Abstract
A globally aging population results in the long-term care of people with chronic illnesses, affecting the living quality of the elderly. Integrating smart technology and long-term care services will enhance and maximize healthcare quality, while planning a smart long-term care information strategy could satisfy the variety of care demands regarding hospitals, home-care institutions, and communities. The evaluation of a smart long-term care information strategy is necessary to develop smart long-term care technology. This study applies a hybrid Multi-Criteria Decision-Making (MCDM) method, which uses the Decision-Making Trial and Evaluation Laboratory (DEMATEL) integrated with the Analytic Network Process (ANP) for ranking and priority of a smart long-term care information strategy. In addition, this study considers the various resource constraints (budget, network platform cost, training time, labor cost-saving ratio, and information transmission efficiency) into the Zero–one Goal Programming (ZOGP) model to capture the optimal smart long-term care information strategy portfolios. The results of this study indicate that a hybrid MCDM decision model can provide decision-makers with the optimal service platform selection for a smart long-term care information strategy that can maximize information service benefits and allocate constrained resources most efficiently.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Long-term care quality is increasingly being recognized among the elderly population, which poses significant challenges for hospitals, home-care institutions, and communities around the world. Population aging is a global development trend; there are 703 million persons aged at least 65 years, which is projected to increase to around 1.5 billion by 2050 (United Nations, 2019). Thus, the world faces a critical aging population problem, including disease control, healthcare support, social insurance legislation, and social welfare resources. Preparing for the economic and social issues associated with an aging population is essential to ensure the implementation of sustainable national development policies (Kazawa et al., 2018). Simultaneously, combining a long-term care system for the elderly with smart technology can improve elderly well-being and make their living environments safe, comfortable, and sustainable.
Management of a smart long-term care information strategy (SLTCIS) has become a crucial topic in academia and the smart healthcare industry. A long-term care policy plays a large role in innovative strategy development processes, as it is one of the most important decision factors regarding care resource utilization (Xu and Intrator, 2019). Long-term care policy reforms should simultaneously consider social and economic drivers, as well as customized patient-oriented services (Maarse and Jeurissen, 2016). In Taiwan, the Ten-year Long-Term Care Plan 2.0 was introduced in 2017, which provides residential care and diversified care services for connecting healthcare with long-term care services. The plan reduces the cost of care and family caregiver pressures to achieve safe and healthy living for the aged. With regard to reducing the caregivers’ burdens of daily needs, this plan effectively utilizes smart healthcare technology to improve the quality and efficiency of long-term care. The main benefits of smart technology can provide care information sharing between hospitals, home-care institutions, and communities. In the healthcare issues regarding smart technology, Torkayesh et al. (2021) proposed a multi-criteria evaluation model based on Type-2 neutrosophic numbers (T2NNs). Their model can identify the contributing factors and understand the adoption of the Internet of Things (IoT) and blockchain in smart medical waste management systems in Turkey. Manikandan et al. (2020) mentioned that combining a smart healthcare information system and the IoT would minimize doctors’ response times. Baskar et al. (2020) presented a framework for the operation of wearable healthcare devices as one of the smart applications.
While it is clear that integrating smart long-term care information technology is a significant driver to accomplishing a sustainable long-term paradigm, many uncertain factors still exist, influencing smart long-term care development and application. Therefore, this study addresses the following main research questions and targets:( i) Which evaluation perspectives and criteria affect the decisions of a smart long-term care information strategy? (ii) Is there an interrelationship between perspective and criteria, respectively? (iii) How can one achieve the weight rankings of a smart long-term care information strategy? (iv) What are the optimal SLTCIS portfolios under constrained resource requirements?
In order to solve these questions and achieve targets, this study proposes a hybrid multi-criteria decision-making model for the optimal portfolio selection of a smart long-term care information strategy with a case study to enhance smart long-term care policy development. This study applies the multi-criteria dimension as a tool for supporting decision-makers in integrating value information to seek definite and feasible alternatives and provide better decision results (Deveci et al., 2021; Simic et al., 2022; Torkayesh & Deveci, 2021). It simultaneously utilizes empirical research through the case study to verify the reliability and accuracy of the decision model, and thus, further increases the quality of decision information (Deveci & Torkayesh, 2021; Simic et al., 2021). Dwivedi et al. (2022) mentioned that cost efficacy is a significant challenge and requires appropriate evaluation, including the cost of development, installation, and usage of smart technology. Therefore, the SLTCIS portfolio should incorporate resource requirements into its decision processes to promote decision information quality.
Multi-criteria decision-making (MCDM) tools are generally applied in solving an optimal decision problem with various alternatives having complex evaluation criteria. Many popular MCDM techniques are applied to deal with solving the best results in diverse evaluation perspectives and criteria, such as the Analytic Hierarchy Process (AHP) (Wind and Saaty, 1980), Analytic Network Process (ANP) (Saaty, 2001), Technique for Order Preference by Similarity to Ideal Solution (TOPSIS) (Hwang & Yoon, 1981), Technique for Order of Preference using Pattern mining based on Risk Aversion (TOPPRA) (Golpîra, 2018), and Vlsekriterijumska Optimizacija Kompromisno Resenje (VIKOR) method (Opricovic, 1998). Integrating the hybrid MCDM method is crucial as it depends on the specifications and characteristics of the decision problem. Further, MCDM is a branch of operational research that analyzes and formulates the optimal results in emerging research issues, such as smart long-term care information strategy evaluation.
The decision model structure developed in this study is a network hierarchy that measures smart long-term care information strategy, which contains complex interdependence among evaluation indicators. For this purpose, the Analytic Network Process (ANP) technique is applied, which can provide a systematic assessment for capturing dependencies among the decision hierarchy model. However, the interrelationships identification of evaluation perspectives and criteria in the ANP method needs rigorous and objective procedures. This deficiency is assisted by integrating the DEMATEL method that can extract the mutual relationships and strength of interdependencies among criteria. In order to satisfy real-world situations implementing smart long-term care information strategies not only a single option but make portfolio decisions will be more practical. This study employed zero–one goal programming (ZOGP) to handle multiple objectives (restricted resources and alternatives importance) decision problems and satisfy the objectives of smart long-term care information strategy portfolio development.
This study formulated three steps to integrate the DEMATEL method and ANP. It considered the various resource constraints in the ZOGP model to capture the optimal smart long-term care information strategy portfolios. DEMATEL is an especially powerful methodology that provides information about the cause-effect relationship between different perspectives (healthcare governance, smart innovation service, sustainable financial development, and resource optimization integration) and criteria and classifies the degree of importance of the different evaluation factors. Subsequently, depending on the relationship between the perspectives and criteria, the weights of smart long-term care information strategy alternatives can be obtained using the ANP method. The model offers government decision-makers an effective analysis of the hierarchy framework. However, responding to real-world situations and knowing how to satisfy the required resource demands are complex practical problems. In this study, various resource constraints (budget, network platform cost, training time, labor cost-saving ratio, and information transmission efficiency), as well as ANP alternative weights, were taken into consideration. In order to verify model reliability and the accuracy of decisions, the ZOGP model was employed to solve the multi-objective decision-making problems. This study aims to accelerate SLTCIS portfolio implementation by establishing evaluation perspectives and criteria for a smart long-term care information platform and providing a straightforward hybrid decision model for government and business practitioners.
The contributions of this study are presented from three different viewpoints, as follows:
-
(i)
From a policy perspective, this optimal portfolio is consistent with the government’s long-term care policy toward smart technology integration. Thus, it can effectively evaluate the smart long-term care information service network platform to assist the elderly by achieving satisfaction with aging care and reducing the burden of care for families.
-
(ii)
From an academic perspective, this study established a hybrid multi-criteria decision-making model which combines the advantages of DEMATEL, ANP, and ZOGP to capture the optimal smart long-term care information strategy portfolios. Simultaneously, the key evaluation perspectives and criteria that influence the SLTCIS decisions were identified, and a case study was utilized to offer decision model verification under constrained resource requirements.
-
(iii)
From the perspective of practical long-term care, this study proposes the SLTCIS decision model to achieve the maximum benefits of each role in the long-term care environment (hospitals, home-care institutions, and communities). This study simultaneously promotes cooperation between hospitals, home-care institutions, and communities to improve the quality of long-term care and effectively allocated human healthcare resources to improve long-term care management.
2 Literature review
A smart long-term care policy emphasizes information integration and evaluation of the information strategies deployed by the smart long-term care environment. Based on the literature review, the three main theoretical dimensions of a smart long-term care information system can be categorized as follows:
2.1 Smart long-term care policy
According to the definition by the World Health Organization in 2000, long-term care is aimed at preserving the highest quality of life for people who do not have the full ability to take care of themselves by providing them with informal caregivers and professionals. Government policy support (i.e., imposing strong regulations) is necessary to achieve this target as it plays an important role in the healthcare industry (Kwon and Jung, 2018). Taiwan started transitioning into an aging society in 1993, with an overall population structure rapidly aging and the number of long-term care needs starting to increase. In order to develop a comprehensive long-term care policy, the government promoted a series of reforms between 1998 and 2016. The recent “Ten-Year Long-term Care Plan 2.0” (LTC 2.0) aims to establish a community-based care model to reduce the pressure on family members and the burden on the capacity of long-term healthcare resources and enhance the quality of life of care receivers and caregivers.
At present, information systems play an important role in long-term care policy by promoting quality and efficient long-term care (Kuo et al., 2016; Qiana et al., 2019). The government has established information systems to support the Smart long-term care policy and promote healthcare quality. The digital learning platform services of long-term care professionals can provide online learning, as well as proof-of-learning hours. As healthcare workers can use the medical affairs service system, caregivers and long-term care institutions can use the care service management information platform to execute care plans. When people need long-term care services, the long-term care geographic information system (LTC-GIS) can display the location of healthcare resources (Ministry of Health and Welfare, 2016).
2.2 Smart long-term care information strategy
Smart healthcare uses a new generation of information technologies, such as the Internet of Things (loT), big data, cloud computing, and artificial intelligence, to reform the traditional healthcare system and make it more efficient, convenient, and personalized (Tian et al., 2019). IoT-based emergency logistics have increasing global concern due to the problems of natural disasters, epidemics, and an aging population. Golpîra et al. (2021) mentioned that emergency logistics developments face many challenges, including various uncertainties, complex communication and coordination, and insufficient resources. More importantly, IoT-based emergency logistics operations require cooperation between local or national public sectors (police forces and ambulance service) and healthcare or medical institutions. IoT-based emergency logistics can assist long-term care resource integration to improve its capabilities and address the information gap among hospitals, home-care institutions, and communities. Qiana et al. (2019) indicated that—with the growing requirements for aged care services, coupled with the global shortage of skilled nursing staff—information technology is expected to reduce this challenge by streamlining nursing work while improving healthcare quality. Chang et al. (2015) mentioned that the long-term care information system was designed to support nurses in nursing care, rehabilitation therapy, and drug management. It can also provide patients with comprehensive care with limited human resources. Papa et al. (2020) provided insights into how Smart wearable devices can influence the health and well-being of the elderly.
The enormous heterogeneity of complex data accumulated from IoT-based emergency logistics must be stored and analyzed appropriately to ensure accuracy and reliability in decision planning. The Smart long-term care information strategy service network platform focuses on optimizing portfolios that employ IoT-based interconnected environments to create effective care service connections between hospitals, home-care institutions, and communities to improve patient care. This study examined the technological maturity and popularity of the smart long-term care information strategy, which are described as follows:
-
Shared decision making strategy (SDM)
Shared decision-making is a process where doctors and patients cooperate in selecting a therapy option based on clinical evidence and the patient’s preference (Härter, Moumjid, Cornuz, Elwyn, and van der Weijden, 2017). Robertson et al. (2018) indicated that a shared decision making strategy in pediatric oncology clinical trials could provide detailed information and sufficient time for patients to make decisions. This strategy will also establish a better doctor-patient relationship, where patients can understand the disease and therapy options and make medical decisions with the doctor, which upgrades the quality of healthcare, provides service satisfaction and meets the security needs of the patient.
-
Smart community health care strategy (SCHC)
Citrin et al. (2018) indicated that a community healthcare system could effectively integrate the patients’ care-center services while maintaining their privacy and dignity. Globally, community-based care service has increasingly become a core component of the healthcare system (Ballard & Schwarz, 2019). From the patient’s perspective, implementing an aging policy can reduce the healthcare burden on the family. The Smart Community Health Care Strategy establishes a community-based long-term care service system that provides an integrated, flexible, and convenient care service to satisfy the demands of its users.
-
Smart home care strategy (SHC)
Menghi, Papetti, and Germani (2019) indicated a need to significantly reduce the hospitalization of patients and increasingly shift the care and monitoring phases to the patients’ homes. Hung and Lin (2020) proposed a Smart home-care system that can conduct real-time patient information and support professional medical advice and response measures to reduce care costs and promote healthcare service. Through the Smart Home Care strategy, caregivers can conduct home visits at regular times and, through their tablets, transmit the relevant disposal records and physiological measurement data of the care receivers to home-care institutions, which assists managers in controlling each case. In addition, when an emergency occurs, care receivers can employ Smart devices, such as wearable devices, to send messages and receive help immediately.
-
Cloud medical record information strategy (CMR)
Globally, many resources are invested in electronic medical records to promote the efficiency and quality of healthcare (Bolgva, Zvartau, Kovalchuk, Balakhontceva, and Metsker, 2017). Doctors can instantly inquire about a patient’s medication profile using the Cloud Medical Record Information Strategy and avoid duplicating medication and wasting resources to improve medication safety and quality. Using this information strategy, community pharmacies can send drugs to chronic patients according to their prescriptions.
-
Health care service management strategy (HCSM)
Zhao, Liu, Qi, Lou, Zhang, and Ma (2020) indicated that a public health information management system has several functions, including health record management, child health, the health of the elderly, health events, health supervision, and management information. The effective management of health records by the healthcare management system has led to its increasing importance (Amoon, Altameem, and Altameem, 2020). Further, using the Health Care Service Management Strategy, caregivers can effectively follow up on case situations and execute care projects, supervise them, link to institutions or localized services, improve care quality, implement case management, manage long-term care institutions, and integrate the diversified requirements of care services.
-
Home-care human resource management strategy (HCHRM)
Löffler, Goldgruber, and Hartinger (2018) indicated that quality management and human resource management are critical factors in the care of elderly people. Even though healthcare is one of the fastest-growing industries in the world, it still faces serious shortages in the availability and retention of human resources (Moses and Sharma, 2020). Using the Home Care Human Resource Management Strategy, patients can easily search for care resources near their homes and ensure the quality of their care. Moreover, education and training for caregivers can be conducted through this strategy, and online learning and proof of learning hours can be provided to enhance the quality of caregivers.
2.3 Evaluation criteria of a smart long-term care information strategy
With respect to the sustainable development of a Smart long-term care information policy, deriving the selection perspectives and criteria consider the management control and business practices necessary for applying the information strategy in a Smart long-term care service platform environment. An integrated hierarchy framework integrates the evaluated perspectives and criteria identified in a literature review. It is designed to incorporate healthcare care governance, Smart innovation services, sustainable financial development, and the optimization and integration of resources, respectively, with regard to the Smart long-term care information strategy portfolios.
-
Health Care Governance
Healthcare governance refers to various related functions performed by decision-makers to achieve health policy objectives. More importantly, adopting a healthcare governance mechanism in a smart long-term care information strategy can achieve long-term value promotion and accountability through interactions between healthcare and social concerns and achieve privacy protection to accomplish the governance goal. To support the Smart long-term care information strategy, Regulatory Compliance (RC) can align its goals with the government’s Smart healthcare policy. Then, through the interaction between Health with Social care Integration (HSI) and privacy protection (PP), it can upgrade the quality of life for the elderly to achieve healthcare governance. In addition, the government should ensures that there is a strong regulatory framework, in which caregivers are trained, and that there is cooperation and integration among various departments (World Health Organization, 2017). Moreover, the critical factors of a healthcare policy are its laws and regulations, which help to formalize and create a sustainable basis for the planning process (World Health Organization, 2016). Mulhern et al. (2019) indicated that the interaction between health and social care is essential for providing longevity and quality of life. Toms et al. (2019) mentioned that social care digital technologies have become the means used for the social care and support of the elderly. Furthermore, the protection of personal data contributes to the development of a Smart healthcare policy. Alraja et al. (2021) mentioned that privacy risks might occur during healthcare information sharing; therefore, privacy protection is one of the critical problems under IoT-based applications.
-
Smart Innovation Service
A Smart innovation service combines technology and innovative service ideas to support a Smart long-term care policy, promote precision medical resources, and apply smart technology to deliver accurate information to improve the quality of doctor-patient relationships. In addition, integrating various resources among the hospitals, communities, and home care institutions will benefit the long-term care process through value-added factors. By developing a Smart long-term care information strategy and maximizing the Precision Medicine Value (PMV), including the implementation of wearable devices and artificial intelligence, patients can obtain relevant information, improve their service satisfaction, and improve the Doctor-Patient Relationship (DPR). Moreover, through the Vertical Integration (VI) services of a hospital, community, and home, healthcare quality is improved, and healthcare resources are saved. Precision medicine refers to tailor-made medical treatment for each patient’s individual needs. Denicolai and Previtali (2020) indicated that precision medicine utilizing smart technology will reduce the waste of resources and gather medical information to predict and control the occurrence of disease. Experts support precision medicine because it includes the ability to promote treatment decisions and provide prognostic information (Vetsch et al., 2019). Liang et al. (2017) showed that a patient-accessible health information system promotes the patients’ perception of service fairness, improves the doctor-patient relationships, and increases patient satisfaction. Grünloh et al. (2018) advocated patient participation as a means of improving patient safety, which is seen as a key component in redesigning healthcare. Lopes et al. (2018) indicated that vertical integration in providing all types of care can take advantage of the existing resources. In order to promote healthcare resource allocation, service resources must be integrated and reinforced to meet the needs of an aging society.
-
Sustainable Financial Development
Sustainable financial development is a critical factor in long-term care. Smart long-term care information strategy planning will increase financial needs, in which sustainable financial resources are one of the significant challenges. Sustainable financial development refers to the capacity of maintaining resources for continuous operations and to react to long-term care environment changes. Sustainable financial development is a major concern of the smart long-term care information strategy planning process. This knowledge highlights the dimension of government support, the smart long-term care industry connection, and cost control. In order to advance the Smart long-term care information strategy, Government Subsidies (GSs) provide the financial resources for care institutions and combine the three value chains of care services, medical services, and long-term care services to promote the Long-term Service Value (LSV) of the care industry. In addition, Effective Cost Control (ECC) can support long-term and sustainable care development, including the initial costs, maintenance costs, and the support and enhancement of system-related long-term costs. The “Regulations for Long-term Care Service Development Awards” clearly stipulate various awards and subsidies. The central governing authority provides award objects and events for long-term care service institutions, providing financial resources for long-term care services. Teymourifar et al. (2021) indicated that subsidy mechanisms contribute to improving the performance of healthcare systems. Accordingly, smart long-term care information strategy implementation needs suitable subsidy policies to support its development. The 2019 PwC report mentioned that a healthcare system infrastructure should be designed to provide effective health services, where the industry value chain of the long-term care industry extends from health promotion to rehabilitation services and from daily needs to care services. The three value chains—life care services, medical services, and long-term care services—are closely related and unique. Moreover, system visibility enables quality and safe care that is transparent and accountable and delivers value to patients (Snowdon and Tallarigo, 2018). However, acquiring an information system application can require an enormous investment for healthcare organizations. Besides the initial costs, a host of long-term costs are associated with maintaining, supporting, and enhancing the system’s operation (Wager et al., 2017).
-
Resource Optimization Integration
Resource optimization and integration maximize the benefits of long-term care services. The smart long-term care service platform includes the various information strategies of associated long-term care environments and applications to offer high-quality and more long-term care services. More importantly, long-term care population planning is contributing to the development of the smart long-term care industry, as well as reasonable resource allocation and process optimization, which are helping achieve long-term service platform performance. The evaluation of a Smart long-term care information strategy includes whether it has an Adequate Service Capacity (ASC), can popularize long-term care services, trains caregivers, and employs mediation. In addition, through Healthcare Process Optimization (HPO), the resources are allocated optimally to improve work efficiency. Finally, it combines home, community, and care institutions and integrates medical, pharmaceutical, and assistive devices to achieve effective Healthcare Resource Utilization (HRU) and provide good care for patients. Ker et al. (2018) indicated that using a healthcare information system offers the possibility of reducing the patient-flow delays of outpatients—and those related to inpatient flow—to promote healthcare quality. The government also approved the plan to improve the long-term care service capacity in 2015, thereby accelerating the establishment and popularization of long-term care services and human resources, strengthening the efficiency of long-term care services, enhancing their effectiveness and quality, and expanding the service targets. Information technology can support nurses and caregivers to provide better quality care to care receivers and to improve their own work processes (Qiana et al., 2019). Abdalkareem et al. (2021) mentioned that enhancing, planning, and scheduling the procedures for healthcare resources play a vital role in improving the healthcare benefits and service quality delivered to patients. Schipper et al. (2015) indicated that the optimal utilization of resources is an important reason for reducing the administrative burden of care institutions. The summary of this research is presented in Table 1, and the research framework is depicted in Fig. 1.
3 Research methodology
This study constructed an MCDM model combined with the DEMATEL, ANP, and ZOGP models. This section demonstrates the process of the evaluation model.
3.1 Decision-making trial and evaluation laboratory
DEMATEL originated in the Geneva Research Centre of the Battelle Memorial Institute (Gabus & Fontela, 1972, 1973). It aims to construct a relationship between the causes and effects of various criteria. Based on a literature review, this study constructed the evaluation criteria for a Smart long-term care information strategy. It includes Regulatory Compliance (RC), Health and Social Care Integration (HSI), Privacy Protection (PP), Precision Medicine Value (PMV), Improved Doctor-Patient Relationship (DPR), Vertical Integration Services (VIS), Government Subsidy (GS), Promote Long-term care Industry Service Value (LSV), Effective Cost Control (ECC), Adequate Service Capacity (ASC), Health Care Process Optimization (HPO), and Health Care Resource Utilization (HPU). The major steps of DEMATEL are as follows (Arabsheibani et al., 2016; Li et al., 2014; Lin, 2013; Rad et al., 2018):
Step 1: Construct and calculate the average direct-relation matrix
To compare the degree of the relative importance of perspectives and criteria, a scale is established. The level of scale measurement consists of no influence (0), low influence (1), medium influence (2), high influence (3), and extreme influence (4). Then, a group of experts identifies the level of direct influence between two perspectives and criteria elements to establish pair-wise comparisons and form the mathematical matrix. Assuming the factors contain several criteria,\({\text{S}} = \left\{ {{\text{S}}_{1} ,{\text{ S}}_{2} \cdots {\text{S}}_{{\text{N}}} } \right\}\), experts propose the level of direct influence between each criterion and derive an average matrix,\({\text{H}}\), where \({\text{e}}_{{{\text{ij}}}}\) denotes the level criterion \(S_{i}\) exerts on criterion \(S_{j}\), in which all major diagonal criteria are equal to zero. The average matrix \({\text{ H}}\) is shown as follows:
Step 2: Calculate the normalized direct-relation matrix and total-relationship matrix.
A normalized direct-relation matrix \({\text{U}}\) can be acquired by multiplying matrix \({\text{H}}\) and s, as in Eqs. (1) and (2)
and continuously decreasing the indirect effects of problems along the powers of \({\text{ U}}\), such as \({\text{U}}^{2} ,{\text{U}}^{3} ,{ } \cdots ,{\text{U}}^{{\text{k}}}\) and \(\mathop {\lim }\limits_{{{\text{k}} \to \infty }} {\text{U}}^{{\text{k}}} = \left[ 0 \right]_{{{\text{n}} \times {\text{n}}}}\), where \({\text{ U}}^{{\text{k}}} = \left[ {{\text{u}}_{{{\text{ij}}}} } \right]_{{{\text{n}} \times {\text{n}}}}\), \(0 \le {\text{u}}_{{{\text{ij}}}} < 1.\)
Then, a total-relationship matrix \({\text{T}}\) can be derived through Eq. (3), where \({\text{I}}\) denotes an \({\text{n}} \times {\text{n}}\) identity matrix
Then,
Step 3: Find the cause and effect groups and set the threshold values to obtain the impact-relation map.
Calculate the sums of rows \({\text{D}}\) and columns \({\text{R}}\) of the total- relationship matrix \({\text{ T}}\). Vectors \({\text{D}}\) and \({\text{R}}\) can be calculated as shown in Eqs. (4) to (6):
where \({\text{D}}\) is the sum of the rows in matrix \({\text{ T}}\), the value of \({\text{D}}\) indicates the total effects, both direct and indirect, that criterion \({\text{i}}\) exerts on the other criteria; and \(\mathrm{R}\) is the sum of columns in matrix \(\mathrm{T}\), presenting the total effects, both direct and indirect, that criterion \(\mathrm{i}\) receives from the other criteria. Concurrently, the values of D-R and D + R are obtained. Some criteria, called the cause group, have a positive D-R value, indicating that criterion \(\mathrm{i}\) affects the other criteria; conversely, if the D-R value is negative, criterion \(\mathrm{i}\) is influenced by the other criteria; this is called the effect group. Moreover, the value of D + R indicates an index of intensity of the influences delivered and received and presents the relationships among criteria. The threshold value is computed in order to construct the impact-relation map. The threshold value p is calculated by taking the average or discussing all the factors in the total relation matrix with the experts. The overall value in matrix H reflects how one factor influences other factors; hence, the threshold value assists in filtering out the critical and insignificant factors affecting the relationships. The impact-relation map is obtained by drawing the values of (D + R, D-R), where the horizontal axis is D + R and D-R is set as the vertical axis, to visualize the complex interrelationships and provide information by which to judge the most important criteria and the influence of the relationships among criteria.
3.2 Analytical network process
The Analytical Hierarchy Process (AHP) is a strong and flexible multi-criteria decision analysis tool (Wind and Saaty, 1980), focusing on dominant matrices and their corresponding measurements and using a unidirectional hierarchical relationship among the decision levels as a framework. ANP is a more general form of AHP introduced by Saaty in 2001. It permits complicated interrelationships between the decision levels and attributes (Rad et al., 2018). This study describes six SLTCISs, including the shared decision making strategy (SDM), the smart community health care strategy (SCHC), the smart home care strategy (SHC), the cloud medical record information strategy (CMR), the health care service management strategy (HCSM), and the home care human resource management strategy (HCHRM). The ANP method can calculate the relative weight of each strategy and derive the interdependence of each criterion and strategy, as well as the priority weights. The major steps of ANP are as follows (Lin et al., 2008):
Step 1: Define the policy issues and establish the policy-making members
To determine the scope of the discussions, all influential factors of the policy issue should be considered based on the character of the issue. A group of decision-makers should be established to integrate experts’ suggestions in the corresponding domain according to the degree of complication and the different fields and to categorize the corresponding information to determine the critical issues affecting the decisions.
Step 2: Issuing a questionnaire and integrating expert preferences
In the expert questionnaire, the experts give each element a weight according to the corresponding upper element to collect opinions regarding the relative importance of the different elements. Then, the level of the expert’s preference assessment and the geometric mean can be used to calculate the overall weights.
Step 3: Establish the comparison matrices
After synthesizing the judgments and opinions of various experts, a comparison matrix of multiple evaluation criteria and options can be constructed. The ANP method uses a measurement scale of 1–9; based on this scale, the relative weights are obtained. Subsequently, the interdependence and relative importance of each evaluation criterion can be computed.
Step 4: Analyze consistency
In the ANP method, the decision-makers or experts who make judgments or have opinions must perform a consistency test according to the Consistency Ratios (CR) of the comparison matrices, which are determined as follows:
where C.I. means the consistency index and R.I. means the random index.
Consistency indicators indicate the degree of difference between the maximum feature value and the number of hierarchy levels, and they are used as a measure of the degree of consistency. If C.R. ≦ 0.1, the degree of consistency is satisfied and acceptable; however, if C.R. > 0, it indicates conflicting judgments among the decision-makers and experts. A Random Index is based on the number of levels in the comparison matrix: that is, the number of comparative elements.
Step 5: Calculate the supermatrix
Collectively, the corresponding priorities of evaluation strategies form the unweighted and weighted super-matrix and limiting powers until the weights converge to stabilize the limited super-matrix. Hence, higher priority weighting evaluation alternatives (Smart long-term care information strategy) indicate that the evaluation strategies with the greatest priority will be selected.
3.3 Zero–one goal programming
The ZOGP method is a tool used to solve MCDM problems and consider resource constraints (Charnes, Cooper, and Ferguson, 1955). Tsai and Kuo (2011) adopted this method to help policymakers evaluate and select a feasible entrepreneurship policy mix under various budget constraints. Yang et al. (2016) employed ZOGP to find the best combination of sustainable public transport infrastructure projects under constrained resources.
This study considers five constraints: the total budget, Smart long-term care network platform cost allocation, training time, the labor cost-saving ratio, and information transmission efficiency. The ZOGP model is a tool used to select multiple alternatives with the minimum overall deviation from the goals (Kengpol et al., 2012). The ZOGP model is described as follows.
Subject to
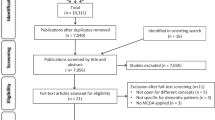
where Z is the sum of the deviation from m targets; n is the policy pool to choose the best set from; \({\text{Q}}_{{\text{k}}}\) indicates a preemptive priority (\({\text{Q}}_{1}\) \(\succ\) \({\text{Q}}_{2} \succ\) \({\text{Q}}_{3} \succ \succ \succ {\text{Q}}_{{\text{k}}}\)) for targets; \({\text{d}}_{{\text{i}}}^{ - }\) and \({\text{d}}_{{\text{i}}}^{ + }\) are the negative or positive deviation variables, respectively, for the choice criterion (resource) \({\text{i}}\); \({\text{w}}_{{\text{j}}}\) is the ANP weight on the \({\text{j}}^{{{\text{th}}}}\) policies; \({\mathrm{a}}_{\mathrm{ij}}\) is the policies parameter \(\mathrm{j}\) of choice resource\(\mathrm{i}\); \({\mathrm{b}}_{\mathrm{i}}\) indicates the available resources considered in the choice decision; and \({\text{x}}_{{\text{j}}}\) denotes the binary variable. According to the defined alternatives and criteria introduced in this study, it is important to demonstrate the feasibility of the MCDM model. This study aims to establish a Smart long-term care information strategy decision model for evaluating the optimal SLTCIS portfolios, which effectively satisfies multiple resource requirements. The research flow is shown in Fig. 2.
4 Case study
4.1 Case study background
This study presents the following situation as an example:
The government decision-maker plans to implement Smart long-term information strategies to promote healthcare quality. Taiwan’s government has made a series of reforms to the long-term care policy, including the combination of long-term care service and information technology, and has developed smart long-term care information strategies (SLTCISs) to promote the quality of long-term care. The decision-makers’ plan is to establish a service network platform that includes several SLTCISs to be utilized between long-term care environments, namely, hospitals, home-care institutions, and communities. Six SLTCIS alternatives meet the requirements of the long-term care industry. However, due to limited government resources, all alternatives—including the total budget, cost allocation for a long-term care smart network platform, training times, labor cost-saving ratio, and information transmission efficiency—cannot be implemented. To solve this decision-making problem, the MCDM model must first be applied to obtain the priority of each alternative. Then, the ZOGP method should be utilized to obtain the optimal Smart long-term care information strategy portfolio with limited resources. The analysis steps are described as follows:
Step 1: Apply DEMATEL to evaluate the relationship between the perspectives and criteria.
DEMATEL was employed to explore the relevance of each perspective and criterion. At the same time, the experts’ feedback was utilized to determine the direction of influence. This study used a total of six experts, including doctors, home-care institutions supervisors, and caregivers, and their average seniority was 9.2 years, as shown in Table 2. The DEMATEL questionnaire was issued between July and August 2019.
Using the DEMATEL method (Eqs. (1)–(6)), the criteria scale and pair-wise comparisons from the expert panel determine the intensity of the influence direction for each criterion in order to acquire the total relationship matrix. Initially, the main perspective and criteria are evaluated, and the experts provide responses to the opinions. The average matrix (H) is conducted (the perspective and criteria value are presented in Appendix A- Tables 11, 12) by the expert questionnaire. Furthermore, the normalized initial direct-relation matrix (U) is formed (the perspective and criteria value are presented in Appendix A- Tables 13, 14) by Eqs. (1) and (2). Finally, the total-relationships matrix (T) is calculated (as shown in the perspective value of Table 3 and the criteria value of Table 4, respectively) using Eq. (3). To make the structure distinct and to present the impact-relation map, the threshold value of 2.363 for perspective and 0.726 for criterion are selected for discussion by the experts. From the decision-makers’ point of view, Health Care Governance (HCG), Resource Optimization Integration (ROI), and Sustainable Financial Development (SFD) are regarded as the most influential evaluation perspectives in the decision to evaluate SLTCIS portfolio strategy in the context of Taiwan. Simultaneously, if the value in the matrix is greater than the threshold value, the column criterion strongly affects the row criterion. The impact-relation map helps to understand the structure in terms of recognizing the influence of one success factor over another and filtering out insignificant effects (Fig. 3). Noteworthily, effective financial support promotes smart long-term care information strategy development and implementation.
Based on Table 4 and Fig. 4, obtaining influential weights of criteria with DEMATEL reveal calculation processes, Regulatory Compliance (RC), Privacy Protection (PP), Improve Doctor-patient Relationship (DPR), Government Subsidy (GS), Effective Cost Control (ECC), Healthcare Process Optimization (HPO), and Healthcare Resource Utilization (HRU) are considered. Privacy Protection (PP) with (D–R = 1.008) is regarded as the most important one among the cause groups. According to the above-discussed results, decision-makers should focus on health care governance, especially in the monitoring process, in addition to maintaining privacy protection for the patient but enhancing the high quality and safety of the long-term care environment.
Step 2: Priority weights of evaluation projects applied by ANP
The relationship between the perspectives and criteria, as calculated by DEMATEL, was applied to the ANP method. To measure the level of influence between the criteria, the experts offered professional advice through a pair-wise comparison based on Saaty’s nine-point scale. To determine the relative values, the scale uses 1 to 9 to indicate the influence levels, from ‘equal importance’ to ‘extreme importance’, respectively, and the entire calculation process was completed using the Super Decision software. The corresponding priorities of the perspectives and criteria establish the unweighted and weighted super-matrix and the limiting ability until the weight converges to stabilize the limited super-matrix. The consistency tests show that the consistency ratio (CR) is less than 0.1. Therefore, the results indicate that for the smart long-term care information strategy, the experts gave high priority to the Smart Community Health Care Strategy, followed by the Health Care Service Management Strategy \(\succ \) the Smart Home Care Strategy \(\succ \) the Home Care Human Resource Management Strategy \(\succ \) the Shared Decision Making Strategy \(\succ \) the Cloud Medical Record Information Strategy (Table 5). These results indicate that the Smart Community Health Care Strategy implements an aging policy and provides an integrated, flexible, and convenient care service while reducing the family burden.
Step 3: ZOGP analysis
This study aimed to establish an evaluation decision model of the service network platform that includes several Smart long-term care information strategies to be utilized in the long-term care environment of hospitals, home-care institutions, and communities. Due to the evaluation planning processes and the uncertain nature of the overall service network platform environment, obtaining real and specific data information regarding the resource inputs is difficult. To overcome the challenge of obtaining the actual data for the evaluation objects of a smart long-term care information strategy, most of the deterministic data (e.g., the network platform cost allocation and training hours) were referred from the interviews with the experts and business information. In fact, the long-term care problem of aging affects the utilization of healthcare environment resources, and the government must consider resource allocation and the limitations of maximizing the healthcare benefits in a significant Smart information strategy plan. Five resources constraints are considered, as shown in Table 6: (1) the total maximum budget of NT$450 million; (2) the total maximum long-term care smart network platform cost allocation of NT$2500 million to establish it; (3) the total maximum training time of 48 h; (4) the total maximum labor cost-saving ratio of 38%; and (5) the total maximum information transmission efficiency of 80%.
The developed mathematical optimization model applied the weights resulting from the ANP and considered the resource constraints. Table 7 illustrates the ZOGP model formulation and shows the ANP prioritized weights and \(d_{i}^{ + }\) and \(d_{i}^{ - }\). The binary variables are \(x_{1}\)(SDM), \(x_{2}\)(SCHC), \(x_{3}\)(SHC), \(x_{4}\)(CMR), \(x_{5}\)(HCSM), and \(x_{6}\)(HCHRM). \(x_{j} = 1\) presents that the \(j^{th}\) SLTCIS is selected, and \(x_{j} = 0\) presents that the \(j^{th}\) SLTCIS is not selected. The following model is constructed by the ZOGP method with the relevant constraints and parameters:
In summary, the weighting order of each smart long-term care information strategy by the ANP method is combined with the ZOGP method to obtain an optimal smart long-term care information strategy portfolio with resource constraints (the total budget, long-term care smart network platform cost allocation, training time, labor cost-saving ratio, and information transmission efficiency). The results indicate that the Shared Decision Making Strategy (SDM), the Smart Community Health Care Strategy (SCHC), the Health Care Service Management Strategy (HCSM), and the Home Care Human Resource Management Strategy (HCHRM) comprise the optimal smart long-term care information strategy portfolio in a long-term care environment. This portfolio can be applied in the long-term care environment, enabling hospitals, home-care institutions, and communities to effectively use healthcare resources and improve the quality of long-term care. From the patient’s perspective, the Shared Decision Making Strategy helps them understand their diseases and their therapy options. It also helps both the doctors and patients to make a common medical decision, which will improve the efficiency of doctor-patient communication. When returning home, the community-based long-term care service system provides an integrated, flexible, and convenient care service that will reduce the family’s healthcare burden. Moreover, caregivers can execute care projects and effectively track specific cases using the Health Care Service Management Strategy. The system can help different caregivers understand the situation and improve healthcare, while the human resources can be managed effectively through the Home Care Human Resource Management Strategy, which will enable people to inquire about the care facilities near their homes and to make appropriate allocations for the full use of their human resources.
4.2 Comparative and additional analyses
In order to identify the best evaluation methodology for a smart long-term care information strategy portfolio decision problem, a measure attributes comparison or integration of different MCDM methods can be applied, as it offers a deep insight into the research topic and future directions of potential research. MCDM tools are generally applied in solving an optimal decision problem with various alternatives having complex evaluation criteria. Despite each MCDM tool’s distinct advantages, it still has room for improvement. This lack is covered using a hybrid decision model, combining the methodology theory strength to provide more objective research contributions. Table 8 is a summary of some of the popular decision analysis methods indicating decision principles, strengths, and weaknesses, respectively.This section mainly presents an additional analysis to confirm the reliability and accuracy of the presented results. The following validation analysis is compared with the AHP and ANP methods and integrated into the VIKOR technique application.
-
Comparative analysis
This section compares the results from AHP, which measures the critical success factors from the independent perspective with the ANP methodology to solve the smart long-term care information strategy decision problem. ANP considers the interrelationships among the critical success factors, and the weights of the criteria in the AHP and ANP models are compared in Table 9.
The finding shows that following the AHP ranking of the critical success factors for the first third priority: Adequate Service Capacity (weight = 0.2006), Vertical Integration Service (weight = 0.1581), and Health Care Resource Utilization (weight = 0.1368). In the ANP method evaluation results, the ranking of the critical success factors is the first third priority: Regulatory Compliance (weight = 0.1732), Industry Service Value (weight = 0.1732), and Health Care Process Optimization (weight = 0.1264). From the point of view of the national long-term care policy, the implementation and development of SLTCIS require regulatory support, attention to industry service value maximization, and enhanced healthcare process optimization.
A comparison of the results showed significant differences between AHP and ANP outcomes derived from interdependencies and feedback. Particularly, this study utilized the DEMTATEL method to identify the interrelationship among evaluation perspectives and criteria. Further, to combine the advantages of the qualitative and quantitative methods, it considers the dependency of the criterion in the analytic network and the inclusive resource requirement constraints in the ZOGP model.
-
Additional analysis
This section describes the integration of the VIKOR technique application. The VIKOR method, developed by Opricovic (1998), identifies the compromise solution from decision alternatives. The compromise ranking process determines the best (utility) value and the worst (regret) value for the evaluation criteria. The utility (\({S}_{i}\)) value, regret (\({R}_{i}\)) value, and VIKOR index (\({\mathrm{Q}}_{i}\)) is calculated as shown in Eqs.(8) to (10):
where:
\({S}_{i}\) represents the utility value;\({R}_{i}\) represents the regret value;\({w}_{j}\) represents the ANP weights of SLTCISs.\({a}_{i}^{*}\) and \({a}_{i}^{-}\) indicate the best value and worst value among the SLTCISs alternative for each evaluation criteria; \({a}_{ij}\) indicate the value corresponding to each evaluation criterion with respect to the SLTCISs alternative.
\({Q}_{i}\) represents the \(ith\) decision alternatives VIKOR index value, namely smart long-term care information strategies (SLTCISs), \(i=\mathrm{1,2},\cdots ,m\).
\({S}^{*}\) and \({S}^{-}\) represent the maximum and minimum value of utility value, and \({R}^{*}\) and \({R}^{-}\) represent the maximum and minimum value of regret value, respectively.
The decision alternatives were ranked based on the minimum values obtained in accordance with satisfying two conditions:
The alternative Q1 is accepted if (Q2 – Q1)\(\ge 1/n-1\), where Q2 is the second rank alternative in the analysis process and n is the number of alternatives.
The alternative Q1 is stable if it obtains the best-ranked alternative in \({S}_{i}\) and \({R}_{i}\) scores.
A compromise solution is a feasible solution closest to the ideal solution. Incorporating the ANP weights of evaluating criteria into the VIKOR method to extract the compromise solution of smart long-term care information strategy. The values of \({S}_{i}\), \({R}_{i}\), and \({Q}_{i}\) were computed by selecting v = 0.5 and are shown in Table 10. The results indicated that the value of \({Q}_{i}\) is (SDM, SCHC, SHC, CMR, HCSM, HCHRM) = (0.533, 0.296, 0.571, 0.603, 0.519, 0.572), of which the ranking is SCHC ≻ HCSM≻ SDM ≻ SHC ≻ HCHRM ≻ CMR. Smart Community Health Care Strategy was the closest to the ideal solution. The performance variance rate was 0.296. It represented Medical Data Informational System still had some gaps (0.296) in the goal value. Simultaneously, Smart Community Health Care Strategy (SCHC) satisfied both conditions, i.e., \({Q}_{i}\)(HCSM)\(- {Q}_{i}\)(HCSM)\(\ge \) \(1/(6-1)\) and \({Q}_{i}\)(HCSM) obtained the first rank according to both the \({S}_{i}\) and \({R}_{i}\) scores.
5 Conclusion and Policy implications
5.1 Conclusion
Long-term care quality is increasingly being recognized among the elderly population, posing significant challenges for hospitals, home-care institutions, and communities around the world. This study proposed a hybrid Multi-Criteria Decision-Making model for the optimal portfolio selection of a smart long-term care information strategy with a case study to enhance smart long-term care policy development. Based on the case study, this study draws the following conclusions.
-
Evaluation perspectives and criteria that affect the decisions regarding the smart long-term care information strategy were established through the literature review. After DEMATEL analysis, the total-relationships matrix of the perspectives and criteria was defined. The values of importance (D + R = 19.85) determined the Sustainable Financial Development plan. Additionally, Health Care Governance, Sustainable Financial Development, and Resource Optimization Integration were measured into the cause group factors. Notably, effective financial support will promote smart long-term care information strategy development and implementation.
-
Next, the priority rankings of the smart long-term information strategies obtained from the ANP methodology are: Smart Community Health Care Strategy (0.1933) ≻ Health Care Service Management Strategy (0.1872) ≻ Smart Home Care Strategy (0.1688) ≻ Home Care Human Resource Management Strategy (0.1587) ≻ Shared Decision Making Strategy (0.1462) ≻ Cloud Medical Record Information Strategy (0.1458). This result indicates that smart community healthcare aims to work in partnership with long-term community services to promote and protect aging people’s health and social well-being.
-
In verifying the decision model reliability and accuracy, this study considered various resource constraints (budget, network platform cost, training time, labor cost-saving ratio, and information transmission efficiency), as well as the ANP alternative weights. The ZOGP model was also employed to solve the multi-objective decision-making problems. The optimal smart long-term care information strategy portfolio includes the Shared Decision Making Strategy (SDM), the Smart Community Health Care Strategy (SCHC), the Health Care Service Management Strategy (HCSM), and the Home Care Human Resource Management Strategy (HCHRM). Thus, the hybrid decision model selected the SLCIS portfolio as most suitable for the smart long-term care service network platform, and this result meets the real-world situation in Taiwan.
-
The comparative analysis concluded that the rankings obtained from the ANP and AHP methods demonstrate the dependency among critical success factors for a smart long-term care information service platform as an important concern. According to the interdependence and interrelationships, the ANP method was more objective and accurate in solving real-life decision problems.
-
The additional analysis indicated that applying the VIKOR to obtain the compromise solution provides a substitute analysis methodology. Interestingly, the best decision alternative (Smart Community Health Care Strategy) from the VIKOR analysis was consistent with the finding of ANP computing results. Although there are differences in decision principles, strengths, and weaknesses, the optimal decision alternative may not fluctuate.
The major limitation of this study is that the decision matrix only focused on certain perspectives, criteria, and alternatives; therefore, more evaluation factors and alternatives can be considered in the future. In particular, under the COVID-19 pandemic environment, a smart long-term care information strategy may have different benefits. Thus, different resource requirements can be further designed using business information, and then, the hybrid MCDM model can be used to plan smart hospital information service infrastructures. Although the results obtained from this study are satisfactory, there exists improvement direction to considering other mathematical methods that solve real-world decision problems, such as the Technique for Order of Preference using Pattern mining based on Risk Aversion (TOPPRA) and compared to the goal programming and resource requirement has been applied in this study.
5.2 Policy implications
To show the real-world applicability of this study, the proposed hybrid MCDM model was extended to a case study of the national healthcare environment in Taiwan. This study makes the following recommendations for developing a smart long-term care information service platform regarding the challenges of the increasing elderly population, which will improve the decision quality of the evaluation process and provide useful policy directions and practical insights.
-
From a policy perspective, this optimal portfolio is consistent with the government’s long-term care policy toward smart technology integration. Effective evaluation of the smart long-term care information service network platform will assist the elderly in achieving aging care satisfaction and reduce the burden of care for families.
-
From an academic perspective, this study established a hybrid Multi-Criteria Decision-Making (MCDM) model by combining the advantages of DEMATEL, ANP, and ZOGP methodologies to capture the optimal smart long-term care information strategy portfolios. The key evaluation perspectives and criteria that influence SLTCIS decisions are simultaneously identified and utilized in a case study to offer decision model verification under constrained resource requirements.
-
From the perspective of long-term care practices, this study proposed the SLTCIS decision model to achieve the maximum benefits for each role in long-term care environments (hospitals, home-care institutions, and communities). Cooperation between hospitals, home-care institutions, and communities will simultaneously promote long-term care quality and effectively allocate human healthcare resources to improve long-term care management.
References
Abdalkareem, Z. A., Amir, A., Al-Betar, M. A., Ekhan, P., & Hammouri, A. I. (2021). Healthcare scheduling in optimization context: a review. Health and Technology, 11(3), 445–469.
Alraja, M. N., Barhamgi, H., Rattrout, A., & Barhamgi, M. (2021). An integrated framework for privacy protection in IoT—Applied to smart healthcare. Computers & Electrical Engineering, 91, 107060.
Amoon, M., Altameem, T., & Altameem, A. (2020). Internet of things sensor assisted security and quality analysis for health care data sets using artificial intelligent based heuristic health management system. Measurement, 161, 107861.
Arabsheibani, R., Kanani Sadat, Y., & Abedini, A. (2016). Land suitability assessment for locating industrial parks: a hybrid multi criteria decision-making approach using geographical information system. Geographical Research, 54(4), 446–460.
Ballard, M., & Schwarz, R. (2019, September). Employing practitioner expertise in optimizing community healthcare systems. In Healthcare (Vol. 7, No. 3, p. 100334). Elsevier.
Baskar, S., Shakeel, P. M., Kumar, R., Burhanuddin, M. A., & Sampath, R. (2020). A dynamic and interoperable communication framework for controlling the operations of wearable sensors in smart healthcare applications. Computer Communications, 149, 17–26.
Bolgva, E. V., Zvartau, N. E., Kovalchuk, S. V., Balakhontceva, M. A., & Metsker, O. G. (2017). Improving electronic medical records with support of human computer interaction in medical information systems. Procedia Computer Science, 121, 469–474.
Chang, I. C., Chang, C. H., Wu, J. W., & Huang, T. C. K. (2015). Assessing the performance of long-term care information systems and the continued use intention of users. Telematics and Informatics, 32(2), 273–281.
Charnes, A., Cooper, W. W., & Ferguson, R. O. (1955). Optimal estimation of executive compensation by linear programming. Management Science, 1(2), 138–151.
Citrin, D., Thapa, P., Nirola, I., Pandey, S., Kunwar, L. B., Tenpa, J., ... & Maru, D. (2018, September). Developing and deploying a community healthcare worker-driven, digitally-enabled integrated care system for municipalities in rural Nepal. In Healthcare (Vol. 6, No. 3, pp. 197–204). Elsevier.
Denicolai, S., & Previtali, P. (2020). Precision Medicine: Implications for value chains and business models in life sciences. Technological Forecasting and Social Change, 151, 119767.
Deveci, M., Simic, V., & Torkayesh, A. E. (2021). Remanufacturing facility location for automotive Lithium-ion batteries: an integrated neutrosophic decision-making model. Journal of Cleaner Production, 317, 128438.
Deveci, M., & Torkayesh, A. E. (2021). Charging type selection for electric buses using interval-valued neutrosophic decision support model. IEEE Transactions on Engineering Management. https://doi.org/10.1109/TEM.2021.3108062
Dwivedi, R., Mehrotra, D., & Chandra, S. (2022). Potential of Internet of Medical Things (IoMT) applications in building a smart healthcare system: A systematic review. Journal of Oral Biology and Craniofacial Research, 22(2), 302–318.
Gabus, A., & Fontela, E. (1972). World problems, an invitation to further thought within the framework of DEMATEL. Battelle Geneva Research Center, Geneva, Switzerland, 1(8).
Gabus, A., & Fontela, E. (1973). Perceptions of the world problematique: Communication procedure, communicating with those bearing collective responsibility (DEMATEL report no. 1). Switzerland Geneva: Battelle Geneva Research Centre.
Golpîra, H. (2018). A novel Multiple Attribute Decision Making approach based on interval data using U2P-Miner algorithm. Data & Knowledge Engineering, 115, 116–128.
Golpîra, H., Khan, S. A. R., & Safaeipour, S. (2021). A review of logistics internet-of-things: Current trends and scope for future research. Journal of Industrial Information Integration, 22, 100194.
Grünloh, C., Myreteg, G., Cajander, Å., & Rexhepi, H. (2018). “Why do they need to check me?” patient participation through eHealth and the doctor-patient relationship: Qualitative study. Journal of Medical Internet Research, 20(1), e8444.
Härter, M., Moumjid, N., Cornuz, J., Elwyn, G., & van der Weijden, T. (2017). Shared decision making in 2017: International accomplishments in policy, research and implementation. Zeitschrift Für Evidenz, Fortbildung Und Qualität Im Gesundheitswesen, 123, 1–5.
Hung, L. P., & Lin, C. C. (2020). A multiple warning and smart monitoring system using wearable devices for home care. International Journal of Human-Computer Studies, 136, 102381. https://doi.org/10.1016/j.ijhcs.2019.102381
Hwang, C. L., & Yoon, K. (1981). Methods for multiple attribute decision making. Multiple attribute decision making: methods and applications a state-of-the-art survey, 58–191.
Kazawa, K., Rahman, M. M., & Moriyama, M. (2018). An investigation of factors influencing high usage of medical and long-term care services in an aging society in Japan. Asia Pacific Journal of Public Health, 30(2), 95–106.
Kengpol, A., Meethom, W., & Tuominen, M. (2012). The development of a decision support system in multimodal transportation routing within Greater Mekong sub-region countries. International Journal of Production Economics, 140(2), 691–701.
Ker, J. I., Wang, Y., & Hajli, N. (2018). Examining the impact of health information systems on healthcare service improvement: The case of reducing in patient-flow delays in a US hospital. Technological Forecasting and Social Change, 127, 188–198.
Kim, H., Kwon, S., Yoon, N. H., & Hyun, K. R. (2013). Utilization of long-term care services under the public long-term care insurance program in Korea: Implications of a subsidy policy. Health Policy, 111(2), 166–174.
Kuo, M. H., Wang, S. L., & Chen, W. T. (2016). Using information and mobile technology improved elderly home care services. Health Policy and Technology, 5(2), 131–142.
Kwon, H., & Jung, E. Y. (2018). The impact of policy on the growth of precision medicine. Health Policy and Technology, 7(4), 347–357.
Li, Y., Hu, Y., Zhang, X., Deng, Y., & Mahadevan, S. (2014). An evidential DEMATEL method to identify critical success factors in emergency management. Applied Soft Computing, 22, 504–510.
Liang, C., Gu, D., Tao, F., Jain, H. K., Zhao, Y., & Ding, B. (2017). Influence of mechanism of patient-accessible hospital information system implementation on doctor–patient relationships: A service fairness perspective. Information & Management, 54(1), 57–72.
Lin, R. J. (2013). Using fuzzy DEMATEL to evaluate the green supply chain management practices. Journal of Cleaner Production, 40, 32–39.
Lin, Y. H., Chiu, C. C., & Tsai, C. H. (2008). The study of applying ANP model to assess dispatching rules for wafer fabrication. Expert Systems with Applications, 34(3), 2148–2163.
Löffler, K., Goldgruber, J., & Hartinger, G. (2018). Moving towards a competence centre for geriatric medicine and care: Quality management and human resource management as major support factors. Best Practice & Research Clinical Anaesthesiology, 32(1), 47–55.
Lopes, H., Mateus, C., & Hernández-Quevedo, C. (2018). Ten years after the creation of the Portuguese national network for long-term care in 2006: Achievements and challenges. Health Policy, 122(3), 210–216.
Maarse, J. H., & Jeurissen, P. P. (2016). The policy and politics of the 2015 long-term care reform in the Netherlands. Health Policy, 120(3), 241–245.
Manikandan, R., Patan, R., Gandomi, A. H., Sivanesan, P., & Kalyanaraman, H. (2020). Hash polynomial two factor decision tree using IoT for smart health care scheduling. Expert Systems with Applications, 141, 112924.
Menghi, R., Papetti, A., & Germani, M. (2019). Product Service Platform to improve care systems for elderly living at home. Health Policy and Technology, 8(4), 393–401.
Moses, A., & Sharma, A. (2020). What drives human resource acquisition and retention in social enterprises? An empirical investigation in the healthcare industry in an emerging market. Journal of Business Research, 107, 76–88.
Mulhern, B., Norman, R., Lourenco, R. D. A., Malley, J., Street, D., & Viney, R. (2019). Investigating the relative value of health and social care related quality of life using a discrete choice experiment. Social Science & Medicine, 233, 28–37.
Opricovic, S. (1998). Multicriteria optimization of civil engineering systems. Faculty of Civil Engineering, Belgrade, 2(1), 5–21.
Papa, A., Mital, M., Pisano, P., & Del Giudice, M. (2020). E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technological Forecasting and Social Change, 153, 119226.
PwC. (2019). Long-term care Industry Practical Manual quickly grasps Long-term care Industry Information. Retrieved October 29, 2019, from https://www.pwc.tw/zh/publications/topic-bio/long-term-care.html
Qian, S., Yu, P., & Bhattacherjee, A. (2019). Contradictions in information technology mediated work in long-term care: An activity theoretic ethnographic study. International Journal of Nursing Studies, 98, 9–18.
Rad, T. G., Sadeghi-Niaraki, A., Abbasi, A., & Choi, S. M. (2018). A methodological framework for assessment of ubiquitous cities using ANP and DEMATEL methods. Sustainable Cities and Society, 37, 608–618.
Robertson, E. G., Wakefield, C. E., Signorelli, C., Cohn, R. J., Patenaude, A., Foster, C., & Fardell, J. E. (2018). Strategies to facilitate shared decision-making about pediatric oncology clinical trial enrollment: a systematic review. Patient Education and Counseling, 101(7), 1157–1174.
Saaty, T. L. (2001). Decision making with dependence and feedback: the analytic network process. RWS Publisher.
Schipper, L., Luijkx, K., Meijboom, B., & Schols, J. (2015). The 3 A’s of the access process to long-term care for elderly: Providers experiences in a multiple case study in the Netherlands. Health Policy, 119(1), 17–25.
Simic, V., Gokasar, I., Deveci, M., & Isik, M. (2021). Fermatean fuzzy group decision-making based CODAS approach for taxation of public transit investments. IEEE Transactions on Engineering Management. https://doi.org/10.1109/TEM.2021.3109038
Simic, V., Gokasar, I., Deveci, M., & Karakurt, A. (2022). An integrated CRITIC and MABAC based type-2 neutrosophic model for public transportation pricing system selection. Socio-Economic Planning Sciences, 80, 101157.
Snowdon, A. W., & Tallarigo, D. (2018). Leveraging supply chain infrastructure to advance patient safety in community health-care settings. Leadership in Health Services. https://doi.org/10.1108/LHS-03-2018-0017
Teymourifar, A., Kaya, O., & Ozturk, G. (2021). Contracting models for pricing and capacity decisions in healthcare systems. Omega, 100, 102232.
Tian, S., Yang, W., Le Grange, J. M., Wang, P., Huang, W., & Ye, Z. (2019). Smart healthcare: Making medical care more intelligent. Global Health Journal, 3(3), 62–65.
Toms, G., Verity, F., & Orrell, A. (2019). Social care technologies for older people: Evidence for instigating a broader and more inclusive dialogue. Technology in Society, 58, 101111. https://doi.org/10.1016/j.techsoc.2019.01.004
Torkayesh, A. E., Deveci, M., Torkayesh, S. E., & Tirkolaee, E. B. (2021). Analyzing failures in adoption of smart technologies for medical waste management systems: A type-2 neutrosophic-based approach. Environmental Science and Pollution Research, 1–14.
Torkayesh, A. E., & Deveci, M. (2021). A mulTi-noRmalization mUlti-distance aSsessmenT (TRUST) approach for locating a battery swapping station for electric scooters. Sustainable Cities and Society, 74, 103243.
Tsai, W. H., & Kuo, H. C. (2011). Entrepreneurship policy evaluation and decision analysis for SMEs. Expert Systems with Applications, 38(7), 8343–8351.
United Nations. (2019). World population ageing 2019. New York, NY: Department of Economic and Social Affairs, Population Division, United Nations.
Vetsch, J., Wakefield, C. E., Techakesari, P., Warby, M., Ziegler, D. S., O'Brien, T. A., ... & Tucker, K. (2019, June). Healthcare professionals’ attitudes toward cancer precision medicine: A systematic review. In Seminars in Oncology (Vol. 46, No. 3, pp. 291–303). WB Saunders.
Wager, K. A., Lee, F. W., & Glaser, J. P. (2017). Healthcare information systems: A practical approach for health care management. John Wiley & Sons.
Wind, Y., & Saaty, T. L. (1980). Marketing applications of the analytic hierarchy process. Management Science, 26(7), 641–658.
World Health Organization. (2016). Strategizing national health in the 21st century: a handbook. World Health Organization. Retrieved October 29, 2019, from https://apps.who.int/iris/handle/10665/250221
World Health Organization. (2017). Global action plan on the public health response to dementia 2017–2025.
Xu, H., & Intrator, O. (2019). Medicaid Long-term Care Policies and Rates of Nursing Home Successful Discharge to Community. Journal of the American Medical Directors Association. https://doi.org/10.1016/j.jamda.2019.01.153
Yang, C. H., Lee, K. C., & Chen, H. C. (2016). Incorporating carbon footprint with activity-based costing constraints into sustainable public transport infrastructure project decisions. Journal of Cleaner Production, 133, 1154–1166.
Zhao, Y., Liu, L., Qi, Y., Lou, F., Zhang, J., & Ma, W. (2020). Evaluation and design of public health information management system for primary health care units based on medical and health information. Journal of Infection and Public Health, 13(4), 491–496.
Acknowledgements
We would like to thank the Ministry of Science and Technology of Taiwan for financially supporting this research under Grant MOST 108-2410-H-606 -009 -MY2 and MOST 111-2410-H-130 -012 -.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, CH., Chen, YC., Hsu, W. et al. Evaluation of smart long-term care information strategy portfolio decision model: the national healthcare environment in Taiwan. Ann Oper Res 326, 505–536 (2023). https://doi.org/10.1007/s10479-023-05358-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10479-023-05358-7