Abstract
Adverse childhood experiences (ACEs) and financial hardship are associated with increased likelihood of heavier alcohol use and health challenges in adulthood among persons living with HIV (PWH). We examined whether retrospectively captured lifetime drinking trajectories are a pathway through which childhood hardships affect current health in a sample of 365 adult PWH. Childhood economic hardship and ACEs were used as main predictors. Measures of alcohol use included age at first drink and lifetime drinking trajectories. Health indicators included health-related quality of life, frailty, number of comorbidities, and symptoms of anxiety, depression, and post-traumatic stress disorder (PTSD). Structural equation modeling (SEM) was applied to estimate both direct and indirect pathways between childhood hardship and physical and mental health. Participants were mostly male; Black (84%); and averaged 48 years of age. SEM results supported both direct and indirect pathways between childhood experiences and adult health. ACEs were connected to physical health directly and mental health both directly and indirectly through age at first drink and drinking heaviness during ages 10–20. Childhood economic hardship related to mental health indirectly through higher drinking levels during ages 10–20. Childhood adverse experiences, economic hardship, and early drinking patterns appear to accumulate, resulting in later life physical and mental health concerns for PWH. Findings support taking a life course approach to health. This includes considering individual trauma histories in HIV care engagement and taking preventative approaches which support the economic and social well-being of vulnerable children to improve health in subsequent decades.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People living with HIV (PWH) are more likely to have experienced traumatic events, including adverse childhood experiences (ACEs), compared to seronegative individuals [1,2,3,4]. HIV-seropositive individuals are 1.5–2.0 times more likely to have experienced childhood physical or sexual abuse than seronegative populations [2]. In a study of 611 in-care PWH in the southern United States, over 50% had experienced at least one form of physical abuse or neglect prior to age 13 [5]. Childhood adversity includes both the witnessing or experiencing of traumatic events (ACEs) and childhood economic hardship (CEH), a condition where a child’s family struggles financially to cover basic needs such as food and housing. Several studies have shown that childhood adversity not only contributes to the transmission of HIV but is also associated with the progression of the disease, poor quality of life, poor antiretroviral therapy (ART) adherence, increased healthcare utilization, and higher HIV-related and all-cause mortality rates among PWH [1,2,3]. Research indicates that early life exposure to adversities such as poverty, neglect, or abuse is linked to negative health outcomes through changes in social information processing, emotional responses, and biological aging (younger initiation of puberty and cellular aging) [6].
Childhood adversity (ACEs and CEH) is linked to poorer physical and mental health outcomes in adulthood among many PWH [2,3,4, 6,7,8,9,10]. Mental health challenges such as anxiety and depressive symptoms, post-traumatic stress and formally diagnosed PTSD, are linked to early-life trauma [2, 11]. Physical health outcomes associated with ACEs, trauma, and CEH are documented as well. These include elevated rates of sexually transmitted infection (STI) acquisition, obesity, cardiovascular disease, and diabetes [12,13,14]. Experiencing a greater number of ACEs has also been associated with increased risk for binge drinking, tobacco use, intravenous drug use and risky sexual behaviors, such as not using a condom, in adulthood [12].
Increased risk for hazardous drinking among PWH has been documented, with two recent national studies of in-care PWH estimating that 32% (total sample N = 7686) and 26% (total sample N = 9336) screened positive for hazardous alcohol use as assessed by the Alcohol Use Disorders Identification Test (AUDIT-C) [15, 16]. Alcohol use is linked to poorer mental and physical health outcomes and an increased risk for subsequent misuse [17,18,19]. Alcohol consumption is negatively associated with ART adherence, immune function, and reliably demonstrated to accelerate HIV disease progression and chronic comorbidity [20, 21, 22].
When considering the mechanisms that link childhood adversity, hazardous drinking patterns, and health in PWH, it is important to recognize that alcohol use frequently changes across the life course [23]. ACE survivors are shown to initiate alcohol use at an earlier age [24, 25], which can lead to poor health outcomes and health-threatening behaviors [26]. Neurobiological studies have found that exposure to early life trauma and chronic stress alters biological pathways, such as the hypothalamo-pituitary (HPA) axis, glucocorticoid production, and dopaminergic (DA) response, resulting in enhanced dopamine release in response to psychostimulant administration, thus making trauma survivors more vulnerable to addiction [27]. Childhood trauma has not only been related to alcohol initiation but lifetime hazardous drinking and susceptibility to relapse [28]. Research from the New Orleans Alcohol use in HIV (NOAH) Study has found that a steeper increase in alcohol consumption after ages 10–20 was related to worse health-related quality of life, frailty, and current drinking [29]. Other studies using NOAH data have found that higher alcohol use at the time of data collection was related to liver disease, fibrosis, higher caloric and fat intake, and insulin resistance, while lifetime alcohol consumption was related to cardiometabolic risk factors and frailty risk [30,31,32].
Alcohol misuse, particularly as a maladaptive coping technique, is a modifiable health behavior with interventions demonstrating improvements in anxiety, depression, and social functioning [18, 33,34,35]. However, the evidence for effectiveness of interventions on HIV related outcomes (i.e., CD4+, viral load) is inconclusive. [36, 37]). Early-life trauma and ACEs, which are often predicated on childhood poverty [38], are, definitionally, non-modifiable in adulthood. Advancing robust models of trauma-informed, PWH-tailored, recovery from alcohol misuse will require sophisticated understandings of the inherent biopsychosocial dynamics that link ACEs with poorer health in later adulthood. Life course theory (LCT) [39]; alongside broader developmental systems frameworks, emphasizes the socio-environmental circumstances that may underlie age of alcohol initiation and onset of specific problem-drinking (e.g., bingeing) patterns [40, 41], particularly in the context of childhood economic hardship [24, 25, 38, 40]. As such, the aims of the present study were twofold: (1) to examine the associations between childhood adversity (ACEs and CEH), retrospectively captured lifetime drinking patterns and current health among adult in care PWH; and (2) to explore if these identified lifetime drinking patterns might serve as pathways from ACEs to poorer mental and physical health outcomes in PWH.
Methods
Data
These data were collected as part of the NOAH Study, a translational longitudinal study examining the interaction of alcohol use with biological and socio-environmental mechanisms impacting HIV-associated comorbidities, accelerated aging, and disease progression [42]. Adult PWH were recruited from an HIV outpatient clinic and a local federally qualified health center from October 2015 to October 2017. Potential participants were screened using the AUDIT and invited to enroll in the translational longitudinal study. To enroll a sufficiently powered sample to examine the impact of alcohol use on HIV progression comprehensively, respondents with AUDIT scores > 8 were oversampled. We provide a brief description of study recruitment and data collection here; greater detail is provided in a previous publication [42].
Study eligibility included non-pregnant PWH age 18 and older who were without acute illness, including non-prophylaxis prescription of antibiotics, or alcohol intoxication at the study visit. There were no further exclusion criteria. Once informed consent was obtained, participants attended a baseline visit at which data on residential address, alcohol use, physical and mental health, and other health-related factors were collected. Participants also provided blood, stool, vaginal, and saliva samples for analysis of HIV clinical outcomes and health biomarkers, blood pressure, and anthropometric measures. Details on the study protocol, recruitment strategy and measures have been published previously [42]. We used data from baseline interviews as well as medical chart abstraction in the present analysis (N = 365). The parent study was approved by the Louisiana State University Health Science Center (LSUHSC) and Tulane University Institutional Review Boards. All participants provided informed consent.
Measures
Childhood adversity Two measures of childhood social and economic adversity were included in the present study. Adverse childhood experiences (ACE) were measured with the adverse childhood experiences questionnaire from the Kaiser Permanente ACE study [13]. In this questionnaire, persons are asked whether they experienced psychological, physical, or sexual abuse; witnessed violence against their mother/caregiver; or lived with household members who evidenced hazardous patterns of substance use, had a mental illness or were suicidal or were ever imprisoned during their childhood (before age 18). Total ACE score was calculated as the sum of all positive responses (range 0–10), with higher scores representing greater adverse experiences.
Childhood economic hardship was assessed with questions adapted from the U.S. Census Bureau’s Survey of Income and Program Participation (SIPP) [43]. Participants were asked if before age 12, their household was unable to pay the rent/mortgage; experienced eviction; was unable to pay gas, oil, or electricity bills; went hungry because there was not enough money for food; moved in with other people because of financial problems; and whether their family owned their own home (reverse coded). Responses were summed to yield a total score (range 0–6), with higher scores representing greater economic hardship.
Life course alcohol use patterns Patterns of alcohol use across the life course were captured via age at first alcohol use and lifetime drinking trajectories. Alcohol use initiation age was captured with a single question at baseline asking participants at what age they first drank alcohol. Lifetime drinking trajectories were constructed based responses to a modified version of the Lifetime Drinking History questionnaire [44]. This series of questions asks about average quantity (e.g., “When you were 10–20 years old, how much did you drink on a typical day when you were drinking?”) and frequency (e.g., “When you were 10–20 years old, how often did you drink?”) of alcohol consumption during each decade of life, starting with the onset of regular drinking and ending with the individual’s current drinking pattern. Its validity and reliability have been established in several previous studies with heavy and non-heavy drinkers [44, 45,46,47]. For each decade of life, quantity and frequency measures were multiplied to yield average annual number of drinks. These counts were divided by 12 to derive average monthly drinks during each decade, then log-transformed for trajectory analyses due to the right-skewness of the counts. Additional details about how we constructed lifetime drinking trajectories are provided in the “Analysis” section below.
Health status To capture general physical decline, three measures of physical health status that span physiological systems were included. These measures also demonstrated associations with lifetime alcohol use in prior studies with this cohort [29]. Health-related Quality of Life (HRQoL) was measured via responses to the Short Form 36 (SF36) [48]. This 36-item questionnaire measures eight health-related domains. In the present study, general perception of health (five items) was included. The five items were summed then transformed to a 0–100 scale (worst to best possible health state). Frailty was captured by a deficit index constructed from 58 items (DI58). Drawn from a prior study examining cumulative lifetime alcohol volume and frailty among NOAH participants, the deficit index included items that were based on self-report (e.g., “how would you rate your health”), screening tests (e.g., Mini-Mental State Examination), clinical evaluation (e.g., congestive heart failure), as well as laboratory measurement (e.g., diabetes mellitus) [49, 50]. Binary deficits were scored as either 0 or 1, whereas deficits with multiple response levels were evenly graded between 0 and 1. The sum of the health indicators was then divided by the total possible score of 58. Higher scores (possible range 0–1) indicate greater frailty. Lastly, a multi-morbidity index was included to provide an additional measure of co-morbidity in the sample. Multimorbidity is a geriatric syndrome defined as the co-prevalence of aging-associated medical conditions [51]. The NOAH Study Multimorbidity Index (MMI) is the sum of 14 common geriatric comorbidities (heart disease, cancer [excluding HIV malignancies], chronic lower respiratory diseases, stroke (cerebrovascular diseases), diabetes, chronic kidney disease, hypertension, hyperlipidemia, arthritis (any type), affective disorder, dementia, anemia (any etiology), osteoporosis, chronic liver disease) diagnosed in an individual participant.
Similarly, three measures of mental health status were also included. Anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS), a validated and reliable screening tool consisting of 14 items (including 7-item subscales for anxiety and depression) [52, 53]. Though the continuous summary score was used in this analysis, a cut off of eight is considered ‘borderline’ while a cut off of 11 is considered ‘clinical’ for both anxiety and depression subscales [53]. PTSD symptoms were assessed using the Primary Care PTSD Screen (PC-PTSD-5) [54]. This instrument is a revision of the original PC-PTSD reflecting updates to PTSD diagnostic criteria in the DSM-5. The screener includes five yes/no items, summed for a possible score of 0–5. Though the continuous summary score was used in this analysis, a cut off of three is considered ‘borderline’ while four is considered ‘clinical’ [54]. This updated measure has demonstrated excellent diagnostic accuracy [54].
Demographic controls Several demographic control variables were explored, based on their correlation with childhood adversity, lifetime drinking trajectories, and/or health status. We focused on those which would be exogenous to and temporally precede childhood adversities, to avoid controlling for potential mediators. Age was included as a continuous variable, centered at the sample mean. Our past work demonstrated generational differences in lifetime drinking patterns, and health is generally known to decline with age [29]. Sex assigned at birth was included due to known sex differences in alcohol use patterns and health status [55, 56]. Educational attainment and income were also explored as potential confounders. However, these were eventually excluded both due to their non-significant relationships with study variables and due to concerns, that they could be products of childhood adversity and/or lifetime alcohol use patterns.
Analysis
Overall approach We began analyses by generating descriptive statistics for all study variables. We then proceeded to construct the latent variables we would use for structural equation models. Lastly, we estimated the full structural equation model, inclusive of our primary predictors (ACE, childhood economic hardship); lifetime drinking mediators (age at first drink; lifetime drinking trajectory parameters); and our health status outcomes (physical health; mental health). Both direct and indirect paths between the predictors and outcomes were tested.
Latent lifetime alcohol use trajectory parameters Like past analyses [29], we characterized lifetime drinking trajectories applying latent curve modeling in MPlus [57]. Latent curve models are an extension of structural equation models which estimate growth parameters (intercept, slope, quadratic) purged of measurement error [58, 59]. The logged average monthly alcoholic drinks for each decade of life were input as observed indicators of the latent trajectory parameters. Full information maximum likelihood (FIML) estimation was used. The best fitting model was the quadratic model, which included intercept, linear slope, and quadratic (deceleration) parameters. For lifetime drinking history, the intercept represented the average number of drinks in the first decade measured (ages 10–20), the linear term represented the change (slope) in average number of drinks across decades over time, and the quadratic represented the change in slope of average number of drinks over time. However, due to instability of the variance around the quadratic parameter, its variance was set to zero. The intercept and slope were allowed to covary.
Latent mental and physical outcomes Physical and mental health were specified in our model as a pair of correlated latent variables. Indicators for each (physical health: HRQoL, frailty, and multimorbidity; mental health: anxiety, depression, and PTSD symptoms) were standardized to facilitate estimation, given widely different measurement scales. The latent health variables were scaled to have a mean of zero and a variance of one and were allowed to covary.
Structural equation modeling After establishing the fit of the latent components of the model, we proceeded to combine the elements into a comprehensive structural equation model, estimated using robust maximum likelihood. Demographic controls were entered as predictors of childhood hardship variables; lifetime drinking variables; and health status variables. Where associations between demographic variables and other variables were non-significant, demographic controls were trimmed for model parsimony. Final model fit was assessed via various fit indicators used in evaluation of structural equation models (i.e., RMSEA; CFI/TLI; etc.) [60].
Results
Descriptive statistics Descriptive statistics are displayed in Table 1. Participants’ ages ranged from 20 to 71 with a mean of 48.2 (SD = 10.35). Most of the sample identified as Black (83.6%), male (69.0%), had a household income below $20,000 a year (88.74%) and over a third identified as a sexual minority (38.4%). In terms of education, 40.8% had less than a high school education, 31.2% had a high school diploma or GED, 22.2% had some college education, 3.8% had a 4-year college degree, and 1.9% had a graduate or professional degree. Predictors of childhood adversity included childhood economic hardship, which had a mean score of 1.5 (SD = 1.5) on a range of 0–6, and ACE score, which had a mean score of 3.4 (SD = 2.7) on a range of 0–10. The sample population had a mean number of 547.9 (SD = 989.9) drinks per year between ages 10 and 20, which increased to 790.3 (SD = 1167.2) drinks per year between ages 21 and 30. From ages 31 to 40, the mean number of drinks per year was 799.6 (SD = 1182.1), which decreased to 703.0 (SD = 1108.5) from ages 41 to 50, to 554.6 (SD = 936.5) from ages 51 to 60 and finally to 274.2 (SD = 570.0) from ages 61 to 70. A high proportion of respondents had borderline or clinical depression (27.7%), anxiety (42.2%) and/or PTSD (21.15%) compared to prevalence in the general population. For the physical indicators, participants reported an average of 3.12 multi-morbidities (SD = 1.77), had an average frailty score of 0.17 (SD = 0.087) out of 1 and a general perception of health score of 59.4 (SD = 23.3) on a scale of 0 (worst possible health) to 100 (best possible health).
Structural equation modeling results Fit statistics indicated that the model fit the data relatively well (CFI = 0.949, RMSEA = 0.043).
Table 2 details the indirect and total pathways from childhood hardship variables (CEH and ACES) to physical and mental health. Indirect pathways were significant for both economic hardship (β = 0.033; p = 0.029) and ACES (β = 0.009; p = 0.029) for mental health, but not for physical health. Total effects were significant for all four pathways with the largest effect size for ACEs to mental health (β = 0.147; p < 0.001).
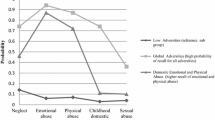
Results of the path analysis are presented in Fig. 1. In this model ACEs were significantly and negatively associated with age at first drink (those with higher ACE scores initiated drinking sooner) (β = − 4.15; p < 0.001). Childhood economic hardship was associated with lifetime drinking history intercept (those with higher childhood economic hardship scores were more likely to engage in heavier drinking between ages 10 and 20) (β = 0.148; p = 0.001). Age at first drink was in turn associated with the lifetime drinking history intercept (β = − 0.098; p < 0.001) and lifetime drinking history linear increase (β = 0.015; p = 0.037). Lifetime drinking history intercept was in turn associated with mental health (β = 0.226; p = 0.003).
Structural equation mediation model. *p < 0.05; **p < 0.01;***p < 0.001; ACE adverse childhood experiences; CEH childhood economic hardship; LDH lifetime drinking history intercept. Purple arrows represent pathways from CEH while green arrows represent pathways from ACEs. Alternating green and purple lines represented shared pathways between ACEs and CEH. Dark solid lines represent significant relationships and lighter dotted lines represent tested for but insignificant relationships (Color figure online)
Discussion
This study explored pathways between childhood adversities (ACEs and CEH), lifetime alcohol use, and mental and physical health outcomes among PWH enrolled in the NOAH study, embracing a lifecourse-informed approach. Our findings revealed that ACES and CEH have a significant impact on both lifetime drinking patterns and current health, particularly mental health, in our study sample. Drinking history early in life (ages 10–20) was a significant mediating factor for the relationship between childhood adversity and mental health with the strongest mediation effects for CEH, indicating the strength of the relationship between childhood poverty, patterns in alcohol use, and mental wellbeing.
These findings build on prior work exploring the detrimental impacts of familial poverty and ACEs on health-related challenges in later adulthood [1,2,3,4,5,6,7,8,9,10,11,12,13,14, 24,25,26]. Prior research has outlined negative health impacts of various forms of ACES and CEH in both domains of mental health (PTSD, depression, etc.) and physical health (cardiovascular health, nutrition, etc.) [2, 6,7,8,9,10,11,12,13,14]. This body of research emphasizes the influence of ACES and CEH on brain development and cognitive processes, highlighting the importance of mental health both as a factor underpinning pathways between adversity and physical health and as an avenue for intervention [3, 6, 9].
We found significant associations between ACEs, CEH and early life alcohol use, with early alcohol use mediating ACEs and CEH’s impact on later life health. Some studies have found connections between ACEs, socioeconomic status, and substance use initiation in adolescent populations [24, 61, 62]. However fewer studies examine drinking frequency trajectories across the life course. Prior work using data from the NOAH study has found that a larger increase in alcohol consumption following ages 10–20 was associated with worse health related quality of life and that high levels of alcohol consumption across the life course was related to cardiometabolic factors and liver functioning [29, 30]. Multiple studies suggest that all but the most severe physical effects of heavy alcohol use in adults including fatty liver, GI tract dysregulation, and myocardial damage are reversible with 4–6 weeks of abstinence from alcohol [63,64,65].
Additionally, though we found mediating effects of drinking trajectories on the pathways between ACES and CEH and health, these mediating effects were strongest for CEH. Recent meta-analytic findings demonstrate consistent, divergent, processes of premature biological aging associated with “deprivation” versus “threat” exposures in childhood, indicating potentially different pathways for CEH (‘deprivation’) and childhood maltreatment (‘threat’) on health [6, 66]. Alcohol use, particularly among PWH reaching older adulthood, may accelerate these processes [67].
More research is needed to explore the long-term impacts of heavy alcohol use on adolescents; however, studies have indicated long-lasting neurodevelopmental changes including elevated neuroinflammation and altered hippocampal neurogenesis, which are related to learning, memory, social and mood functioning, even after reduced use in adulthood [68,69,70]. This may explain why mediating pathways of early life alcohol use were more strongly associated with later life mental health, indicating that recovery for mental health concerns may necessitate further intervention beyond abstinence.
Practice Implications
Our findings suggest that accumulating ACEs during childhood is associated with earlier alcohol initiation, average number of drinks consumed in adolescence, and particularly strong negative impacts to mental health (in addition to their impacts on physical health). As early life history variables were tied to later life health, these findings support lifecourse-informed approach to health and particularly mental health in this population. Through this lens, intervening on alcohol mis/use in the U.S. must consider that alcohol is likely adopted as a maladaptive coping technique in response to early life economic hardship and social-emotional stressors. This chronic stress over the life course can undermine the development of long-term healthy stress responses [41, 71, 72].
Treatment strategies for poor mental health and maladaptive coping frequently focus on adaptive coping skills and behavior change. However, interventions informed by these findings must also acknowledge the broader systemic/structural factors and personal histories which shape the lives of PWH [73]. One example of such an intervention; the Intervention Innovations Team, integrated conceptual model (IIT-ICM), developed by Gwadz et al., incorporated critical race theory, harm reduction, and self-determination theory along with more traditional behavior change intervention components to better serve the complex needs of Black and Latino PWH enrolled in the Heart to Heart 2 project [73]. This approach, which emphasized person-centeredness with an understanding of upstream historical, structural, and systemic factors which occur across the life course was identified to be highly acceptable and lacking in most HIV care settings by Heart to Heart 2 participants [73]. Further, screening for ACEs and trauma history has received increasing attention in the HIV care field due to demonstrated effectiveness in increasing linkage to trauma-informed and wraparound care [74]. In addition to incorporating trauma histories in HIV care, a truly lifecourse-informed approach recognizes the importance of comprehensive multisectoral service systems: (1) “vertically,” or across primary, secondary, and tertiary care; (2) “horizontally” in wraparound coordination with social services such as housing (a common and overwhelming stressor in many in-care PWH [75, 76]); and, (3) “longitudinally,” building continuity of pediatric, adolescent, transition-age, and adult healthcare [77]. Continuity of high-fidelity wraparound pediatric, adolescent, and early adulthood healthcare carries the potential to disrupt multiple harmful health behaviors in youth, including those associated with HIV acquisition [78, 79], early alcohol initiation, and hazardous alcohol-use behaviors within the critical 10–20-year-old developmental span implicated by our findings. Additionally, strengthening the family economically through job training, housing vouchers and assistance may dismantle “toxic” stressors that arise from CEH [71, 80,81,82].
Policy Implications
Though a lifecourse-informed approach encourages early intervention on childhood trauma and economic hardship on a systemic level, interventions remain incumbered by fiscal, bureaucratic [83, 84], and political obstacles [85], particularly across the Gulf South. Louisiana, for example, is mired in family economic hardship: statewide, 18.0% of households earned incomes below the federal poverty line (FPL), and an additional 33.0% could not afford basic costs of living [86, 87] with ~ 140,000 children enduring “deep poverty” (< 50% FPL [88]) prior to the COVID-19 pandemic [89, 90]. Political economy scholars highlight Louisiana policymakers’ refusal to raise the state minimum wage, intersecting with longstanding nationwide lack of paid parental leave, subsidized childcare, and affordable housing [91, 92], as contributing to growing inequality in the state [81, 82]. Viewed through a lifecourse lens, persistent poverty in Louisiana, the structural context driving ACE accumulation, and the lifelong health challenges for PWH result from intentional policymaking [1,2,3,4,5,6,7,8,9,10, 24, 25] that even the most carefully tailored models of individual treatment may only partially ameliorate.
Limitations
This study has several strengths, including a lifecourse-informed approach and the combination of latent curve and structural equation modeling, which allowed us to analyze complex relationships to capture both within-individual variability (e.g., change over time in alcohol use) and between-individual variability (e.g., differences in initial levels of alcohol use) in a path analysis. However, there are several limitations to note. First, measurements were taken using a single survey and ACEs, lifetime economic hardship, and alcohol patterns were captured retrospectively. Concerns about recall bias arise from retrospective surveys around alcohol use, particularly as some research suggests this design underestimates alcohol consumption by at least 30% [93]. However other studies have found that retrospective lifetime drinking history assessments are highly to moderately correlated with prospective measures and with health outcomes in the anticipated direction [44,45,46,47, 94]. Similar concerns regarding retrospective childhood maltreatment measures state that mental health conditions such as depression interfere with recall. However, a recent study found changes in repeat measures of ACE scores to be unrelated to mental health [95]. Secondly, it was necessary to set the variance of the quadratic term to zero due to low variance in the sample, meaning that the quadratic term was held constant over time for everyone. Though fixing the quadratic term to zero can simplify the model, it may also lead to risks for misspecification [96]. Third, physical and mental health were assigned as correlated latent variables. While the measures we chose are commonly studied for both mental and physical health, they are not comprehensive of an individual’s overall physical and mental wellbeing. Lastly, respondents were recruited from HIV clinics, as such the sample represented only in care PWH. This is significant as substance use is known to impact engagement across the continuum of HIV care, therefore our sample population may not fully or accurately represent HIV positive substance users [97].
Conclusion
Our study, providing a LCT informed perspective, adds to the current body of literature on childhood adversity, lifetime alcohol use, and later life mental and physical health outcomes. Respondents in our sample not only reported high levels of ACEs, CEH, depression, anxiety, and PTSD, but also experienced homelessness (52%) and incarceration (64.11%) during their lifetime at high rates, and the majority (88.74%) had household incomes below 20,000 USD a year. This, along with our findings that CEH and ACEs were related to adolescent and young adult alcohol use patterns, which were in turn associated with later life health, suggests a need for interventions which include recognition of the pervasive toll of poverty and trauma in the lives of in-care PWH who use or misuse alcohol [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38, 40]. Along with behavior change interventions, this includes high fidelity wraparound healthcare across the life course [76] and preventative interventions targeted at the emotional and financial well-being of children and families [70, 71, 78, 79]. Ultimately an environment of high poverty and inequity, as is the current climate in Louisiana, undermines attempts by integrated healthcare systems to address trauma in a meaningful way. As such, addressing poverty and systemic issues at the policy level is necessary to address childhood trauma and improve health outcomes for PWH in Louisiana.
Data Availability
Not applicable.
References
Bekele T, Collins EJ, Maunder RG, et al. Childhood adversities and physical and mental health outcomes in adults living with HIV: findings from the Ontario HIV Treatment Network Cohort Study. AIDS Res Treat. 2018;2018:2187232. https://doi.org/10.1155/2018/2187232.
Brezing C, Ferrara M, Freudenreich O. The syndemic illness of HIV and trauma: implications for a trauma-informed model of care. Psychosomatics. 2015;56:107–18. https://doi.org/10.1016/j.psym.2014.10.006.
Pence BW, Mugavero MJ, Carter TJ, et al. Childhood trauma and health outcomes in HIV-infected patients: an exploration of causal pathways. J Acquir Immune Defic Syndr. 2012;59:409–16. https://doi.org/10.1097/QAI.0b013e31824150bb.
Wallace M, Felker-Kantor E, Madkour A, et al. Adverse childhood experiences, smoking and alcohol use, and allostatic load among people living with HIV. AIDS Behav. 2020;24:1653–62. https://doi.org/10.1007/s10461-019-02684-5.
Whetten K, Leserman J, Lowe K, et al. Prevalence of childhood sexual abuse and physical trauma in an HIV-positive sample from the deep south. Am J Public Health. 2006;96:1028–30. https://doi.org/10.2105/AJPH.2005.063263.
McLaughlin KA, Colich NL, Rodman AM, Weissman DG. Mechanisms linking childhood trauma exposure and psychopathology: a transdiagnostic model of risk and resilience. BMC Med. 2020;18(1):96. https://doi.org/10.1186/s12916-020-01561-6.
Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37(3):268–77. https://doi.org/10.1016/s0091-7435(03)00123-3.
Peck AE, Lambert CC, Dobbs GC. Measuring the effects of childhood trauma in HIV primary care. J Nurse Pract. 2021;17:116–8. https://doi.org/10.1016/j.nurpra.2020.08.005.
Clark US, Herrington OD, Hegde RR. Effects of early-life adversities on neuropsychiatric and executive functions in HIV-positive adults. J Int Neuropsychol Soc. 2023;29:68–79. https://doi.org/10.1017/S1355617721001466.
Young-Wolff KC, Sarovar V, Sterling SA, et al. Adverse childhood experiences, mental health, substance use, and HIV-related outcomes among persons with HIV. AIDS Care. 2019;31:1241–9. https://doi.org/10.1080/09540121.2019.1587372.
LeGrand S, Reif S, Sullivan K, Murray K, Barlow ML, Whetten K. A review of recent literature on trauma among individuals living with HIV. Curr HIV/AIDS Rep. 2015;12:397–405. https://doi.org/10.1007/s11904-015-0288-2.
Campbell JA, Walker RJ, Egede LE. Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. Am J Prev Med. 2016;50(3):344–52. https://doi.org/10.1016/j.amepre.2015.07.022.
Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. https://doi.org/10.1016/s0749-3797(98)00017-8.
Lee H, Slack KS, Berger LM, Mather RS, Murray RK. Childhood poverty, adverse childhood experiences, and adult health outcomes. Health Soc Work. 2021;46(3):159–70. https://doi.org/10.1093/hsw/hlab018.
Crane HM, Nance RM, Whitney BM, et al. Drug and alcohol use among people living with HIV in care in the United States by geographic region. AIDS Care. 2021;33:1569–76. https://doi.org/10.1080/09540121.2021.1874274.
Crane HM, Ruderman SA, Whitney BM, et al. Associations between drug and alcohol use, smoking, and frailty among people with HIV across the United States in the current era of antiretroviral treatment. Drug Alcohol Depend. 2022;240: 109649. https://doi.org/10.1016/j.drugalcdep.2022.109649.
Bountress KE, Cusack SE, Sheerin CM, et al. Alcohol consumption, interpersonal trauma, and drinking to cope with trauma-related distress: an auto-regressive, cross-lagged model. Psychol Addict Behav. 2019;33:221–31. https://doi.org/10.1037/adb0000457.
Charlet K, Heinz A. Harm reduction—a systematic review on effects of alcohol reduction on physical and mental symptoms. Addict Biol. 2017;22:1119–59. https://doi.org/10.1111/adb.12414.
María-Ríos CE, Morrow JD. Mechanisms of shared vulnerability to post-traumatic stress disorder and substance use disorders. Front Behav Neurosci. 2020;14:6. https://doi.org/10.3389/fnbeh.2020.00006.
Kelso-Chichetto NE, Plankey M, Abraham AG, et al. Association between alcohol consumption trajectories and clinical profiles among women and men living with HIV. Am J Drug Alcohol Abuse. 2018;44:85–94. https://doi.org/10.1080/00952990.2017.1335317.
Marshall BDL, Tate JP, McGinnis KA, et al. Long-term alcohol use patterns and HIV disease severity. AIDS. 2017;31(9):1313–21. https://doi.org/10.1097/QAD.0000000000001473.
Brief DJ, Bollinger AR, Vielhauer MJ, et al. Understanding the interface of HIV, trauma, post-traumatic stress disorder, and substance use and its implications for health outcomes. AIDS Care. 2004;16:S97–120. https://doi.org/10.1080/09540120412301315259.
Cranford JA, Krentzman AR, Mowbray O, Robinson EAR. Trajectories of alcohol use over time among adults with alcohol dependence. Addict Behav. 2014;39:1006–11. https://doi.org/10.1016/j.addbeh.2014.02.009.
Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38:e1-10. https://doi.org/10.1016/j.jadohealth.2005.06.006.
Chatterjee D, McMorris B, Gower AL, Forster M, Borowsky IW, Eisenberg ME. adverse childhood experiences and early initiation of marijuana and alcohol use: the potential moderating effects of internal assets. Subst Use Misuse. 2018;53:1624–32. https://doi.org/10.1080/10826084.2017.1421224.
Leung JP, Britton A, Bell S. Adverse childhood experiences and alcohol consumption in midlife and early old-age. Alcohol Alcohol. 2016;51:331–8. https://doi.org/10.1093/alcalc/agv125.
Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30. https://doi.org/10.1196/annals.1441.030.
Heffner JL, Blom TJ, Anthenelli RM. Gender differences in trauma history and symptoms as predictors of relapse to alcohol and drug use. Am J Addict. 2011;20:307–11. https://doi.org/10.1111/j.1521-0391.2011.00141.x.
Madkour AS, Felker-Kantor E, Welsh DA, Molina PE, Theall KP, Ferguson T. Lifetime alcohol use trajectories and health status among persons living with HIV (PLWH). J Stud Alcohol Drugs. 2022;83:695–703. https://doi.org/10.15288/jsad.21-00303.
Ferguson TF, Rosen E, Carr R, et al. Associations of liver disease with alcohol use among people living with HIV and the role of hepatitis C: the New Orleans Alcohol Use in HIV Study. Alcohol Alcohol. 2020;55:28–36. https://doi.org/10.1093/alcalc/agz089.
Simon L, Ferguson TF, Vande Stouwe C, et al. Prevalence of insulin resistance in adults living with HIV: implications of alcohol use. AIDS Res Hum Retrovir. 2020;36:742–52. https://doi.org/10.1089/AID.2020.0029.
Rosen EM, Primeaux SD, Simon L, Welsh DA, Molina PE, Ferguson TF. Associations of binge drinking and heavy alcohol use on sugar and fat intake in a cohort of southern people living with HIV. Alcohol Alcohol. 2022;57:226–33. https://doi.org/10.1093/alcalc/agab066.
Smith-Bernardin SM, Suen LW, Barr-Walker J, Cuervo IA, Handley MA. Scoping review of managed alcohol programs. Harm Reduct J. 2022;19:82. https://doi.org/10.1186/s12954-022-00646-0.
Moitra E, Anderson BJ, Herman DS, et al. Examination of using alcohol to cope, depressive symptoms, and perceived social support in persons with HIV and Hepatitis C. AIDS Care. 2020;32:1238–45. https://doi.org/10.1080/09540121.2020.1734177.
Crockett KB, Kalichman SC, Kalichman MO, Cruess DG, Katner HP. Experiences of HIV-related discrimination and consequences for internalised stigma, depression and alcohol use. Psychol Health. 2019;34:796–810. https://doi.org/10.1080/08870446.2019.1572143.
Madhombiro M, Musekiwa A, January J, Chingono A, Abas M, Seedat S. Psychological interventions for alcohol use disorders in people living with HIV/AIDS: a systematic review. Syst Rev. 2019;8:244. https://doi.org/10.1186/s13643-019-1176-4.
Wechsberg WM, Browne FA, Bonner CP, Washio Y, Howard BN, van der Drift I. Current interventions for people living with HIV who use alcohol: why gender matters. Curr HIV/AIDS Rep. 2021;18:351–64. https://doi.org/10.1007/s11904-021-00558-x.
Walsh D, McCartney G, Smith M, Armour G. Relationship between childhood socioeconomic position and adverse childhood experiences (ACEs): a systematic review. J Epidemiol Community Health. 2019;73:1087–93. https://doi.org/10.1136/jech-2019-212738.
Corna LM. A life course perspective on socioeconomic inequalities in health: a critical review of conceptual frameworks. Adv Life Course Res. 2013;18:150–9. https://doi.org/10.1016/j.alcr.2013.01.002.
Cheng TL, Solomon BS. Translating Life Course Theory to clinical practice to address health disparities. Matern Child Health J. 2014;18:389–95. https://doi.org/10.1007/s10995-013-1279-9.
Zucker RA. Alcohol use and the alcohol use disorders: a developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology. New York: Wiley; 2015. p. 620–56.
Welsh DA, Ferguson T, Theall KP, et al. The New Orleans Alcohol Use in HIV Study: launching a translational investigation of the interaction of alcohol use with biological and socioenvironmental risk factors for multimorbidity in people living with HIV. Alcohol Clin Exp Res. 2019;43:704–9. https://doi.org/10.1111/acer.13980.
Bauman K. Direct measures of poverty as indicators of economic need: evidence from The Survey of Income and Program Participation. United States Census Bureau: Working Paper Number POP-WP030. 1998. https://www.census.gov/library/working-papers/1998/demo/POP-twps0030.html. Accessed 6 May 2023.
Skinner HA, Sheu WJ. Reliability of alcohol use indices. The lifetime drinking history and the MAST. J Stud Alcohol. 1982;43:1157–70. https://doi.org/10.15288/jsa.1982.43.1157.
Sobell LC, Sobell MB, Riley DM, et al. The reliability of alcohol abusers’ self-reports of drinking and life events that occurred in the distant past. J Stud Alcohol. 1988;49:225–32. https://doi.org/10.15288/jsa.1988.49.225.
Lemmens PH, Volovics L, De Haan Y. Measurement of lifetime exposure to alcohol: data quality of a self-administered questionnaire and impact on risk assessment. Contemp Drug Probl. 1997;24:581–600. https://doi.org/10.1177/009145099702400308.
Koenig LB, Jacob T, Haber JR. Validity of the lifetime drinking history: a comparison of retrospective and prospective quantity-frequency measures. J Stud Alcohol Drugs. 2009;70:296–303. https://doi.org/10.15288/jsad.2009.70.296.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Maffei VJ, Ferguson TF, Brashear MM, et al. Lifetime alcohol use among persons living with HIV is associated with frailty. AIDS. 2020;34:245–54. https://doi.org/10.1097/QAD.0000000000002426.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A. 2007;62:722–7. https://doi.org/10.1093/gerona/62.7.722.
Guaraldi G, Silva AR, Stentarelli C. Multimorbidity and functional status assessment. Curr Opin HIV AIDS. 2014;9:386–97. https://doi.org/10.1097/COH.0000000000000079.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. https://doi.org/10.1016/s0022-3999(01)00296-3.
Prins A, Bovin MJ, Smolenski DJ, et al. The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31:1206–11. https://doi.org/10.1007/s11606-016-3703-5.
DeVito EE, Weinberger AH, Pang RD, Petersen N, Fagle T, Allen AM. Impulsivity across substance use categories: consideration of sex/gender. Curr Behav Neurosci Rep. 2020;7:109–27. https://doi.org/10.1007/s40473-020-00213-6.
Cavanagh A, Wilson CJ, Kavanagh DJ, Caputi P. Differences in the expression of symptoms in men versus women with depression: a systematic review and meta-analysis. Harv Rev Psychiatry. 2017;25:29–38. https://doi.org/10.1097/HRP.0000000000000128.
Muthén LK, Muthén BO. Mplus user’s guide. 8th ed. Los Angeles: Muthén & Muthén; 1998–2017.
Schulenberg J, Maggs JL. Moving targets: modeling developmental trajectories of adolescent alcohol misuse, individual and peer risk factors, and intervention effects. Appl Dev Sci. 2001. https://doi.org/10.1207/S1532480XADS0504_05.
Duncan DT, Kim B, Al-Ajlouni YA, Callander D. Neighborhood-level structural factors, HIV, and communities of color. In: Ojikutu BO, Stone VE, editors. HIV in US communities of color. Cham: Springer; 2021. p. 147–68.
Kim KH. The relation among fit indexes, power, and sample size in structural equation modeling. Struct Equ Model. 2005;12(3):368–90.
Gomez B, Peh CX, Cheok C, Guo S. Adverse childhood experiences and illicit drug use in adolescents: findings from a national addictions treatment population in Singapore. J Subst Use. 2018;23:86–91. https://doi.org/10.1080/14659891.2017.1348558.
Stein MD, Conti MT, Kenney S, et al. Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug Alcohol Depend. 2017;179:325–9. https://doi.org/10.1016/j.drugalcdep.2017.07.007.
Leclercq S, Matamoros S, Cani PD, Neyrinck AM, Jamar F, Stärkel P, Windey K, Tremaroli V, Bäckhed F, Verbeke K, de Timary P. Intestinal permeability, gut-bacterial dysbiosis, and behavioral markers of alcohol-dependence severity. Proc Natl Acad Sci USA. 2014;111(42):E4485–93.
Leggio L, Lee MR. Treatment of alcohol use disorder in patients with alcoholic liver disease. Am J Med. 2017;130(2):124–34.
Thomes PG, Rasineni K, Saraswathi V, Kharbanda KK, Clemens DL, Sweeney SA, Kubik JL, Donohue TM Jr, Casey CA. Natural recovery by the liver and other organs after chronic alcohol use. Alcohol Res Curr Rev. 2021. https://doi.org/10.35946/arcr.v41.1.05.
Colich NL, Rosen ML, Williams ES, McLaughlin KA. Biological aging in childhood and adolescence following experiences of threat and deprivation: a systematic review and meta-analysis. Psychol Bull. 2020;146:721–64. https://doi.org/10.1037/bul0000270.
Leza L, Siria S, López-Goñi JJ, Fernández-Montalvo J. Adverse childhood experiences (ACEs) and substance use disorder (SUD): a scoping review. Drug Alcohol Depend. 2021;221: 108563. https://doi.org/10.1016/j.drugalcdep.2021.108563.
Bekman NM, Winward JL, Lau LL, Wagner CC, Brown SA. The impact of adolescent binge drinking and sustained abstinence on affective state. Alcohol Clin Exp Res. 2013;37(8):1432–9.
Broadwater MA, Liu W, Crews FT, Spear LP. Persistent loss of hippocampal neurogenesis and increased cell death following adolescent, but not adult, chronic ethanol exposure. Dev Neurosci. 2014;36(3–4):297–305.
Lees B, Meredith LR, Kirkland AE, Bryant BE, Squeglia LM. Effect of alcohol use on the adolescent brain and behavior. Pharmacol Biochem Behav. 2020;192: 172906.
Shern DL, Blanch AK, Steverman SM. Toxic stress, behavioral health, and the next major era in public health. Am J Orthopsychiatry. 2016;86:109–23. https://doi.org/10.1037/ort0000120.
Shonkoff JP, Slopen N, Williams DR. Early childhood adversity, toxic stress, and the impacts of racism on the foundations of health. Annu Rev Public Health. 2021;42:115–34. https://doi.org/10.1146/annurev-publhealth-090419-101940.
Gwadz M, Cluesman SR, Freeman R, et al. Advancing behavioral interventions for African American/Black and Latino persons living with HIV using a new conceptual model that integrates critical race theory, harm reduction, and self-determination theory: a qualitative exploratory study. Int J Equity Health. 2022;21:97. https://doi.org/10.1186/s12939-022-01699-0.
Anand P, Carter B, Bronstein A, et al. 1268. Clinic screening for adverse childhood experiences among persons with HIV: a pilot project. Open Forum Infect Dis. 2019;6:S456. https://doi.org/10.1093/ofid/ofz360.1131.
Gwadz M, Cleland CM, Freeman R, et al. Stopping, starting, and sustaining HIV antiretroviral therapy: a mixed-methods exploration among African American/Black and Latino long-term survivors of HIV in an urban context. BMC Public Health. 2021;21:419. https://doi.org/10.1186/s12889-021-10464-x.
Maulsby C, Enobun B, Batey DS, et al. A mixed-methods exploration of the needs of people living with HIV (PLWH) enrolled in access to care, a national HIV linkage, retention and re-engagement in medical care program. AIDS Behav. 2018;22:819–28. https://doi.org/10.1007/s10461-017-1809-3.
Spratt T. Families with multiple problems: some challenges in identifying and providing services to those experiencing adversities across the life course. J Soc Work. 2010;11:343–57. https://doi.org/10.1177/1468017310379256.
Whitfield THF, Parsons JT, Rendina HJ. Rates of pre-exposure prophylaxis use and discontinuation among a large U.S. national sample of sexual minority men and adolescents. Arch Sex Behav. 2020;49:103–12. https://doi.org/10.1007/s10508-019-01602-z.
Macapagal K, Kraus A, Korpak AK, Jozsa K, Moskowitz DA. PrEP awareness, uptake, barriers, and correlates among adolescents assigned male at birth who have sex with males in the U.S. Arch Sex Behav. 2020;49:113–24. https://doi.org/10.1007/s10508-019-1429-2.
Sheffler JL, Piazza JR, Quinn JM, Sachs-Ericsson NJ, Stanley IH. Adverse childhood experiences and coping strategies: identifying pathways to resiliency in adulthood. Anxiety Stress Coping. 2019;32:594–609. https://doi.org/10.1080/10615806.2019.1638699.
Malti T, Noam GG, Beelmann A, Sommer S. Toward dynamic adaptation of psychological interventions for child and adolescent development and mental health. J Clin Child Adolesc Psychol. 2016;45:827–36. https://doi.org/10.1080/15374416.2016.1239539.
Malhi GS, Das P, Bell E, Mattingly G, Mannie Z. Modelling resilience in adolescence and adversity: a novel framework to inform research and practice. Transl Psychiatry. 2019;9:316. https://doi.org/10.1038/s41398-019-0651-y.
Herd P, Moynihan D. How administrative burdens can harm health. Health Aff. 2020. https://doi.org/10.1377/hpb20200904.405159.
Camillo CA. Understanding the mechanisms of administrative burden through a within-case study of Medicaid expansion implementation. J Behav Public Adm. 2021. https://doi.org/10.30636/jbpa.41.196.
Milat AJ, Bauman A, Redman S. Narrative review of models and success factors for scaling up public health interventions. Implement Sci. 2015;10:113. https://doi.org/10.1186/s13012-015-0301-6.
Jesuit Social Research Institute, Loyola University New Orleans. JustSouth Index 2019. Published November 2020. https://jsri.loyno.edu/sites/loyno.edu.jsri/files/JustSouth%20Index%202019_2.pdf. Accessed 3 May 2023.
Louisiana Association of United Ways. ALICE: the consequences of insufficient household income. Published August 2020. https://www.launitedway.org/alice-report-update-louisiana-released-august-2020. Accessed 10 May 2023.
Butkus N, Donovan J. Louisiana Budget Project. Poverty data should be a wake-up call for Louisiana. Published September 2018. https://www.labudget.org/wp-content/uploads/2018/09/LBP-ACS-analysis-2018-1-1.pdf. Accessed 10 May 2023.
Louisiana Budget Project. Poverty in Louisiana: census 2019. Published September 2020. https://www.labudget.org/wp-content/uploads/2020/09/LBP-Census-2019.pdf. Accessed 3 May 2023.
U.S. Census Bureau. Historical county level poverty estimates tool. Updated October 8, 2021. https://www.census.gov/library/visualizations/time-series/demo/census-poverty-tool.html. Accessed 23 May 2023.
Lewis K. Measure of America, Social Science Research Council. A portrait of Louisiana 2020: human development in an age of uncertainty. Published October 29, 2020. https://measureofamerica.org/louisiana2020. Accessed 10 May 2023.
Florida R. Ranking cities by the new urban crisis. Bloomberg CityLab. Published August 29, 2019. https://www.bloomberg.com/news/articles/2019-08-29/ranking-cities-by-the-new-urban-crisis. Accessed 6 Dec 2023.
Heeb J-L, Gmel G. Measuring alcohol consumption: a comparison of graduated frequency, quantity frequency, and weekly recall diary methods in a general population survey. Addict Behav. 2005;30:403–13. https://doi.org/10.1016/j.addbeh.2004.04.022.
Bell S, Britton A. Reliability of a retrospective decade-based life-course alcohol consumption questionnaire administered in later life. Addiction. 2015;110:1563–73. https://doi.org/10.1111/add.13012.
Frampton NMA, Poole JC, Dobson KS, Pusch D. The effects of adult depression on the recollection of adverse childhood experiences. Child Abuse Negl. 2018;86:45–54. https://doi.org/10.1016/j.chiabu.2018.09.006.
Diallo TMO, Morin AJS, Parker PD. Statistical power of latent growth curve models to detect quadratic growth. Behav Res Methods. 2014;46:357–71. https://doi.org/10.3758/s13428-013-0395-1.
Korthuis PT, Edelman EJ. Substance use and the HIV care continuum: important advances. Addict Sci Clin Pract. 2018;13:13. https://doi.org/10.1186/s13722-018-0114-4.
Acknowledgements
The authors would like to thank the NOAH Study participants for their commitment to participate. The authors acknowledge the investigators and research staff affiliated with the LSUHSC Comprehensive Alcohol-HIV/AIDS Research Center for their scientific contributions, including: Virginia Garrison, Erin Meyaski, Mary Meyaski-Schluter, Dr. Bobby Siggins, Curtis Vande Stouwe, and Dr. Liz Simon. This work was prepared while Aubrey Spriggs Madkour was employed at Tulane University. The opinions expressed in this article are the author’s own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Funding
National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism P60 AA009803.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures were reviewed and approved by the Institutional Review Board of the Louisiana State University Health Sciences Center, New Orleans.
Consent to Participate
All participants provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gasik, R.E., Madkour, A.S., Skeen, S.J. et al. The Impact of Childhood Adversity on Life Course Alcohol Use Patterns and Health Status Among People Living with HIV. AIDS Behav (2024). https://doi.org/10.1007/s10461-024-04368-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s10461-024-04368-1