Abstract
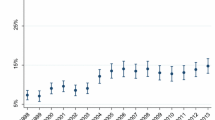
Curable sexually transmitted infections (STIs) affect millions of people across the world. Besides unacceptably high HIV rates, South Africa also has the highest burden of STIs in the world. The aim of the study was to investigate temporal changes in STI incidence rates using the data from ~ 10,000 women who enrolled in several HIV prevention trials, KwaZulu-Natal, South Africa (2002–2016). We particularly focused on the changes in distribution of the most influential factors and their population-level impacts on STI incidence rates over time. Characteristics of the women were compared across the study periods: 2002–2004, 2005–2008, 2009–2011, and 2012–2016. Besides multivariable Cox regression models, population attributable risks were calculated for the significant factors. Despite the significant progress in prevention, testing, and treatment programs, infection rates increased substantially from 13.6 to 20.0 per 100 person-year over the study period. Our findings provided a compelling evidence for single/non-cohabiting South African women to be the most vulnerable population who consistently and substantially contributed to increasing STI rates during the 15 years of study duration (PAR%: 44%–47%). We also highlighted the impact of women’s lack of knowledge related to their partner, using injectable contraceptives, less parity, and baseline STI positivity which were increased substantially over time. Our findings suggest that a significant proportion of STIs could be prevented by targeting single/non-cohabiting. These results may provide guidance in developing more effective STI prevention programs by targeting women at highest risk of infections and delivering more realistic messages.


Similar content being viewed by others
References
Adachi, K., Nielsen-Saines, K., & Klausner, J. D. (2016). Chlamydia trachomatis infection in pregnancy: The global challenge of preventing adverse pregnancy and infant outcomes in Sub-Saharan Africa and Asia. BioMed Research International. https://doi.org/10.1155/2016/9315757.
Baeten, J.M., Palanee-Phillips, T., Brown, E.R., Schwartz, K., SotoTorres, L.E., Govender, V., Mgodi, N.M., Kiweewa, F.M., Nair, G., Mhlanga, F., Siva, S., Bekker, L.G. for the MTN-020-ASPIRE Study Team. (2016). Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. New England Journal of Medicine. https://doi.org/10.1056/NEJMoa1506110.
Brown, J. L., Sales, J. M., DiClemente, R. J., Salazar, L. F., Vanable, P. A., Carey, M. P., Brown, L. K., Romer, D., Valois, R. F., & Stanton, B. (2012). Predicting discordance between self-reports of sexual behavior and incident sexually transmitted infections with African American female adolescents: Results from a 4-city study. AIDS and Behavior, 16(6), 1491–1500.
Census. (2011). Statistical release. Statistics South Africa. 2012 (p. 14) Retrieved from http://www.statssa.gov.za.
Chersich, M. F., & Rees, H. V. (2008). Vulnerability of women in southern Africa to infection with HIV: Biological determinants and priority health sector interventions. AIDS, 22, S27–S40.
DiClemente, R. J., Swartzendruber, A. L., & Brown, J. L. (2013). Improving the validity of self-reported sexual behavior: No easy answers. Sexually Transmitted Diseases, 40, 111–112. https://doi.org/10.1097/OLQ.0b013e3182838474.
Dunkle, K. L., Jewkes, R. K., Brown, H. C., Gray, G. E., McIntryre, J. A., & Harlow, S. D. (2004). Transactional sex among women in Soweto, South Africa: Prevalence, risk factors and association with HIV infection. Social Science and Medicine, 59(1581–1592), 39.
Heffron, R., Parikh, U. M., Penrose, K. J., Mugo, N., Donnell, D., Celum, C., Mellors, J. W., & Baeten, J. (2017). Objective measurement of inaccurate condom use reporting among women using depot medroxyprogesterone acetate for contraception. AIDS and Behavior, 21, 2173–2179. https://doi.org/10.1007/s10461-016-1563-y
Jewkes, R. K., Dunkle, K., Nduna, M., & Shai, N. (2010). Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet, 376, 41–48.
Joint United Nations Program on HIV/AIDS (UNAIDS). (2016). Global AIDS update. Geneva, Switzerland. Retrieved from https://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf
Karim, Q. A., Karim, S. S. A., Frohlich, J. A., Grobler, A. C., Baxter, C., Mansoor, L. E., Kharsany, A. B., Sibeko, S., Mlisana, K. P., Omar, Z., & Gengiah, T. N. (2010). Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science, 329(5996), 1168–1174.
Kharsanya, A. B. M., McKinnona, L. R., Lewisa, L., Cawoodd, C., Khanyiled, D., Masekoe, D. V., & Toledog, C. (2020). Population prevalence of sexually transmitted infections in a high HIV burden district in KwaZulu-Natal, South Africa: Implications for HIV epidemic control. International Journal of Infectious Diseases, 98(2020), 130–137. https://doi.org/10.1016/j.ijid.2020.06.046.
Leah, G. (2016). The mercurial piece of the puzzle: Understanding stigma and HIV/AIDS in South Africa. SAHARA-J. Journal of Social Aspects of HIV/AIDS, 13(1), 8–16.
Lewis, D. A. (2012). Detection and management of acute HIV infections in patients with sexually transmitted infections: A window of opportunity for HIV prevention within South Africa? Southern African Journal of Epidemiology and Infection, 27(4), 149–155.
Luke, N. (2003). Age and economic asymmetries in the sexual relationships of adolescent girls in sub-Saharan Africa. Studies in Family Planning, 34(2), 67–86.
Marrazzo, J. M., Ramjee, G., Richardson, B. A., Gomez, K., Mgodi, N., Nair, G., Palanee, T., Nakabiito, C., Van Der Straten, A., Noguchi, L., & Hendrix, C. W. (2015). Tenofovir-based preexposure prophylaxis for HIV infection among African women. New England Journal of Medicine, 372(6), 509–518.
Mayer, K. H., & de Vries, H. (2018). HIV and sexually transmitted infections: Responding to the “newest normal.” Journal of the International AIDS Society, 21(7), e25164.
Mayer, K. H., & Venkatesh, K. K. (2011). Interactions of HIV, other sexually transmitted diseases, and genital tract inflammation facilitating local pathogen transmission and acquisition. American Journal of Reproductive Immunology, 65, 308–316.
McClelland, R. S., Sangaré, L., Hassan, W. M., Lavreys, L., Mandaliya, K., Kiarie, J., Ndinya-Achola, J., Jaoko, W., & Baeten, J. M. (2007). Infection with Trichomonas vaginalis increases the risk of HIV-1 acquisition. Journal of Infectious Diseases, 195(5), 698–702.
McCormack, S., Ramjee, G., Kamali, A., Rees, H., Crook, A. M., Gafos, M., Jentsch, U., Pool, R., Chisembele, M., Kapiga, S., Mutemwa, R., Vallely, A., Palanee, T., Sookrajh, Y., Lacey, C. J., Darbyshire, J., Grosskurth, H., Profy, A., Nunn, A., & Weber, J. (2010). PRO2000 vaginal gel for prevention of HIV-1 infection (Microbicides Development Programme 301): A phase 3, randomised, double-blind, parallel-group trial. Lancet, 376, 1329–1337.
Microbicide Trials Network (MTN). (2011). MTN statement on decision to discontinue use of Tenofovir gel in VOICE, a major HIV prevention study in women. http://www.mtnstopshiv.org/ node/3909. Accessed 19 December 2019.
Moodley, D., Moodley, P., Sebitloane, M., Deepak, S., McNaughton-Reyes, H. L., Groves, A. K., & Maman, S. (2015). High prevalence and incidence of asymptomatic sexually transmitted infections during pregnancy and postdelivery in KwaZulu Natal, South Africa. Sexually Transmitted Diseases, 42(1), 43–47. https://doi.org/10.1097/OLQ.0000000000000219.
Ott, M. Q., Bärnighausen, T., Tanser, F., Lurie, M. N., & Newell, M. L. (2011). Age-gaps in sexual partnerships: Seeing beyond ‘sugar daddies.’ AIDS, 25, 861–863.
Padian, N. S., van der Straten, A., Ramjee, G., Chipato, T., de Bruyn, G., Blanchard, K., Shiboski, S., Montogomery, E. T., Fancher, H., & Cheng, H. (2007). Diaphragm and lubricant gel for prevention of HIV acquisition in southern African women: A randomised controlled trial. Lancet, 370, 251–261.
Posel, D., & Rogan, M. (2009). Women, income and poverty: Gendered access to resources in post-apartheid South Africa. Agenda, 81, 25–34.
Reynolds, S. J., Risbud, A. R., Shepherd, M. E., Rompalo, A. M., Ghate, M. V., Godbole, S. V., Joshi, S. N., Divekar, A. D., Gangakhedkar, R. R., Bollinger, R. C., & Mehendale, S. M. (2006). High rates of syphilis among STI patients are contributing to the spread of HIV-1 in India. Sexually Transmitted Infections, 82(2), 121–126.
Rowley, J., Vander Hoorn, S., Korenromp, E., Low, N., Unemo, M., Abu-Raddad, L. J., Chico, R. M., Smolak, A., Newman, L., Gottlieb, S., & Thwin, S. S. (2019). Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates, 2016. Bulletin of the World Health Organization, 97(8), 548–562.
Shin, L., & Kaul, R. (2008). Stay it with flora: Maintaining vaginal health as a possible avenue for prevention of human immunodeficiency virus acquisition. Journal of Infectious Diseases, 197, 1355–1357.
Skoler-Karpoff, S., Ramjee, G., Ahmed, K., Altini, L., Plagianos, M. G., Friedland, B., Govender, S., De Kock, A., Cassim, N., & Palanee, T. (2008). Efficacy of Carraguard for prevention of HIV infection in women in South Africa: A randomised, double-blind, placebo-controlled trial. Lancet, 372, 1977–1987.
South African National Department of Health (DOH). (2015). National Antenatal Sentinel HIV & Syphilis Survey Report. Retrieved from https://www.hst.org.za/publications/NonHST%20Publications/Antenatal_Sentinel_survey_Report2012_final.pdf
Street, R., Reddy, T., & Ramjee, G. (2016). The generational effect on age disparate partnerships and the risk for human immunodeficiency virus and sexually transmitted infections acquisition. International Journal of STD & AIDS, 27, 746–752.
Wand, H., & Ramjee, G. (2011). Combined impact of sexual risk behaviors for HIV seroconversion among women in Durban, South Africa: Implications for prevention policy and planning. AIDS and Behavior, 15(2), 479–486.
Wand, H., Reddy, T., Naidoo, S., Moonsamy, S., Siva, S., Morar, N. S., & Ramjee, G. (2018). A simple risk prediction algorithm for HIV transmission: Results from HIV prevention trials in KwaZulu Natal, South Africa (2002–2012). AIDS and Behavior, 22(1), 325–336. https://doi.org/10.1007/s10461-017-1785-7.
World Health Organization. (2016). Global health sector strategy on sexually transmitted infections 2016–2021. Towards ending STIs. Report No. WHO/RHR/16.09. Geneva: Author. Retrieved from http://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for the trials, including all study protocols and informed consent forms, was received from the University of KwaZulu-Natal Biomedical Research Ethics Committee and the South African Medical Research Council Ethics Committee as well as the various study-specific Institutional Review Boards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1: Population Attributable Risk
Appendix 1: Population Attributable Risk
We estimated population attributable risk (i.e. \(PAR\%\)) for the factors in the combined study population using a methodology which can handle complex and correlated nature of the several risk factors in a multivariable model setting (Wand & Ramjee, 2011) where \(PAR\%\)( 95% CIs) were estimated by combining the prevalence of an exposure and its strength with STI incidence (i.e. HRs). For a binary risk factor:
\({\text{HR}}\) is the hazard ratio, \(p\) is the prevalence of the risk factor in the population and \(s\) indexes the two strata determined by the value of the risk factor. In multi-factorial setting:
where \({\text{HR}}_{s}\) and \(p_{s}\), \(s = 1,...,S\), are the hazard ratios and the prevalence of an exposure in the population for the \(s\) th combination of the risk factors.
where \(t\) denotes a stratum of unique combinations of levels of all background risk factors which are not modifiable and/or not under study, \(t = 1,...,T,\) and \(HR_{2t}\) is the hazard ratio in combination \(t\) relative to the lowest risk level, where \(HR_{2,1}\) = 1.
Rights and permissions
About this article
Cite this article
Wand, H., Ramjee, G. & Reddy, T. Quantifying Vulnerabilities of Single Women and Sexually Transmitted Infections in South Africa (2002–2016): Is It Getting Better (or Worse)?. Arch Sex Behav 50, 3237–3245 (2021). https://doi.org/10.1007/s10508-021-01998-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-021-01998-7