Abstract
This systematic review and meta-analysis study aimed to investigate the effect of sexual counseling based on PLISSIT (Permission, Limited Information, Specific Suggestions, and Intensive Therapy) and EX-PLISSIT models on sexual function, satisfaction, and quality of sexual life. We searched seven electronic databases (MEDLINE, CINAHL, Web of Science, Cochrane Library, ProQuest, Scopus, and PubMed). Studies published between January 1, 2010, and August 16, 2022, were included in the search. Eighteen articles were eligible for inclusion in the analysis. There was a significant difference in the sexual function scores of the PLISSIT and EX-PLISSIT groups and the comparison groups (standardized mean difference (SMD): 1.677; 95% CI 0.668, 2.686; p < 0.05) and “sexual and communication satisfaction” sub-dimension of sexual life quality (SMD: 0.748; 95% CI 0.022, 1.475; p < 0.05). There was no difference in the sexual satisfaction (SMD: 0.425; 95% CI − 0.335, 1.184; p > 0.05) and quality of sexual life scores of the PLISSIT and EX-PLISSIT groups and the comparison groups (SMD: − 0.09; 95% CI − 0.211, 0.032; p > 0.05). PLISSIT and EX-PLISSIT models-based sexual counseling on sexual function was affected by the moderator variables of the time of evaluation of the results after the intervention, type of comparison group, the study population, and by whom the intervention was applied. Sexual counseling based on the PLISSIT and EX-PLISSIT models improved sexual function scores and “sexual and communication satisfaction” sub-dimension of sexual life quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sexuality is one of the basic human needs (East & Hutchinson, 2013). Sexual function is an important part of health and one of the factors affecting the quality of life (Panahi et al., 2021). Sexual quality of life, on the other hand, refers to a general state of well-being in sexual function and satisfaction with sexual function (Mohammadi et al., 2022). In recent years, models are commonly used in sexual health assessment and counseling. It is stated that the use of models is effective in improving the sexual functions of individuals, increasing their sexual satisfaction and sexual life quality (Ziaei et al., 2022). One of these models is the PLISSIT (Permission, Limited Information, Specific Suggestions, and Intensive Therapy) and EXTENDED PLISSIT (EX-PLISSIT) models (Taylor & Davis, 2007). The PLISSIT model was first developed by Annon (1976). The model includes four levels (Permission—Limited Information—Specific Suggestions—Intensive Therapy) of intervention. Each level suggests approaches for responding to sexual concerns. The first level in meeting the sexual health needs of the individual is the evaluation process. In the second level, where information is given about the effect of the disease on sexuality and how treatment can affect sexual functions, it is emphasized that informing patients about their treatments on sexual health has an important place among nursing interventions. The third level includes special suggestions and information for the individual/partner in order to make sexual life more satisfying. The fourth level involves intensive therapy and requires referral to a specialist in sexual rehabilitation.
The PLISSIT model is a standard model and one of the most commonly used. One of the limitations of this model is its linearity and proceeding from one level to the next in which the therapist cannot diagnose the necessity of returning to the previous level to resolve the patient’s sexual concerns. Additionally, it does not include reflection and review elements. Thus, Taylor and Davis (2007) developed the EX-PLISSIT model as an extension of the PLISSIT model. EX-PLISSIT consulting model is based on the key concepts of the PLISSIT model. The main difference is that the allowing step is at the center of the other steps. As in the PLISSIT model, each step is intertwined with each other, not in sequence. In this way, it enables the individual to reveal his/her feelings and thoughts about sexuality. Counseling and intervention in the PLISSIT model, it is possible to move from one level to the other linearly, while in the EX-PLISSIT model, they are cyclical, the permission level is at the center of the other levels. Although the EX-PLISSIT model is based on the main concepts of the PLISSIT model, feedback is essential to increase self-awareness in the EX-PLISSIT model. In the EX-PLISSIT model, after seeking feedback from the client and reviewing outcomes, the therapist will be better off in challenging his or her own assumptions.
The PLISSIT and EX-PLISSIT models are used to evaluate and improve sexual health in patients with breast cancer (Keshavarz et al., 2021; Khoei et al., 2022), multiple sclerosis (Khakbazan et al., 2016), gynecological cancer (Nho, 2013), type 2 diabetes mellitus (Rutte et al., 2015), HIV positive (Asadi et al., 2018), and stoma (Ayaz, 2009). In addition, it is actively used in different processes of women's life such as pregnancy (Nejati et al., 2020) and the postpartum period (Sahin & Sentürk Erenel, 2019).
There are systematic review and meta-analysis studies on the effectiveness of the PLISSIT model in the literature (Kharaghani et al., 2020; Mashhadi et al., 2022; Tuncer & Oskay, 2022). A systematic review found that the PLISSIT model on sexual counseling was an effective, simple, useful, and cost-effective counseling method. The meta-analysis study showed that psychological interventions including the PLISSIT model improved the sexual function of women significantly (Kharaghani et al., 2020). In the other meta-analysis study, it was determined that sexual counseling based on the PLISSIT and EX-PLISSIT models was effective in sexual dysfunction (Mashhadi et al., 2022). Although there are these meta-analysis studies in the literature evaluating the effect of the PLISSIT and EX-PLISSIT models on sexual function, there are no studies in the literature examining the effect of PLISSIT and EX-PLISSIT models on sexual satisfaction and quality of sexual life. For this reason, this systematic review and meta-analysis study aimed to investigate the effect of sexual counseling based on the PLISSIT and EX-PLISSIT models on sexual function, level of satisfaction, and quality of sexual life.
Method
Design
It followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Moher et al., 2015). The protocol of the study was recorded in the "PROSPERO" database, which allows systematic review and meta-analysis studies to be recorded (ID: CRD42021240114).
Search Method
We searched seven electronic databases (MEDLINE, CINAHL, Web of Science, Cochrane Library, ProQuest, Scopus, and PubMed). Studies published between January 1, 2010, and August 16, 2022, were included in the search.
The following MeSH search headings were used: “women OR female" AND plissit OR ex-plissit AND "sexual health" OR sexual OR func* OR "sexual func*” OR dysfunc* OR "sexual dysfunc*" OR "quality of life" OR satisfac* OR "sexual satisfac*" OR "sexual life." These terms and their combinations were searched as text words or abstract/title.
Inclusion Criteria
Types of Studies
We limited the studies to randomized controlled trials. Randomized controlled trials and controlled trials that compared the PLISSIT and EX-PLISSIT model with control groups (e.g., usual care, placebo, no intervention, or waitlist control) or other intervention groups (BETTER model, Sexual Health Model (SHM), and solution-focused group).
Language of Studies
The studies published in English were included in the analysis.
Participants
We applied no restrictions to the participants.
Types of Interventions
We considered the PLISSIT and EX-PLISSIT models-based interventions. We applied no restrictions to the intervention type, dosage, duration, etc.
Types of Outcome Measures
The outcomes measured using validated scales were sexual function (Female Sexual Function Index [FSFI], Brief Index of Sexual Functioning for Women [BISF-W], and Sexual Dysfunctional Beliefs Questionnaire), sexual satisfaction (Hudson's Index of Sexual Satisfaction [ISI] and Berg’s Sexual Satisfaction Questionnaire), and quality of sexual life (Sexual Quality Life-Female [SQOL-F]). We imposed no restrictions for the time measuring health outcomes after the intervention (follow-up period).
Exclusion Criteria
-
1.
Reviews, book chapters, editorials, pilot, commentary and protocols, case repots, quasi-experimental, and duplicate articles.
-
2.
Studies whose full text cannot be reached
-
3.
Studies in languages other than English
Search Outcomes
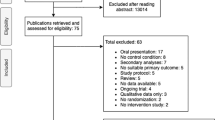
We initially identified 224 records. The results were saved to a citation manager in EndNote X8-2. Then, 115 duplicated articles were identified and excluded. After removing duplicates, we excluded 86 records by reviewing titles and abstracts. The full texts of the remaining 23 records were retrieved and screened for eligibility. We excluded four articles; there were unwanted outcomes (n = 2), and they were not in English (n = 2). As a result, 19 articles were eligible for inclusion in the systematic review and 18 articles in the meta-analysis. Figure 1 presents the flowchart of this systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., 2021). The process of study selection is illustrated in Fig. 1.
Study Selection
Firstly, we imported the documents retrieved from seven databases into EndNote to check for duplicates. Then, the initial screening was performed by two reviewers (SCO and ADG) who independently screened the titles and abstracts of potentially relevant studies. The full texts of the studies that met the inclusion criteria were retrieved and evaluated independently for inclusion in the analysis by the two reviewers (SCO and ADG). The two researchers (SCO and ADG) read the full texts of the studies and determined whether they should be included in the analysis. If they had any disagreement during the study selection process, they tried to resolve it by trying to reach consensus. When consensus could not be reached, a third researcher (ASE) independently reviewed the full text of the study, and three researchers discussed whether it should be included in the analysis.
Assessment of Study Quality
Two reviewers (SCO and ADG) independently assessed the study eligibility. The quality of the included studies was assessed using the RoB 2: A revised Cochrane risk of bias tool for randomized trials (Higgins et al., 2011). Before assessment, the researchers learned how to use the tool which includes seven items: (1) randomization process; (2) deviations from intended interventions; (3) missing outcome data; (4) measurement of the outcome; (5) selection of the reported result; and (6) overall bias. Each item has three options: low risk, high risk, and unclear risk. All assessments of the researchers were integrated into a risk of bias graph and risk of bias summary (Table 1).
Two researchers (SCO and ADG) selected original studies on the basis of the inclusion criteria and reviewed the quality of each. Any disagreement between the two researchers regarding the assessment process was resolved through discussion. The quality assessment process was checked by the third researcher (ASE).
Data Abstraction
Two researchers (SCO and ADG) extracted detailed data on publication information, authors’ name, publication year, publication country, publications’ name, objective, study design, participant characteristics (sample size, diagnosis, and age), intervention details, comparators, tools, outcomes, and results of each study using a structured data extraction form, which was confirmed by the third researcher (ASE).
Data Synthesis and Analysis
All statistical analyses were performed using the Comprehensive Meta-Analysis software 3.0. All randomized studies with sufficient data to calculate the standardized mean difference were included in the meta-analyses (Higgins et al., 2022). One of the studies included in the analysis reported only median and min–max values (Dangesaraki et al., 2019). Therefore, it was not included in the meta-analysis.
Results are presented as standardized mean difference (SMD) with 95% confidence interval (CI) for continuous variables. Cochran’s Q test, I2, and Tau-squared (τ2) were performed to examine the heterogeneity. Heterogeneity was present when the Cochran’s Q test was statistically significant, and the I2 statistic was > 50% (Borenstein et al., 2011). Another indicator of heterogeneity is the Tau-squared (τ2) statistic; if the value of this test is zero, it means there is no heterogeneity (Quintana, 2015).
A random effects model was used in case of heterogeneity. We weighted the studies included in meta-analyses using the inverse-variance method. A two-sided p value of < 0.05 was used to indicate statistical significance. A subgroup analysis was carried out on factors that were thought to affect the homogeneity of the study. Subgroup analyses with mixed-effects models were applied to examine the potential categorical moderators for the PLISSIT or EX-PLISSIT models effects (Borenstein et al., 2011). Publication bias was assessed for the outcomes sexual function and sexual satisfaction. The funnel plot, Begg and Mazumdar’s rank correlation test, and Egger’s regression asymmetry test were used to evaluate the publication bias. There was evidence of publication bias when the results from both tests were statistically significant (Borenstein et al., 2011).
Results
Search Results
A total of 224 studies written in English were retrieved from all databases. Then, 115 duplicate articles were excluded. The remaining 109 articles were reviewed by title and abstract, and 86 studies that did not meet the inclusion criteria were excluded. The full texts of 23 articles were evaluated for relevance. A total of four articles whose language was not English, whose measurement outcomes were not appropriate (Fig. 1). The risk of bias of 19 articles meeting the eligibility criteria was evaluated, and they were included in the review. However, since one of these studies (Dangesaraki et al., 2019) did not report mean and SD values, it was excluded from the analysis, and 18 studies were included in the meta-analysis.
Study Characteristics
A total of 1501 women with a mean age ranging from 18 to 60 years had participated in the 19 randomized controlled trials included in the study. One of the women constituting the sample of the evaluated studies was HIV positive, three had MS, two were post-hysterectomy, one had cyclic mastalgia, three were puerperal, one was with diabetes mellitus, two had sexual problems, three were pregnant, one high body mass index, one was gynecologic cancer, and one had spinal cord injury. Eighteen of the studies were carried out in Iran, and one was conducted in Turkey (Table 2).
The duration of the counseling session based on the PLISSIT and EX-PLISSIT was different. The number of the counseling sessions varied from 1 to 5, and the duration of each session varied from 30 to 120 min. In all studies, the comparison group was the control group, the group received routine care. The other comparison groups were the solution-focused group counseling, BETTER model, and the SHM.
The practitioners of sexual counseling based on the PLISSIT and EX-PLISSIT models had different occupations such as trained midwives (Dangesaraki et al., 2019; Khakbazan et al., 2016; Mehrabi et al., 2019; Moghaddam et al., 2019; Nejati et al., 2020), research team members (Asadi et al., 2020; Farnam et al., 2014; Kargar et al., 2021; Malakouti et al., 2020; Mohammadi et al., 2022; Rezaei-Fard et al., 2019; Tutuncu and Yilmaz, 2012), a counselor (Azari-Barzandig et al., 2020), and a trained student of reproductive health under the supervision of a sex therapist or tutor (Ghodsi et al., 2021; Ziaei et al., 2022).
Ten studies used the FSFI to evaluate sexual function (Asadi et al., 2018; Dangesaraki et al., 2019; Karimi et al., 2021; Khakbazan et al., 2016; Malakouti et al., 2020; Mehrabi et al., 2019; Mohammadi et al., 2022; Rezaei-Fard et al., 2019; Shahbazi et al., 2019; Tutuncu & Yıldız, 2012), and one study used the Brief Index of Sexual Functioning for Women (BISF-W) (Farnam et al., 2014). The measurement times differed in these studies. In some studies, the FSFI was administered 1 month after the intervention (Asadi et al., 2018; Karimi et al., 2021; Malakouti et al., 2020; Mehrabi et al., 2019; Rezaei-Fard et al., 2019; Shahbazi et al., 2019), while in some others, it was administered 2 months after the intervention (Khakbazan et al., 2016; Malakouti et al., 2020; Mehrabi et al., 2019; Mohammadi et al., 2022; Rezaei-Fard et al., 2019). It was administered 3 months after the intervention in three studies (Asadi et al., 2018; Khakbazan et al., 2016; Tutuncu & Yıldız, 2012). In one study, sexual function was evaluated by administering the FSFI 6 months after the intervention (Tutuncu & Yıldız, 2012), and again only one study used the Sexual Dysfunctional Beliefs Questionnaire (Moghaddam et al., 2019). And also in one study, sexual function was evaluated by administering the BISF-W 7 months after the intervention (Farnam et al., 2014).
In five studies, sexual satisfaction was evaluated using the ISS (Banei et al., 2016; Ghodsi et al., 2021; Kargar et al., 2021; Moghaddam et al., 2019; Ziaei et al., 2022). One study used Linda Berg's Sexual Satisfaction Questionnaire to assess sexual satisfaction (Nejati et al., 2020). In almost all studies, sexual satisfaction was evaluated 1 month after the intervention (Banei et al., 2016; Ghodsi et al., 2021; Kargar et al., 2021; Moghaddam et al., 2019; Nejati et al., 2020; Ziaei et al., 2022). One study evaluated sexual satisfaction 2 weeks after the intervention (Nejati et al., 2020), and two studies evaluated it 3 months after the intervention (Banei et al., 2016; Ghodsi et al., 2021).
Sexual quality of life was evaluated in four studies. The SQOL-F was used as a measurement tool for this purpose (Azari-Barzandig et al., 2020; Dangesaraki et al., 2019; Kazemi et al., 2021; Mohammadi et al., 2022). In these studies, sexual quality of life was reevaluated 2 months after the intervention. It was evaluated 2 weeks after the intervention in only one study (Kazemi et al., 2021).
Risk of Bias
The bias assessment of nineteen RCT studies using the Cochrane risk of bias ROB 2.0 instrument showed that six studies were at high risk, and thirteen studies were at some concerns. These studies lacked detailed randomization methods and allocation concealment. And also data collection was based on self-report questionnaires, the participants or practitioners could not be blinded and no “intention-to-treat estimates.” Table 1 shows for the details summarizing the risk of bias assessment for the included studies.
Effectiveness of the PLISSIT and EX-PLISSIT Models
Sexual Function
Outcome data 1, 2, 3, 6, or 7 months after the intervention were available in nine trials (1121 women). Random effects was selected, because the ten studies were heterogeneous (Tau2 = 2.120, Q2 = 418.2795, df = 9 (p < .001), I2 = 97.848%). The forest plot in Fig. 2 illustrates that there was a significant difference in the sexual function scores of the PLISSIT and EX-PLISSIT groups and the comparison group (SMD: 1.677; 95% CI 0.668, 2.686; p < 0.05).
Sexual Satisfaction
Outcome data were available for six trials (673 women). Random effects was selected because these six studies were heterogeneous (Tau2 = 0.847, Q2 = 102.123, df = 5 (p < .001), I2 = 95.104%). The forest plot in Fig. 3 illustrates that there was not significant difference in the sexual satisfaction scores of the PLISSIT and EX-PLISSIT groups and the comparison group (SMD: 0.425; 95% CI − 0.335, 1.184; p > 0.05).
Quality of Sexual Life
Outcome data were available for three trials (1164 women). Random effects was selected because these three studies were heterogeneous (Tau2 = 0.584, Q2 = 123.725, df = 11 (p < .001), I2 = 91.109%). The forest plot in Fig. 4 illustrates that there was no difference in the quality of sexual life scores of the PLISSIT and EX-PLISSIT groups and the comparison group (SMD: − 0.666; 95% CI − 0.520, 0.389; p > 0.05). SQOL-F scale sub-dimension scores of the groups were examined. No difference was found between the PLISSIT and EX-PLISSIT groups and the comparison group in terms of the mean “feeling of worthlessness” (SMD: − 0.172; CI − 0.877, 0.532; p > 0.05), “psycho-sexual feelings” (SMD: -0.522, CI − 1.796, 0.751; p > 0.05), and “suppression of sexual expression” (SMD: − 0.349, CI − 1.411, 0.712; p > 0.05) sub-dimension scores of the SQOL. However, a significant difference was observed between the PLISSIT and EX-PLISSIT groups and the comparison group in terms of the mean “sexual and communication satisfaction” sub-dimension score (SMD: 0.748; 95% CI 0.022, 1.475; p < 0.05).
Subgroup Analysis
Two months (5.588) and 3 months (4.170) after intervention had a greater effect in improving sexual function than those with other measurement times (effect size: 2.489; 95% CI 1.256, 3.721; p < 0.05). In studies with a control group, the effect of the PLISSIT and EX-PLISSIT models on sexual function is higher than other studies (BETTER and SHM groups) (effect size: 1.514; 95% CI 0.614, 2.414; p < 0.05). The effect of PLISSIT and EX-PLISSIT models on sexual function of women with diseases (2.792) and with hysterectomy (1.432) was more than in women with pregnant or postpartum (0.899), with cancer (0.127), and with sexual problems (effect size: 1.539; 95% CI 0.327, 2.751; p < 0.05). The intervention is performed by a trained midwife (4.699) which had a greater effect in improving sexual function than by a research team members (0.824) (effect size: 1.770; 95% CI 0.685, 2.854; p < 0.05) (Table 3).
Three months of after intervention (2.042) had a greater effect in improving sexual satisfaction than those with 1 and 2 months (1.004, 95% CI 0.685, 1.323, p < 0.05). There was not significant overall effect of PLISSIT and EX-PLISSIT models on sexual satisfaction by the comparison group, study population, and by whom intervention (p > 0.05) (Table 3).
Publication Bias
Based on the results obtained using the funnel plot of standard error by SMD for the outcomes sexual function and sexual satisfaction, it was not possible to conclude that there was a likelihood of publication bias (Figs. 5 and 6). Because the Begg and Mazumdar rank correlation test (p = 0.465) and the Egger’s regression test (p = 0.138) were not significant for the outcomes sexual function. Likewise, the Begg and Mazumdar rank correlation test (p = 0.916) and the Egger’s regression test (p = 0.408) were not significant for the outcomes sexual satisfaction.
Discussion
Our meta-analysis revealed that individual sexual counseling based on the PLISSIT and EX-PLISSIT models applied in different populations improves sexual. And also, there was a positive and significant improvement only in the “sexual and communication satisfaction” sub-dimension of sexual life quality.
Sexuality is affected by many physiological, cultural, social, and psychological factors (McCool-Myers et al., 2018). This effect is more pronounced in pathologies that are directly related to reproduction rates, and in medical conditions such as multiple sclerosis and spinal cord injury that affect the muscle and neurological system (Azimi et al., 2019; Courtois et al., 2017). In addition, it is known that chronic diseases and periods such as pregnancy, postpartum period, and menopause, where biological and hormonal changes are experienced, directly affect sexual life negatively (Sentürk Erenel et al., 2015; Gutzeit et al., 2020; Rahmanian et al., 2019). The women in our study had different characteristics (HIV positive, MS, women with hysterectomy, pregnant women, postpartum women, cancer, with diabetes mellitus, women with sexual problems, high body mass index, and spinal cord injury). The study revealed that individual sexual counseling based on the PLISSIT and EX-PLISSIT models had a positive effect on sexual function. Similar to our results, two systematic review studies which examined the effectiveness of sexual counseling based on the PLISSIT model reported that the use of a model was effective in improving sexual functions (Kırıcı & Ege, 2021; Tuncer & Oskay, 2022). One meta-analysis study which investigated the effect of sexual counseling based on the PLISSIT model on sexual dysfunction in both women and men reported that counseling positively affects sexual function (Mashhadi et al., 2022).
Our meta-analysis showed that individual sexual counseling based on the PLISSIT and EX-PLISSIT models had a positive effect on the sub-dimension of sexual and communication satisfaction in the SQOL scale. It is known that with the increase in sexual function, the harmony between the couples increases and the general quality of life is positively affected (Jones et al., 2018; Mallory et al., 2019). In this context, our meta-analysis findings support the literature. However, no significant effect was observed in this study in the other sub-dimensions of the SQOL scale (feeling of worthlessness, psychosexual feelings, and suppression of sexual expression). This may be related to the multidimensional and complex nature of sexuality.
According to the subgroup analysis, it was determined that the effectiveness of sexual counseling based on PLISSIT and EX-PLISSIT model on sexual function and satisfaction was high in the 2nd and 3rd months. However, the effect of PLISSIT and EX-PLISSIT model on sexual function decreased in the 6th and 7th months. This shows that the effectiveness of the counseling based on the PLISSIT and EX-PLISSIT models decreased in the following periods. It is important to evaluate the effects of sexual counseling at certain periods and to repeat the intervention when necessary (Kharaghani et al., 2020).
In studies with a control group, the effect of the PLISSIT and EX-PLISSIT models on sexual function is higher than other studies (BETTER and SHM groups). This may have resulted from the fact that the individuals participating in the control group studies did not receive any intervention and received routine care.
There was no standardized model-based counseling in the reviewed studies, and counseling was carried out by different practitioners with different populations. According to the subgroup analysis, the effectiveness of sexual counseling based on PLISSIT and EX-PLISSIT model on sexual function is higher in women with diseases (MS, HIV, SCI, diabetes mellitus, CM, and obesity) and post-hysterectomy, than in women with sexual problems and pregnant or postpartum women. Sexual interest and desire decrease due to physical and physiological changes during pregnancy and postpartum. The frequency of sexual intercourse during pregnancy decreases due to cultural practices, lack of awareness that sexual intercourse during pregnancy is not contraindicated unless recommended by an obstetrician, belief that it may cause miscarriage, stillbirth and fetal infections, lack of appropriate counseling by health-care providers about safe sexual practices during pregnancy, and lack of communication between spouses about their sexual expectations and needs during pregnancy (Fernández-Carrasco et al., 2020; Thapa et al., 2023). During the puerperium, sexual interest and desire decreases due to body changes, pain, fatigue, anxiety, and role changes (Drozdowskyj et al., 2020). It is thought that the reason why the effectiveness of the models is less effective in women during pregnancy and puerperium is due to the decrease in sexual interest and desire in women during these processes and the focus being on the baby.
Furthermore, according to subgroup analysis, we identified that the trained midwifery by sexual counseling based on PLISSIT and EX-PLISSIT models was an important moderator on increasing sexual function. This may be due to the longer duration of counseling provided by trained midwives. In addition, midwives, like nurses, are the main care providers who first contact with the patient and are perceived as more reliable by patients (Demir et al., 2020). These situations may have affected the high effectiveness of midwife-led interventions.
Studies in this meta-analysis were rated to have “some concerns” or “a high risk of bias.” The reviewed studies did not include blinding, and the data were collected using self-report questionnaires, which increased the risk of bias. In addition, "allocation concealment" was not ensured during the allocation process, and no appropriate analyses were used in the evaluation of the missing data, which increased the risk of bias in the reviewed studies. Therefore, it is recommended to evaluate the results of this meta-analysis considering the risk of bias findings. Experimental studies with low risk of bias are needed to clearly demonstrate the effect of individual counseling based on the PLISSIT and EX-PLISSIT models on sexual health parameters.
Conclusion and Recommendations
This meta-analysis showed that sexual counseling based on the PLISSIT and EX-PLISSIT models provided significant improvements in sexual function and “sexual and communication satisfaction” sub-dimension of sexual life quality. According to the subgroup analysis, it was determined that PLISSIT and EX-PLISSIT models-based sexual counseling on sexual function was affected by the moderator variables of the time of evaluation of the results after the intervention, type of comparison group, the study population, and by whom the intervention was applied. In addition, there is a need for more methodologically strong experimental studies in this area in order to explain the current effect more clearly.
References
Annon, J. S. (1976). The PLISSIT model: A proposed conceptual scheme for the behavioral treatment of sexual problems. Journal of Sex Education and Therapy, 2(1), 1–15. https://doi.org/10.1080/01614576.1976.11074483
Asadi, L., Ziaei, T., Koochak, H. E., Montazeri, A., Rezaei, E., Moghadam, Z. B., & Shahmohammadi, L. (2018). Effect of counseling based on PLISSIT model on sexual function of HIV-positive married women. HIV & AIDS Review International Journal of HIV-Related Problems, 17(3), 169–175.
Ayaz, S., & Kubilay, G. (2009). Effectiveness of the PLISSIT model for solving the sexual problems of patients with stoma. Journal of Clinical Nursing, 18(1), 89–98.
Azari-Barzandig, R., Sattarzadeh-Jahdi, N., Nourizadeh, R., Malakouti, J., Mousavi, S., & Dokhtvasi, G. (2020). The effect of counseling based on EX-PLISSIT model on sexual dysfunction and quality of sexual life of married women with multiple sclerosis: A randomized controlled clinical trial. Sexuality and Disability, 38(2), 271–284.
Azimi, A., Hanaei, S., Sahraian, M. A., Mohammadifar, M., Ramagopalan, S. V., & Ghajarzadeh, M. (2019). Prevalence of sexual dysfunction in women with multiple sclerosis: A systematic review and meta-analysis. Maedica, 14(4), 408–412. https://doi.org/10.26574/maedica.2019.14.4.408
Banaei, M., Zahrani, S. T., Pormehr-Yabandeh, A., Ozgoli, G., & Azad, M. (2016). Investigating the impact of counseling based on PLISSIT model on sexual intimacy and satisfaction of breastfeeding women. International Journal of Pharmaceutical Research and Allied Sciences, 5(3), 489–499.
Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2011). Introduction to meta-analysis. John Wiley & Sons Ltd.
Courtois, F., Alexander, M., & McLain, A. B. (2017). Women’s sexual health and reproductive function after SCI. Topics in Spinal Cord Injury Rehabilitation, 23(1), 20–30. https://doi.org/10.1310/sci2301-20
Dangesaraki, M. M., Maasoumi, R., Hamzehgardeshi, Z., & Kharaghani, R. (2019). Effect of the EX-PLISSIT model on sexual function and sexual quality of life among women after hysterectomy: A randomised controlled trial. Sexual Health, 16(3), 225–232.
Demir, R., Çakaloz, D. K., Taşpinar, A., & Çoban, A. (2020). Ebelik öğrencilerinin hasta güvenliği konusundaki düşünceleri ve tıbbi hata yapma eğilimleri. Celal Bayar Üniversitesi Sağlık Bilimleri Enstitüsü Dergisi, 7(2), 148–156.
Drozdowskyj, E. S., Castro, E. G., Lopez, E. T., Taland, I. B., & Actis, C. C. (2020). Factors influencing couples’ sexuality in the puerperium: A systematic review. Sexual Medicine Review, 8(1), 38–47.
East, L., & Hutchinson, M. (2013). Moving beyond the therapeutic relationship: A selective review of intimacy in the sexual health encounter in nursing practice. Journal of Clinical Nursing, 22(23–24), 3568–3576.
Farnam, F., Janghorbani, M., Raisi, F., & Merghati-Khoei, E. (2014). Compare the effectiveness of PLISSIT and sexual health models on women’s sexual problems in Tehran, Iran: A randomized controlled trial. Journal of Sexual Medicine, 11(11), 2679–2689.
Fernández-Carrasco, F. J., Rodríguez-Díaz, L., González-Mey, U., Vázquez-Lara, J. M., Gómez-Salgado, J., & Parrón-Carreño, T. (2020). Changes in sexual desire in women and their partners during pregnancy. Journal of Clinical Medicine, 9(2), 526. https://doi.org/10.3390/jcm9020526
Ghodsi, F., Bahrami, N., Mafi, M., & Olfati, F. (2021). The effect of sex counseling based on (permission, limited information, specific suggestions, intensive therapy) model on sexual satisfaction in women with cyclic mastalgia: A randomized controlled clinical trial. Iranian Journal of Nursing and Midwifery Research, 26(6), 562–568.
Gutzeit, O., Levy, G., & Lowenstein, L. (2020). Postpartum female sexual function: Risk factors for postpartum sexual dysfunction. Sexual Medicine, 8(1), 8–13. https://doi.org/10.1016/j.esxm.2019.10.005
Higgins, J.P.T., Li, T., Deeks, J.J. (2022). Choosing effect measures and computing estimates of effect. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, & V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane, 2022. Retrieved from www.training.cochrane.org/handbook.
Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a metaanalysis. Statistics in Medicine, 21(11), 1539–1558.
Jones, A. C., Robinson, W. D., & Seedall, R. B. (2018). The role of sexual communication in couples’ sexual outcomes: A dyadic path analysis. Journal of Marital and Family Therapy, 44(4), 606–623. https://doi.org/10.1111/jmft.12282
Kargar, M., Yousefzadeh, S., Behnam, H. R., & Vaghee, S. (2021). Comparing the effect of solution-focused group counseling and individual counseling based on PLISSIT model on sexual satisfaction of women with high body mass index. Journal of Midwifery & Reproductive Health, 9(2), 2697–2706.
Karimi, F., Babazadeh, R., Roudsari, R. L., Asgharipour, N., & Esmaily, H. (2021). Comparing the effectiveness of sexual counseling based on PLISSITand BETTER models on sexual selfdisclosure in women with sexual problems after childbirth: A randomized trial. Iranian Journal of Nursing and Midwifery Research, 26(1), 68–74.
Kazemi, Z., Mousavi, M. S., & Etemadifar, M. (2021). The effect of counseling based on the PLISSIT model on sexual quality of life of married women with multiple sclerosis referring to MS center in 2019: A randomized, controlled trial. Archives of Women’s Mental Health, 24(3), 437–444.
Keshavarz, Z., Karimi, E., Golezar, S., Ozgoli, G., & Nasiri, M. (2021). The effect of PLISSIT based counseling model on sexual function, quality of life, and sexual distress in women surviving breast cancer: A single-group pretest–posttest trial. BMC Women’s Health, 21(1), 417. https://doi.org/10.1186/s12905-021-01570-4
Khakbazan, Z., Daneshfar, F., Behboodi-Moghadam, Z., Nabavi, S. M., Ghasemzadeh, S., & Mehran, A. (2016). The effectiveness of the permission, limited information, specific suggestions, intensive therapy (PLISSIT) model based sexual counseling on the sexual function of women with multiple sclerosis who are sexually active. Multiple Sclerosis and Related Disorders, 8, 113–119.
Kharaghani, R., Khani, M. E., Dangesaraki, M. M., & Damghanian, M. (2020). The effects of psychological interventions on sexual function of women: A systematic review and meta-analysis. Nursing Practice Today, 7(3), 169–182.
Khoei, E. M., Kharaghani, R., Shakibazadeh, E., Faghihzadeh, S., Aghajani, N., Korte, J. E., & Esmkhani, M. (2022). Sexual health outcomes of PLISSIT-based counseling versus grouped sexuality education among Iranian women with breast cancer: A randomized clinical trial. Sexual and Relationship Therapy, 37(4), 557–568.
Kırıcı, S., & Ege, E. (2021). The effect of the PLISSIT Model on sexual functions: A systematic review. BANÜ Sağlık Bilimleri Ve Araştırmaları Dergisi, 3(3), 199–207. https://doi.org/10.46413/boneyusbad.943252
Malakouti, J., Golizadeh, R., Mirghafourvand, M., & Farshbaf-Khalili, A. (2020). The effect of counseling based on ex-PLISSIT model on sexual function and marital satisfaction of postpartum women: A randomized controlled clinical trial. Journal of Education and Health Promotion, 9, 2841–3287.
Mallory, A. B., Stanton, A. M., & Handy, A. B. (2019). Couples’ sexual communication and dimensions of sexual function: A meta-analysis. Journal of Sex Research, 56(7), 882–898. https://doi.org/10.1080/00224499.2019.1568375
Mashhadi, Z. N., Irani, M., Ghorbani, M., Ghazanfarpour, M., Nayyeri, S., & Ghodrati, A. (2022). The effects of counselling based on PLISSIT Model on sexual dysfunction: A systematic review and meta-analysis. Research in Health & Medical Sciences, 1(2), 16–29.
McCool-Myers, M., Theurich, M., Zuelke, A., Knuettel, H., & Apfelbacher, C. (2018). Predictors of female sexual dysfunction: A systematic review and qualitative analysis through gender inequality paradigms. BMC Women’s Health, 18(1), 108. https://doi.org/10.1186/s12905-018-0602-4
Mehrabi, M., Lotfi, R., Rahimzadeh, M., & Merghati Khoei, E. (2019). Effectiveness of sexual counseling using PLISSIT model on sexual function of women with type 2 diabetes mellitus: Results from a randomized controlled trial. International Journal of Diabetes in Developing Countries, 39(4), 626–632.
Moghaddam, M. M., Moradi, M., Mirzaii Najmabadi, K., Ramezani, M. A., & Shakeri, M. T. (2019). Effect of counseling on the sexual satisfaction level of women with sexual dysfunction using PLISSIT model focused on dysfunctional sexual beliefs. Evidence Based Care, 9(3), 49–57.
Mohammadi, Z., Maasoumi, R., Vosoughi, N., Eftekhar, T., Soleimani, M., & Montazeri, A. (2022). The effect of the EX-PLISSIT model-based psychosexual counseling on improving sexual function and sexual quality of life in gynecologic cancer survivors: A randomized controlled clinical trial. Supportive Care in Cancer, 30(11), 9117–9126.
Mohammadi, Z., Maasoumi, R., Vosoughi, N., Eftekhar, T., Soleimani, M., & Montazeri, A. (2022). The effect of the EX-PLISSIT model-based psychosexual counseling on improving sexual function and sexual quality of life in gynecologic cancer survivors: A randomized controlled clinical trial. Supportive Care in Cancer, 30, 9117–9126.
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., & Stewart, L. A. (2015). Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1. https://doi.org/10.1186/2046-4053-4-1
Nejati, B., Masoumi, S., Parsa, P., Karami, M., & Mortazavi, A. (2020). Effect of counselling based on the PLISSIT model on pregnant women’s sexual satisfaction: A randomised controlled trial. Family Medicine & Primary Care Review, 22(1), 43–48.
Nho, J. H. (2013). Effect of PLISSIT model sexual health enhancement program for women with gynecologic cancer and their husbands. Journal of Korean Academy of Nursing, 43(5), 681–689.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., & Chou, R. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. British Medical Journal, 372. https://doi.org/10.1136/bmj.n71
Panahi, R., Anbari, M., Javanmardi, E., Ghoozlu, K. J., & Dehghankar, L. (2021). The effect of women’s sexual functioning on quality of their sexual life. Journal of Preventive Medicine and Hygiene, 62(3), 776–781.
Quintana, D. S. (2015). From pre-registration to publication: A nontechnical primer for conducting a meta-analysis to synthesize correlational data. Frontiers in Psychology, 6, 1549. https://doi.org/10.3389/fpsyg.2015.01549
Rahmanian, E., Salari, N., Mohammadi, M., & Jalali, R. (2019). Evaluation of sexual dysfunction and female sexual dysfunction indicators in women with type 2 diabetes: A systematic review and meta-analysis. Diabetology & Metabolic Syndrome, 11, 73. https://doi.org/10.1186/s13098-019-0469-z
Rezaei-Fard, M., Lotfi, R., Rahimzadeh, M., & Merghati-Khoei, E. (2019). Effectiveness of sexual counseling using PLISSIT model to promote sexual function of women with spinal cord injury: A randomized controlled trial. Sexuality and Disability, 37(4), 511–519.
Rutte, A., van Oppen, P., Nijpels, G., Snoek, F. J., Enzlin, P., Leusink, P., & Elders, P. J. (2015). Effectiveness of a PLISSIT model intervention in patients with type 2 diabetes mellitus in primary care: Design of a cluster-randomised controlled trial. BMC Family Practice, 16(1), 69. https://doi.org/10.1186/s12875-015-0283-0
Sahin, E., & Erenel, A. S. (2019). A study examining women’s sexual function in twelve months postpartum. Medicine, 8(1), 148–153.
Senturk Erenel, A., Golbasi, Z., Kavlak, T., & Dilbaz, S. (2015). Relationship between menopausal symptoms and sexual dysfunction among married Turkish women in 40–65 age group. International Journal of Nursing Practice, 21(5), 575–583.
Shahbazi, Z., Farshbaf-Khalili, A., Sattarzadeh, N., & Kamalifard, M. (2019). The effect of sexual counseling based on PLISSIT model on sexual function of pregnant women: A randomized controlled clinical trial. International Journal of Women’s Health and Reproduction Science, 7(3), 372–379.
Taylor, B., & Davis, S. (2007). The extended PLISSIT model for addressing the sexual wellbeing of individuals with an acquired disability or chronic illness. Sexuality and Disability, 25, 135–139. https://doi.org/10.1007/s11195-007-9044-x
Thapa, B., Pradhan, S. M., Maharjan, M., Pandey, A., Sen, K., Karki, S., Pudasaini, P., & Tiwari, A. (2023). Sexual intercourse during pregnancy among postpartum women admitted to the Department of Obstetrics in a tertiary care centre. JNMA Journal of the Nepal Medical Association, 61(266), 798–802.
Tuncer, M., & Oskay, Ü. Y. (2022). Sexual counseling with the PLISSIT model: A systematic review. Journal of Sex & Marital Therapy, 48(3), 309–318.
Tutuncu, B., & Yildiz, H. (2012). The influence on women’s sexual functions of education given according to the PLISSIT model after hysterectomy. Procedia-Social and Behavioral Sciences, 47, 2000–2004.
Ziaei, T., Kharaghani, R., Haseli, A., & Ahmadnia, E. (2022). Comparing the effect of extended PLISSIT model and group counseling on sexual function and satisfaction of pregnant women: A randomized clinical trial. Journal of Caring Sciences, 11(1), 7–14.
Acknowledgements
The authors would like to thank all the women who participated in this study.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). No grants or financial support was received from any funding agency in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Contributions
SCO, ADG, and ASE helped in conceptualization; SCO, ADG, and ASE helped in methodology; SCO helped in data analysis; SCO and ADG contributed to writing—original draft preparation; and SCO, ADG, and ASE writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
Ethics committee approval is not required as this study is a systematic review and meta-analysis study.
Consent to Participate
As this was an analysis of the studies that had been published in the past, no consent to participate was necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cicek Ozdemir, S., Dogan Gangal, A. & Senturk Erenel, A. The Effect of Sexual Counseling Based on PLISSIT and EX-PLISSIT Models on Sexual Function, Satisfaction, and Quality of Life: A Systematic Review and Meta-Analysis. Arch Sex Behav (2024). https://doi.org/10.1007/s10508-024-02898-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10508-024-02898-2