271/bbb.57.1376
King JC, Cummings GE, Guo N et al (2007) A double-blind, placebo-controlled, pilot study of bovine lactoferrin supplementation in bottle-fed infants. J Pediatr Gastroenterol Nutr 44:245–251. https://doi.org/10.1097/01.mpg.0000243435.54958.68
Kuhara T, Yamauchi K, Tamura Y, Okamura H (2006) Oral administration of lactoferrin increases NK cell activity in mice via increased production of IL-18 and type I IFN in the small intestine. J Interferon Cytokine Res 26:489–499. https://doi.org/10.1089/jir.2006.26.489
Lepanto MS, Rosa L, Cutone A et al (2018) Efficacy of lactoferrin oral administration in the treatment of anemia and anemia of inflammation in pregnant and non-pregnant women: an interventional study. Front Immunol 9:2123. https://doi.org/10.3389/fimmu.2018.02123
Li F, Wu SS, Berseth CL et al (2019) Improved neurodevelopmental outcomes associated with bovine milk fat globule membrane and lactoferrin in infant formula: a randomized, controlled trial. J Pediatr 215:24-31.e8. https://doi.org/10.1016/j.jpeds.2019.08.030
Lönnerdal B, Hernell O (1994) Iron, zinc, copper and selenium status of breast-fed infants and infants fed trace element fortified milk-based infant formula. Acta Paediatr 83:367–373. https://doi.org/10.1111/j.1651-2227.1994.tb18121.x
Lönnerdal B, Jiang R, Du X (2011) Bovine lactoferrin can be taken up by the human intestinal lactoferrin receptor and exert bioactivities. J Pediatr Gastroenterol Nutr 53:606–614. https://doi.org/10.1097/MPG.0b013e318230a419
Lönnerdal B, Du X, Jiang R (2021) Biological activities of commercial bovine lactoferrin sources. Biochem Cell Biol 99:35–46. https://doi.org/10.1139/bcb-2020-0182
Mikulic N, Uyoga MA, Mwasi E et al (2020) Iron absorption is greater from apo-lactoferrin and is similar between holo-lactoferrin and ferrous sulfate: stable iron isotope studies in Kenyan infants. J Nutr 150:3200–3207. https://doi.org/10.1093/jn/nxaa226
Miyakawa M, Kubo S, Oda H et al (2020) Effects of lactoferrin on sleep conditions in children aged 12–32 months: a preliminary, randomized, double-blind, placebo-controlled trial. Nat Sci Sleep 12:671–677. https://doi.org/10.2147/NSS.S263106
Miyakawa M, Kubo S, Tada A et al (2021a) Effects of bovine lactoferrin on subjective gastrointestinal symptoms related to physical conditions in healthy subjects: a randomized, double-blind, placebo-controlled trial. Jpn Pharmacol Ther 49:2187–2193
Miyakawa M, Oda H, Shin K et al (2021b) Effects of lactoferrin on gene expression of type I interferon in HT-29 cells and subjective symptoms related to physical condition in healthy adults. Jpn Pharmacol Ther 49:1501–1506
Mizuki M, Tsukahara T, Oda H et al (2020) Effects of lactoferrin on prevention of acute gastrointestinal symptoms in winter: a randomized, double-blinded, placebo-controlled trial for staff of kindergartens and nursery schools in Japan. Int J Environ Res Public Health 17:E9582. https://doi.org/10.3390/ijerph17249582
Motoki N, Mizuki M, Tsukahara T et al (2020) Effects of lactoferrin-fortified formula on acute gastrointestinal symptoms in children aged 12–32 months: a randomized, double-blind, placebo-controlled trial. Front Pediatr 8:233. https://doi.org/10.3389/fped.2020.00233
Ochoa TJ, Chea-Woo E, Campos M et al (2008) Impact of lactoferrin supplementation on growth and prevalence of Giardia colonization in children. Clin Infect Dis 46:1881–1883. https://doi.org/10.1086/588476
Ochoa TJ, Chea-Woo E, Baiocchi N et al (2013) Randomized double-blind controlled trial of bovine lactoferrin for prevention of diarrhea in children. J Pediatr 162:349–356. https://doi.org/10.1016/j.jpeds.2012.07.043
Oda H, Wakabayashi H, Yamauchi K et al (2013) Isolation of a bifidogenic peptide from the pepsin hydrolysate of bovine lactoferrin. Appl Environ Microbiol 79:1843–1849. https://doi.org/10.1128/AEM.03343-12
Oda H, Tanaka M, Abe F (2020a) Effects of lactoferrin on viral infections. Milk Sci 69:173. https://doi.org/10.11465/milk.69.173
Oda H, Wakabayashi H, Tanaka M et al (2020b) Effects of lactoferrin on infectious diseases in Japanese summer: a randomized, double-blinded, placebo-controlled trial. J Microbiol Immunol Infect. https://doi.org/10.1016/j.jmii.2020.02.010
Oda H, Kolawole AO, Mirabelli C et al (2021) Antiviral effects of bovine lactoferrin on human norovirus. Biochem Cell Biol 99:166–172. https://doi.org/10.1139/bcb-2020-0035
Okuda M, Nakazawa T, Yamauchi K et al (2005) Bovine lactoferrin is effective to suppress Helicobacter pylori colonization in the human stomach: a randomized, double-blind, placebo-controlled study. J Infect Chemother 11:265–269. https://doi.org/10.1007/s10156-005-0407-x
Omar OM, Assem H, Ahmed D, Abd Elmaksoud MS (2021) Lactoferrin versus iron hydroxide polymaltose complex for the treatment of iron deficiency anemia in children with cerebral palsy: a randomized controlled trial. Eur J Pediatr 180:2609–2618. https://doi.org/10.1007/s00431-021-04125-9
Ono T, Morishita S, Murakoshi M (2013) Novel function of bovine lactoferrin in lipid metabolism: visceral fat reduction by enteric-coated lactoferrin. PharmaNutrition 1:32–34. https://doi.org/10.1016/j.phanu.2012.11.001
Paesano R, Pietropaoli M, Gessani S, Valenti P (2009) The influence of lactoferrin, orally administered, on systemic iron homeostasis in pregnant women suffering of iron deficiency and iron deficiency anaemia. Biochimie 91:44–51. https://doi.org/10.1016/j.biochi.2008.06.004
Paesano R, Berlutti F, Pietropaoli M et al (2010) Lactoferrin efficacy versus ferrous sulfate in curing iron disorders in pregnant and non-pregnant women. Int J Immunopathol Pharmacol 23:577–587. https://doi.org/10.1177/039463201002300220
Paesano R, Pietropaoli M, Berlutti F, Valenti P (2012) Bovine lactoferrin in preventing preterm delivery associated with sterile inflammation. Biochem Cell Biol 90:468–475. https://doi.org/10.1139/o11-060
Paesano R, Pacifici E, Benedetti S et al (2014) Safety and efficacy of lactoferrin versus ferrous sulphate in curing iron deficiency and iron deficiency anaemia in hereditary thrombophilia pregnant women: an interventional study. Biometals 27:999–1006. https://doi.org/10.1007/s10534-014-9723-x
Pierce A, Colavizza D, Benaissa M et al (1991) Molecular cloning and sequence analysis of bovine lactotransferrin. Eur J Biochem 196:177–184. https://doi.org/10.1111/j.1432-1033.1991.tb15801.x
Rai D, Adelman AS, Zhuang W et al (2014) Longitudinal changes in lactoferrin concentrations in human milk: a global systematic review. Crit Rev Food Sci Nutr 54:1539–1547. https://doi.org/10.1080/10408398.2011.642422
Roberts AK, Chierici R, Sawatzki G et al (1992) Supplementation of an adapted formula with bovine lactoferrin: 1. Effect on the infant faecal flora. Acta Paediatr 81:119–124. https://doi.org/10.1111/j.1651-2227.1992.tb12186.x
Rosa L, Cutone A, Lepanto MS et al (2017) Lactoferrin: a natural glycoprotein involved in iron and inflammatory homeostasis. Int J Mol Sci 18:E1985. https://doi.org/10.3390/ijms18091985
Schulz-Lell G, Dörner K, Oldigs HD et al (1991) Iron availability from an infant formula supplemented with bovine lactoferrin. Acta Paediatr Scand 80:155–158. https://doi.org/10.1111/j.1651-2227.1991.tb11826.x
Shin K, Oda H, Wakabayashi H et al (2017) Effects of lactoferrin on the production of interferon-λ by the human intestinal epithelial cell line HT-29. Biochem Cell Biol 95:53–56. https://doi.org/10.1139/bcb-2016-0031
Somm E, Larvaron P, van de Looij Y et al (2014) Protective effects of maternal nutritional supplementation with lactoferrin on growth and brain metabolism. Pediatr Res 75:51–61. https://doi.org/10.1038/pr.2013.199
Steijns JM, van Hooijdonk AC (2000) Occurrence, structure, biochemical properties and technological characteristics of lactoferrin. Br J Nutr 84(Suppl 1):S11-17. https://doi.org/10.1017/s0007114500002191
Superti F, Ammendolia MG, Valenti P, Seganti L (1997) Antirotaviral activity of milk proteins: lactoferrin prevents rotavirus infection in the enterocyte-like cell line HT-29. Med Microbiol Immunol 186:83–91. https://doi.org/10.1007/s004300050049
Talukder MJR, Takeuchi T, Harada E (2003) Characteristics of lactoferrin receptor in bovine intestine: higher binding activity to the epithelium overlying Peyer’s patches. J Vet Med A Physiol Pathol Clin Med 50:123–131. https://doi.org/10.1046/j.1439-0442.2003.00512.x
Timby N, Domellöf E, Hernell O et al (2014) Neurodevelopment, nutrition, and growth until 12 mo of age in infants fed a low-energy, low-protein formula supplemented with bovine milk fat globule membranes: a randomized controlled trial. Am J Clin Nutr 99:860–868. https://doi.org/10.3945/ajcn.113.064295
Tolone S, Pellino V, Vitaliti G et al (2012) Evaluation of Helicobacter Pylori eradication in pediatric patients by triple therapy plus lactoferrin and probiotics compared to triple therapy alone. Ital J Pediatr 38:63. https://doi.org/10.1186/1824-7288-38-63
Tsukahara T, Fujimori A, Misawa Y et al (2020) The preventive effect of lactoferrin-containing yogurt on gastroenteritis in nursery school children-intervention study for 15 weeks. Int J Environ Res Public Health 17:E2534. https://doi.org/10.3390/ijerph17072534
van de Looij Y, Ginet V, Chatagner A et al (2014) Lactoferrin during lactation protects the immature hypoxic-ischemic rat brain. Ann Clin Transl Neurol 1:955–967. https://doi.org/10.1002/acn3.138
World Health Organization (2001) Iron deficiency anaemia: assessment, prevention and control -A guide for programme managers-. https://apps.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/index.html. Accessed 24 Jan 2022
Yang C, Zhu X, Liu N et al (2014) Lactoferrin up-regulates intestinal gene expression of brain-derived neurotrophic factors BDNF, UCHL1 and alkaline phosphatase activity to alleviate early weaning diarrhea in postnatal piglets. J Nutr Biochem 25:834–842. https://doi.org/10.1016/j.jnutbio.2014.03.015
Yen M-H, Chiu C-H, Huang Y-C, Lin T-Y (2011) Effects of lactoferrin-containing formula in the prevention of enterovirus and rotavirus infection and impact on serum cytokine levels: a randomized trial. Chang Gung Med J 34:395–402
Yoshioka H, Iseki K, Fujita K (1983) Development and differences of intestinal flora in the neonatal period in breast-fed and bottle-fed infants. Pediatrics 72:317–321
Zhao X, Xu X-X, Liu Y et al (2019) The in vitro protective role of bovine lactoferrin on intestinal epithelial barrier. Molecules 24:E148. https://doi.org/10.3390/molecules24010148
Zimecki M, Spiegel K, Właszczyk A et al (1999) Lactoferrin increases the output of neutrophil precursors and attenuates the spontaneous production of TNF-alpha and IL-6 by peripheral blood cells. Arch Immunol Ther Exp (warsz) 47:113–118
Zou J, Dong J, Yu XF (2009) Meta-analysis: the effect of supplementation with lactoferrin on eradication rates and adverse events during Helicobacter pylori eradication therapy. Helicobacter 14:119–127. https://doi.org/10.1111/j.1523-5378.2009.00666.x
Zuccotti GV, Salvini F, Riva E, Agostoni C (2006) Oral lactoferrin in HIV-1 vertically infected children: an observational follow-up of plasma viral load and immune parameters. J Int Med Res 34:88–94. https://doi.org/10.1177/147323000603400111
Zuccotti GV, Vigano A, Borelli M et al (2007) Modulation of innate and adaptive immunity by lactoferrin in human immunodeficiency virus (HIV)-infected, antiretroviral therapy-naïve children. Int J Antimicrob Agents 29:353–355. https://doi.org/10.1016/j.ijantimicag.2006.11.017
Zuccotti GV, Trabattoni D, Morelli M et al (2009) Immune modulation by lactoferrin and curcumin in children with recurrent respiratory infections. J Biol Regul Homeost Agents 23:119–123
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, HO; investigation, MM; data curation, MM; writing—original draft preparation, MM; writing—review and editing, HO; supervision, MT. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors are employed by Morinaga Milk Industry.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miyakawa, M., Oda, H. & Tanaka, M. Clinical research review: usefulness of bovine lactoferrin in child health. Biometals 36, 473–489 (2023). https://doi.org/10.1007/s10534-022-00430-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10534-022-00430-4